Abstract
Background
Recent studies have shown that hospital type impacts patient outcomes, but no studies have examined hospital differences in outcomes for patients undergoing minimally invasive surgery (MIS) for segmental colectomies.
Methods
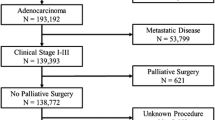
The 2010–2014 National Cancer Data Base was queried for patients undergoing segmental colectomy for non-metastatic colon adenocarcinoma. Descriptive statistics characterized MIS utilization by hospital type. Multivariable models were used to examine the effect of hospital type on outcomes after MIS. Survival probability was plotted using the Kaplan–Meier method.
Results
80,922 patients underwent MIS segmental colectomy for colon cancer from 2010 to 2014. From 2010 to 2014, the number of MIS segmental colectomies increased by 157% at academic hospitals, 151% at comprehensive hospitals, and 153% at community hospitals. Compared to academic hospitals, community and comprehensive hospitals had greater adjusted odds of positive margins (Community OR 1.525, 95% Confidence Interval 1.233–1.885; Comprehensive OR 1.216, 95% CI 1.041–1.42), incomplete number of lymph nodes analyzed (< 12 LNs) from surgery (Community OR 2.15, 95% CI 1.98–2.32; Comprehensive OR 1.42, 95% CI 1.34–1.51), and greater 30-day mortality (Community OR 1.43, 95% CI 1.14–1.78; Comprehensive OR 1.36, 95% CI 1.17–1.59). Patient survival probability was higher at academic hospitals at 5 years (Academic 69% vs. Comprehensive 66% vs. Community 63%, p < 0.001). Community hospitals and comprehensive hospitals had significantly higher risk of adjusted long-term mortality (Community HR 1.28; 95% CI 1.19–1.37; p < 0.001; Comprehensive HR 1.14; 95% CI 1.09–1.20; p < 0.001).
Conclusions
Despite widespread use of laparoscopic oncologic surgery, short- and long-term outcomes from MIS for segmental colectomy are superior at academic hospitals. This difference may be due to superior perioperative oncologic technique and surgical outcomes at academic hospitals. Our data provide important information for patients, referring physicians, and surgeons about the significance of hospital type in management of colon cancer.



Similar content being viewed by others
References
Bonjer HJ et al (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142(3):298–303
Holder-Murray J, Dozois EJ (2011) Minimally invasive surgery for colorectal cancer: past, present, and future. Int J Surg Oncol 2011:490917
Fowler DL, White SA (1991) Laparoscopy-assisted sigmoid resection. Surg Laparosc Endosc 1(3):183–188
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Braga M et al (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236(6):759–766 (Disscussion 767)
Guillou PJ et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Lacy AM et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359(9325):2224–2229
Liang JT et al (2007) Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: a randomized controlled trial. Ann Surg Oncol 14(1):109–117
Milsom JW et al (1998) A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 187(1):46–54 (Discussion 54–55)
Veldkamp R et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Noel JK et al (2007) Minimally invasive colorectal resection outcomes: short-term comparison with open procedures. J Am Coll Surg 204(2):291–307
Weeks JC et al (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287(3):321–328
Schwenk W et al (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 3:CD003145
Kiran RP et al (2010) Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211(2):232–238
Bartels SA et al (2010) Quality of life after laparoscopic and open colorectal surgery: a systematic review. World J Gastroenterol 16(40):5035–5041
Jayne DG et al (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97(11):1638–1645
Kuhry E et al (2008) Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev 34(6):498–504
da Luz Moreira A et al (2010) Laparoscopic versus open colectomy for patients with American Society of Anesthesiology (ASA) classifications 3 and 4: the minimally invasive approach is associated with significantly quicker recovery and reduced costs. Surg Endosc 24(6):1280–1286
Weber WP et al (2007) Impact of surgeon and hospital caseload on the likelihood of performing laparoscopic vs open sigmoid resection for diverticular disease: a study based on 55,949 patients. Arch Surg 142(3):253–259 (Discussion 259)
Alnasser M et al (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28(1):49–57
Moghadamyeghaneh Z et al (2015) Variations in laparoscopic colectomy utilization in the United States. Dis Colon Rectum 58(10):950–956
Roohan PJ et al (1998) Hospital volume differences and five-year survival from breast cancer. Am J Public Health 88(3):454–457
Bach PB et al (2001) The influence of hospital volume on survival after resection for lung cancer. N Engl J Med 345(3):181–188
Fong Y et al (2005) Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg 242(4):540–544 (Discussion 544–547)
Killeen SD et al (2005) Provider volume and outcomes for oncological procedures. Br J Surg 92(4):389–402
Birkmeyer JD et al (2007) Hospital volume and late survival after cancer surgery. Ann Surg 245(5):777–783
Begg CB et al (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280(20):1747–1751
Holm T et al (1997) Influence of hospital- and surgeon-related factors on outcome after treatment of rectal cancer with or without preoperative radiotherapy. Br J Surg 84(5):657–663
American College of Surgeons. National Cancer Data Base. [cited 2016 March 19]; Available from https://www.facs.org/quality%20programs/cancer/ncdb
Bilimoria KY et al (2008) The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol 15(3):683–690
American College of Surgeons. National Cancer Data Base—Data Dictionary PUF 2015 (2017) [cited 2018 4/1/2018]; Available from http://ncdbpuf.facs.org/node/259?q=print-pdf-all
Baxter NN et al (2005) Lymph node evaluation in colorectal cancer patients: a population-based study. J Natl Cancer Inst 97(3):219–225
Bilimoria KY et al (2008) Lymph node evaluation as a colon cancer quality measure: a national hospital report card. J Natl Cancer Inst 100(18):1310–1317
(NCDB), N.C.D.B. Hospital Type or Health Care System. 2016; Available from http://oliver.facs.org/BMPub/help/hcr_09_hosp_typesys.cfm
Burke LG et al (2017) Association between teaching status and mortality in US hospitals. JAMA 317(20):2105–2113
Aquina CT et al (2018) Surgeon, hospital, and geographic variation in minimally invasive colectomy. Ann Surg. https://doi.org/10.1097/SLA.0000000000002694
Tekkis PP et al (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242(1):83–91
Ritchie WP Jr, Rhodes RS, Biester TW (1999) Work loads and practice patterns of general surgeons in the United States, 1995–1997: a report from the American Board of Surgery. Ann Surg 230(4):533–542 (Discussion 542–543)
Dominguez EP et al (2013) Minimally invasive surgery adoption into an established surgical practice: impact of a fellowship-trained colleague. Surg Endosc 27(4):1267–1272
Birch DW, Misra M, Farrokhyar F (2007) The feasibility of introducing advanced minimally invasive surgery into surgical practice. Can J Surg 50(4):256–260
Schrag D et al (2003) Surgeon volume compared to hospital volume as a predictor of outcome following primary colon cancer resection. J Surg Oncol 83(2):68–78 (Discussion 78–79)
Massarotti H et al (2017) Impact of surgeon laparoscopic training and case volume of laparoscopic surgery on conversion during elective laparoscopic colorectal surgery. Colorectal Dis 19(1):76–85
Buurma M et al (2015) Influence of individual surgeon volume on oncological outcome of colorectal cancer surgery. Int J Surg Oncol 2015:464570
Liu CJ et al (2015) Association of surgeon volume and hospital volume with the outcome of patients receiving definitive surgery for colorectal cancer: a nationwide population-based study. Cancer 121(16):2782–2790
Karanicolas PJ et al (2009) The more the better?: the impact of surgeon and hospital volume on in-hospital mortality following colorectal resection. Ann Surg 249(6):954–959
Borowski DW et al (2007) Impact of surgeon volume and specialization on short-term outcomes in colorectal cancer surgery. Br J Surg 94(7):880–889
Rogers SO Jr et al (2006) Relation of surgeon and hospital volume to processes and outcomes of colorectal cancer surgery. Ann Surg 244(6):1003–1011
McGrath DR et al (2005) Surgeon and hospital volume and the management of colorectal cancer patients in Australia. ANZ J Surg 75(10):901–910
Larson DW et al (2008) Surgeon volume does not predict outcomes in the setting of technical credentialing: results from a randomized trial in colon cancer. Ann Surg 248(5):746–750
Ko CY et al (2002) Are high-volume surgeons and hospitals the most important predictors of in-hospital outcome for colon cancer resection? Surgery 132(2):268–273
Waters JA et al (2010) Laparoscopic colectomy: does the learning curve extend beyond colorectal surgery fellowship? JSLS 14(3):325–331
Ross HM et al (2008) Adoption of laparoscopic colectomy: results and implications of ASCRS hands-on course participation. Surg Innov 15(3):179–183
Tsui C, Klein R, Garabrant M (2013) Minimally invasive surgery: national trends in adoption and future directions for hospital strategy. Surg Endosc 27(7):2253–2257
Sheetz KH et al (2017) Provider experience and the comparative safety of laparoscopic and open colectomy. Health Serv Res 52(1):56–73
Damle RN et al (2014) Surgeon volume and elective resection for colon cancer: an analysis of outcomes and use of laparoscopy. J Am Coll Surg 218(6):1223–1230
Lowes M et al (2017) The utilization of multidisciplinary tumor boards (MDT) in clinical routine: results of a health care research study focusing on patients with metastasized colorectal cancer. Int J Colorectal Dis. https://doi.org/10.1007/s00384-017-2871-z
Munro A et al (2015) Do Multidisciplinary Team (MDT) processes influence survival in patients with colorectal cancer? A population-based experience. BMC Cancer 15:686
Bonrath EM et al (2015) Comprehensive surgical coaching enhances surgical skill in the operating room: a randomized controlled trial. Ann Surg 262(2):205–212
Greenberg CC et al (2015) Surgical coaching for individual performance improvement. Ann Surg 261(1):32–34
Nagendran M et al (2013) Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 8:CD006575
Parent RJ et al (2010) Early, intermediate, and late effects of a surgical skills “boot camp” on an objective structured assessment of technical skills: a randomized controlled study. J Am Coll Surg 210(6):984–989
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kyle Freischlag, Mohamed Adam, Megan Turner, Brain Ezekian, Joshua Watson, Paul M. Schroder, Christopher Mantyh, and John Migaly have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Freischlag, K., Adam, M., Turner, M. et al. With widespread adoption of MIS colectomy for colon cancer, does hospital type matter?. Surg Endosc 33, 159–168 (2019). https://doi.org/10.1007/s00464-018-6289-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6289-7