Abstract
Background
Little is known of the natural history of fundoplication or paraesophageal hernia (PEH) repair in terms of reoperation or the incidence treatment of postsurgical gastroparesis (PSG) in large series. Repeat fundoplications or PEH repairs, as well as pyloroplasty/pyloromyotomy operations, have proven to be effective in the context of PSG or recurrence. In this study, we analyzed the incidences of PSG and risk factors for these revisional surgeries following fundoplication and PEH repair procedures in the state of New York.
Methods
The New York State Planning and Research Cooperative System (NY SPARCS) database was utilized to examine all adult patients who underwent fundoplication or PEH repair for the treatment of GERD between 2005 and 2010. The primary outcome was the incidence of each type of reoperation and the timing of the follow-up procedure/diagnosis of gastroparesis. Generalized linear mixed models were used to examine the risk factors for follow-up procedures/diagnosis.
Results
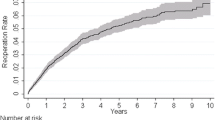
A total of 5656 patients were analyzed, as 3512 (62.1%) patients underwent a primary fundoplication procedure and 2144 (37.9%) patients underwent a primary PEH repair. The majority of subsequent procedures (n = 254, 65.5%) were revisional procedures (revisional fundoplication or PEH repair) following a primary fundoplication. A total of 134 (3.8%) patients who underwent a primary fundoplication later had a diagnosis of gastroparesis or a follow-up procedure to treat gastroparesis, while 95 (4.4%) patients who underwent a primary PEH repair were later diagnosed with gastroparesis or underwent surgical treatment of gastroparesis.
Conclusion
The results revealed low reoperation rates following both fundoplication and PEH repairs, with no significant difference between the two groups. Additionally, PEH repair patients tended to be older and were more likely to have a comorbidity compared to fundoplication patients, particularly in the setting of hypertension, obesity, and fluid and electrolyte disorders. Further research is warranted to better understand these findings.
Similar content being viewed by others
References
Nwokediuko SC (2012) Current trends in the management of gastroesophageal reflux disease: a review. ISRN Gastroenterol 2012:391631. https://doi.org/10.5402/2012/391631
Dent J, El-Serag HB, Wallander M-A, Johansson S (2005) Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 54(5):710–717. https://doi.org/10.1136/gut.2004.051821
DeMeester TR (2017) Surgical options for the treatment of gastroesophageal reflux disease. Gastroenterol Hepatol 13(2):128–129
Lebenthal A, Waterford SD, Fisichella PM (2015) Treatment and controversies in paraesophageal hernia repair. Front Surg 2:13. https://doi.org/10.3389/fsurg.2015.00013
Johansson J, Johnsson F, Joelsson B, Florén C-H, Walther B (1993) Outcome 5 years after 360° fundoplication for gastro-oesophageal reflux disease. Br J Surg 80:46–49. https://doi.org/10.1002/bjs.1800800118
Chang CG, Thackeray L. Laparoscopic hiatal hernia repair in 221 patients: outcomes and experience. JSLS J Soc Laparoendosc Surg. 2016;20(1):e2015.00104. https://doi.org/10.4293/JSLS.2015.00104
Soykan I, Sivri B, Kiernan B, NcCallum RW (1998 Nov) Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci 43(11):2398–2404
Eagon JC, Miedema BW, Kelly KA (1992) Postgastrectomy syndromes. Surg Clin North Am 72:445–465
Shafi MA, Pasricha PJ (2007) Post-surgical and obstructive gastroparesis. Curr Gastroenterol Rep 9:280. https://doi.org/10.1007/s11894-007-0031-2
Obeid NR, Altieri MS, Yang J et al. (2017) Patterns of reoperation after failed fundoplication: an analysis of 9462 patients. Surg Endosc. https://doi.org/10.1007/s00464-017-5682-y
Chen X, Wang Y, Schoenfeld E, Saltz M, Saltz J, Wang F (2017) Spatio-temporal analysis for New York State SPARCS data. In: AMIA summits on translational science proceedings. 2017:483–492
Parkman HP, Fass R, Foxx-Orenstein AE (2010) Treatment of patients with diabetic gastroparesis. Gastroenterol Hepatol 6(6 Suppl 9):1–16
Asena GC, Taylan K, Bülent S, Bülent OY (2013) Effects of l-thyroxine on gastric motility and ghrelin in subclinical hypothyroidism: a prospective study. J Clin Endocrinol Metab 98 (11):E1775–E1779. https://doi.org/10.1210/jc.2013-1488
Zhou T, Harnsberger C, Broderick R et al (2015) Reoperation rates after laparoscopic fundoplication. Surg Endosc 29:510. https://doi.org/10.1007/s00464-014-3660-1
Rathore MA, Andrabi SIH, Bhatti MI, Najfi SMH, McMurray A (2007) Metaanalysis of recurrence after laparoscopic repair of paraesophageal hernia. JSLS J Soc Laparoendosc Surg 11(4):456–460
Latzko M, Borao F, Squillaro A, Mansson J, Barker W, Baker T (2014) Laparoscopic repair of paraesophageal hernias. JSLS J Soc Laparoendosc Surg 18(3):e2014. https://doi.org/10.4293/JSLS.2014.00009. 00009.
Parkman HP, Yates KP, Hasler WL et al (2011) Dietary intake and nutritional deficiencies in patients with diabetic or idiopathic gastroparesis. Gastroenterology 141(2):486–498. e1–e7
Olga Yaylali S, Kirac M, Yilmaz et al (2009) Does hypothyroidism affect gastrointestinal motility? Gastroenterol Res Pract 2009:7. Article ID 529802. https://doi.org/10.1155/2009/529802.
Acknowledgements
We acknowledge the biostatistical consultation and support provided by the Biostatistical Consulting Core at School of Medicine, Stony Brook University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Konstantinos Spaniolas reports grants from Merck, personal fees from Mallickrodt, outside the submitted work. Dr. Aurora D. Pryor reports other from Medtronic, other from Ethicon, other from Stryker, other from Merck, other from Gore, other from Obalon, other from Baranova, outside the submitted work. Mr. Danni Lu, Dr. Maria S. Altieri, Dr. Jie Yang, Ms. Donglei Yin, Dr. Nabeel Obeid, Dr. Mark Talamini have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, D., Altieri, M.S., Yang, J. et al. Investigating rates of reoperation or postsurgical gastroparesis following fundoplication or paraesophageal hernia repair in New York State. Surg Endosc 33, 2886–2894 (2019). https://doi.org/10.1007/s00464-018-6588-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6588-z