Abstract
Background
The aim of this retrospective study was to assess postoperative quality of life (QOL) after robot-assisted radical transmediastinal esophagectomy, defined as a nontransthoracic esophagectomy with radical mediastinal lymphadenectomy combining a robotic transhiatal approach and a video-assisted cervical approach. The results were compared to those of transthoracic esophagectomy.
Methods
In this study, all consecutive patients who underwent robot-assisted radical transmediastinal esophagectomy or transthoracic esophagectomy for esophageal cancer at University of Tokyo between January 2010 and December 2014 were included. The European Organization for Research and Treatment of Cancer (EORTC)’s quality of life questionnaires QLQ-C30 and QLQ-OES18 were sent to all patients that were still living, had no recurrence or other malignancy, and had not undergone a reoperation because of complications after esophagectomy.
Results
We were able to survey 63 (98.4%) of 64 eligible patients. We assessed and compared the QOL scores of both groups of patients. Compared to transthoracic esophagectomy, transmediastinal esophagectomy was associated with better QOL. Global health status and the physical, role, and cognitive function scale scores were significantly superior in the transmediastinal esophagectomy group (P = 0.004, < 0.0001, 0.007, 0.002, respectively). Fatigue, nausea and vomiting, pain, appetite loss, reflux, and taste scores were significant lower (superior) in the transmediastinal esophagectomy group (P = 0.003, 0.032, 0.025, 0.018, 0.001, 0.041, respectively).
Conclusions
This study indicates that robot-assisted radical transmediastinal esophagectomy is associated with better postoperative QOL compared to transthoracic esophagectomy. A larger study and prospective analyses are needed to confirm the current results.
Similar content being viewed by others
Radical esophagectomy for esophageal cancer is still a challenging surgery because of its high morbidity and mortality [1]. Whereas perioperative mortality rates have fallen to 3.4%, postoperative morbidity rates remain high, at approximately 40% [2]. Progress has been made in minimally invasive esophagectomy for esophageal cancer [3] and a randomized control trial has shown evidence for the short-term benefits of video-assisted thoracoscopic esophagectomy compared with open esophagectomy [4]. However, a recent report on the Japanese national database revealed that minimally invasive esophagectomy increases the rate of surgical complications [2]. Further efforts should be made to reduce the morbidity and mortality of esophagectomy. Transhiatal esophagectomy is also a favored choice, with lower perioperative morbidity, but the oncological outcome of the transhiatal approach is generally considered inferior, since only limited lymph nodes can be harvested when compared to the transthoracic approach [5].
To overcome these shortcomings, we developed transmediastinal esophagectomy, a nontransthoracic esophagectomy with radical mediastinal lymphadenectomy combining a robotic transhiatal approach and a video-assisted cervical approach reported previously by the authors [6]. In our previous study, which compared transmediastinal esophagectomy with conventional transthoracic esophagectomy, we found that postoperative hospital stays were shorter and postoperative pneumonia did not occur in the transmediastinal esophagectomy group [7]. The same study also demonstrated that the radicality of transmediastinal esophagectomy was equivalent to that of transthoracic esophagectomy in terms of the number of harvested lymph nodes and surgical margin pathology [7].
Patients’ quality of life (QOL) after transmediastinal esophagectomy accompanying radical mediastinal dissection was still unknown, however. The object of the present study was to assess postoperative QOL after transmediastinal esophagectomy.
Materials and methods
Patients
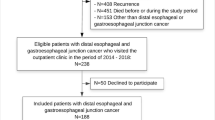
Esophageal cancer patients who underwent transmediastinal esophagectomy or transthoracic esophagectomy with gastric conduit reconstruction via the posterior mediastinal route between January 2010 and December 2014 at the University of Tokyo Hospital were candidates for this study. All these patients were staged preoperatively using esophagogastroduodenoscopy with biopsies and computed tomography scans. Transmediastinal esophagectomy was performed using a robotic surgical system as described in our previous clinical study verifying the safety and utility of robotic transmediastinal esophagectomy [7]. The indications for transthoracic or transmediastinal esophagectomy are (1) histologically proven esophageal cancer, (2) sufficiently good general condition to tolerate conventional open esophagectomy, and (3) a tumor clinically staged as T1-3 N0-1 M0 according to the 7th edition of the American Joint Committee on Cancer tumor-node-metastasis (TNM) classification. In addition, written informed consent to undergo robot-assisted surgery without receiving financial support from the national health insurance system was required for transmediastinal esophagectomy. The QOL survey was performed after excluding those of the above-described patients who met the following exclusion criteria: (1) patients who had a recurrent lesion or who were under treatment for other malignancies; (2) patients who had a history of surgeries of another malignancy; (3) patients who had undergone a reoperation because of complications after esophagectomy. Between January 2010 and December 2014, 128 esophageal cancer patients underwent transthoracic esophagectomy or transmediastinal esophagectomy. Of the 128 patients, 17 patients had died before this study began, 18 patients developed disease recurrence, and 2 patients had a history of reoperation for postoperative complications after esophagectomy. According to the exclusion criteria, consequently, 64 patients, 26 transmediastinal esophagectomy patients, and 38 transthoracic esophagectomy patients, were subjects in the present study, in which we assessed the QOL scores of post-esophagectomy patients and compared the transmediastinal esophagectomy and the transthoracic esophagectomy group scores. This study was approved by The University of Tokyo’s institutional review board. All study participants provided informed consent, and all 64 patients gave their consent.
Surgical methods
The robot-assisted transmediastinal esophagectomy with three-field lymphadenectomy was performed in three stages, all with the patient in the supine position. In the first stage, lymph node dissections in the cervical and the abdominal fields were performed simultaneously by two surgical teams. The cervical procedure was performed via a collar incision under mediastinoscopic guidance. The abdominal procedure was performed via a laparoscopic approach. In the second stage, the robotic surgical device, da Vinci S (Intuitive Surgical, Sunnyvale, CA, USA), was brought in to perform the transhiatal robotic procedure through the abdominal ports. In the dissections consisting of the cervical procedure via the collar incision and the da Vinci procedure via the transhiatal approach, the entire esophagus as well as dissected mediastinal lymph nodes was freed from adhesions and attachments. Upon completion of the mediastinal dissection, the da Vinci S robotic system was moved away from the surgical field. The last stage included the harvest of surgical specimens, reconstruction with a gastric tube conduit, and cervical anastomosis.
Transthoracic esophagectomy patients underwent a right anterolateral thoracotomy via the fourth intercostal space with two- or three-field lymphadenectomy and intrathoracic anastomosis. The creation of the gastric conduit was performed by the same procedure as that performed in the transmediastinal esophagectomy: a gastric conduit with a diameter of 4 cm was created with linear staplers. Pyloroplasty was performed by the same procedure in both transthoracic esophagectomy and transmediastinal esophagectomy. The posterior mediastinal route was used with only one exception, and the anastomosis was performed using a 25-mm circular stapler.
Quality of life measurement
The cross-sectional QOL survey evaluated patients at intervals of more than 3 months since their esophagectomy or the last administration of chemotherapeutic agents from October 2014 to September 2015. Patients who met the above criteria were asked to participate in this study on their regular follow-up visit. The participants were given a self-administered questionnaire and were asked to send it back by mail after filling out the queries.
Patients’ quality of life was assessed using the validated European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire (EORTC QLQ-C30) [8] as well as the esophageal site-specific module (EORTC QLQ-OES18) [9]. The EORTC QLQ-C30 consists of the patient’s global health status, five functional scales (physical, role, emotional, cognitive, and social functioning), three symptom scales (fatigue, pain, and nausea and vomiting) and six single-item measures (dyspnea, insomnia, appetite loss, constipation, diarrhea, financial difficulties). It can assess functional aspects of QOL and symptoms that commonly occur in patients with cancer. The EORTC QLQ-OES18 consists of nine symptom scales (eating, reflux, pain, trouble swallowing saliva, choking when swallowing, dry mouth, trouble with taste, trouble with coughing, and trouble speaking), and was designed to assess patients treated for esophageal cancer by procedures including esophagectomy, chemoradiation, endoscopic palliation, or palliative chemotherapy and/or radiotherapy. High scores in the global health status and the function scales represent a higher level of function and enhanced global health status. On the other hand, higher scores in symptom scales represent more severe symptoms. The reliability and validity of the Japanese version of the EORTC QLQ-C30 and OES-18 have been demonstrated [10, 11].
Statistical analysis
All statistical analyses were performed using JMP 11.0 (SAS Institute Inc. Cary, NC, USA). Wilcoxon’s rank-sum test was used for the analysis of group differences and Fisher’s exact test was used for the proportional differences. A P value less than 0.05 was considered statistically significant.
Results
Esophageal cancer recurred in 14 (15.4%) of the 91 patients in the transthoracic group and in 4 (10.8%) of the 37 patients in the transmediastinal group; there was no significant difference (P = 0.59). Each of the two groups had one patient who had a history of reoperation; there was no significant difference (P = 0.50). There was, however, a significant difference in the current study population in terms of mortality: 16 cases (17.6%) among the 91 patients in the transthoracic group, 1 case (2.7%) among the 37 patients in the transmediastinal group (P = 0.023).
Of the 64 patients meeting the criteria for assessment of QOL, we were able to survey 63 patients (98.4%) using EORTC QLQ-C30 and QLQ-OES18. The patients’ characteristics are shown in Table 1. There were significant differences in clinical and pathological tumor stage between the two groups (P = 0.005, 0.043, respectively). However, there were no significant differences in clinical and pathological lymph node stage, nor were there significant differences in pathological stage between the two groups. Postoperative complications rated greater than Grade 2 by the Clavien–Dindo Classification [12] are shown in Table 2. The diagnosis of postoperative pneumonia was made in accordance with the Japanese Respiratory Society’s Guidelines for Hospital Acquired Pneumonia in Adults [13]. Pneumonia was significantly more frequent (P = 0.008) in the transthoracic group (24.3%) than in the transmediastinal group (0%). Anastomotic leakage was more frequent (though not significantly) (P = 0.707) in the transmediastinal (15.4%) than in the transthoracic group (10.8%). The median time point of assessment from esophagectomy was 23 months (range 6–37) in the transmediastinal group and 24 months (range 3–59) in the transthoracic group (no significant difference).
EORTC QLQ-C30
Table 3 shows the transmediastinal esophagectomy and the transthoracic esophagectomy groups’ postoperative QOL scores measured using EORTC QLQ-C30. The global health status, physical, role, and cognitive function scale scores were significantly higher in the transmediastinal esophagectomy group than in the transthoracic esophagectomy group (P = 0.004, < 0.0001, 0.002, respectively). In the remaining functional scales, no significant differences were found. Fatigue, nausea and vomiting, pain, and appetite loss scores were significantly lower in the transmediastinal esophagectomy group than in the transthoracic esophagectomy group (P = 0.003, 0.032, 0.025, 0.018, respectively). The remaining symptom scales showed no significant differences.
EORTC QLQ-OES18
Table 4 shows the same two groups’ postoperative QOL scores measured using EORTC QLQ-OES18. The reflux and taste scores were significantly lower in the transmediastinal esophagectomy group than in the transthoracic esophagectomy group (P = 0.001, 0.041, respectively). The remaining scales showed no significant differences.
Discussion
We performed transmediastinal esophagectomy using a robotic surgical system to reduce postoperative pulmonary complications after esophagectomy [7]. Our findings suggest that this produces an improvement in the postoperative course and noninferiority in the pathological outcome, but its superiority in the long-term outcome was not investigated in our previous study. To evaluate surgical patients’ postoperative QOL, comparisons have been made between video-assisted thoracoscopic esophagectomy and open transthoracic esophagectomy and between transhiatal esophagectomy and transthoracic esophagectomy. Video-assisted thoracoscopic esophagectomy was found to be superior to open transthoracic esophagectomy in terms of global health status, physical function, fatigue, pain, and dyspnea [14], while transhiatal esophagectomy was superior to open transthoracic esophagectomy in terms of global health status, reflux, and odynophagia [15].
The superiority of QOL in conventional transhiatal esophagectomy may be explained by the reduced lymph dissection along the vagal nerve system; however, the effect on patients’ QOL after transmediastinal esophagectomy accompanying radical mediastinal dissection is still unknown. Dissecting the middle mediastinal lymph nodes such as the parabronchial or paracarinal nodes injures the pulmonary branches of the vagus [16] and such injuries may have negative effects on patients’ QOL. As for the recurrent laryngeal nerve, radical lymph dissections along the nerve may impair the patients’ QOL. The present study aimed to evaluate, using the EORTC questionnaires, the benefit of a robot-assisted radical transmediastinal procedure in terms of postoperative QOL compared to the transthoracic procedure.
Generally, transmediastinal esophagectomy is associated with better QOL scores in many measures. Above all, the reflux scores in QLQ-OES18 have been found to be superior in the transmediastinal esophagectomy group while several studies have found no significant difference in postoperative reflux scores in comparisons between video-assisted thoracoscopic esophagectomy and an open approach [14, 17]. Nonetheless, this finding is concordant with the previous report demonstrating better reflux scores in transhiatal esophagectomy patients than in transthoracic esophagectomy patients [15]. Although there are significant differences in the anastomotic sites—the frequency of the cervical as opposed to the intrathoracic anastomosis being significantly higher in the transmediastinal esophagectomy group than in the transthoracic esophagectomy group—the impact of the anastomotic site on postoperative QOL remains controversial [17,18,19]. Therefore, transmediastinal esophagectomy’s superior reflux scores might be explained not only by the anastomotic site but also by the surgical approach itself.
There are many limitations in our study: there was no assessment of preoperative QOL, and the cross-sectional study design did not enable us to investigate changes in QOL scores within individuals over time. To confirm the superiority of QOL in patients undergoing transmediastinal radical esophagectomy, another prospective study that includes survival analyses with adequate follow-up periods should be conducted. Furthermore, the transthoracic group had a higher proportion of exclusions from this study due to mortality. Although there was no significant difference in the pathological stage between two groups, this difference in mortality might be attributable to a higher frequency of advanced-stage disease in the transthoracic group, which had significantly higher primary tumor status and more (though not significantly) pathological stage III cases. This study can also be criticized for lacking any comparisons with minimally invasive esophagectomy. The improved QOL scores in the transmediastinal group of our current study should be interpreted as being significantly affected by the invasiveness of the transthoracic procedure. Among the QOL scales in the EORTC QLQ-C30 and QLQ-OES18, global health status, the functional scales (physical, role, and cognitive), and the symptom scales (fatigue, nausea and vomiting, pain, appetite loss) in QLQ-C30 might reflect differences between the invasiveness of the approaches, while symptom scales in QLQ-OES18 (reflux and taste) might reflect the better QOL of transmediastinal esophagectomy, as mentioned previously.
In conclusion, this cross-sectional study indicates that robot-assisted radical transmediastinal esophagectomy is associated with better QOL compared to transthoracic esophagectomy. Larger, prospective analyses are needed to confirm these results.
References
Law S (2003) Strategies to improve surgical results in the treatment of esophageal cancer. Esophagus 1(1):49–55
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Sugihara K, Mori M (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Takeuchi H, Kawakubo H, Kitagawa Y (2013) Current status of minimally invasive esophagectomy for patients with esophageal cancer. Gen Thorac Cardiovasc Surg 61(9):513–521
Biere SS a Y, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JHG, Hollmann MW, Lange ESM, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Hulscher J, van Sandick J, Boer A, Wijnhoven B, Tijssen J, Fockens P, Stalmeier P, Ten Kate F, van Dekken H, Obertop H, Tilanus H, van Lanschot J (2002) Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med 347:1662–1669
Mori K, Yamagata Y, Wada I, Shimizu N, Nomura S, Seto Y (2013) Robotic-assisted totally transhiatal lymphadenectomy in the middle mediastinum for esophageal cancer. J Robot Surg 7:385–387
Mori K, Yamagata Y, Aikou S, Nishida M, Kiyokawa T, Yagi K, Yamashita H, Nomura S, Seto Y (2015) Short-term outcomes of robotic radical esophagectomy for esophageal cancer by a nontransthoracic approach compared with conventional transthoracic surgery. Dis Esophagus. https://doi.org/10.1111/dote.12345
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez N, Flilberti A, Flechtner H, Fleishman S, Haes J, Kaasa S, Klee M, Osoba D, Razavi D, Rofe P, Schraub S, Sneeuw K, Sullivan M, Takeda F (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 5:365–376
Blazeby J, Conroy T, Hammerlid E, Fayers P, Sezer O, Koller M, Arraras J, Bottomley A, Vickery CW, Etienne PL, Alderson D (2003) Clinical and psychometric validation of an EORTC questionnaire module, the EORTC QLQ-OES18, to assess quality of life in patients with oesophageal cancer. Eur J Cancer 39:1384–1394
Kobayashi K, Takeda F, Teramukai S, Gotoh I, Sakai H, Yoneda S, Noguchi Y, Ogasawara H, Yoshida K (1998) A cross-validation of the European Organization for Research and Treatment of Cancer QLQ-C30 (EORTC QLQ-C30) for Japanese with lung cancer. Eur J Cancer 34:810–815
Fujita T, Okada N, Sato T, Mayanagi S, Kanamori J, Daiko H (2016) Translation, validation of the EORTC esophageal cancer quality-of-life questionnaire for Japanese with esophageal squamous cell carcinoma: analysis in thoraco-laparoscopic esophagectomy versus open esophagectomy. Jpn J Clin Oncol 46:174–177
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications. Ann Surg 240:205–213
Japanese Respiratory Society (2009) Definition of hospital-acquired pneumonia and characteristics of guidelines in Japan. Respirology 14:3–5
Wang H, Feng M, Tan L, Wang Q (2010) Comparison of the short-term quality of life in patients with esophageal cancer after subtotal esophagectomy via video-assisted thoracoscopic or open surgery. Dis Esophagus 23:408–414
Akkerman RDL, Haverkamp L, van Rossum PSN, van Hillegersberg R, Ruurda JP (2015) Long-term quality of life after oesophagectomy with gastric conduit interposition for cancer. Eur J Cancer 51:1538–1545
Weijs TJ, Ruurda JP, Luyer MDP, Nieuwenhuijzen GAP, Van Hillegersberg R, Blays RL (2015) Topography and extent of pulmonary vagus nerve supply with respect to transthoracic oesophagectomy. J Anat 227:431–439
Zeng J, Liu JS (2012) Quality of life after three kinds of esophagectomy for cancer. World J Gastroenterol 18:5106–5113
Schmidt C, Bestmann B, Kuchler T, Phil D, Schmid A, Kremer B (2004) Quality of life associated with surgery for esophageal cancer: differences between collar and intrathoracic anastomoses. World J Surg 28:355–360
Wormald JCR, Bennett J, van Leuven M, Lewis MPN (2014) Does the site of anastomosis for esophagectomy affect long-term quality of life? Dis Esophagus. https://doi.org/10.1111/dote.12301
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The contributions of the authors to this study are as described here: Shuntaro Yoshimura, Kazuhiko Mori, and Yasuyuki Seto are the authors mainly responsible for the study’s conception and design, acquisition of data, and analysis and interpretation of data. Yukinori Yamagata, Susumu Aikou, Koichi Yagi, Masato Nishida, Hiroharu Yamashita, and Sachiyo Nomura contributed mainly to the drafting of the article and to revising it critically for important intellectual content. Yasuyuki Seto contributed most importantly by giving final approval to the version to be submitted and revised versions to be published. Drs. Shuntaro Yoshimura, Kazuhiko Mori, Yukinori Yamagata, Susumu Aikou, Koichi Yagi, Masato Nishida, Hiroharu Yamashita, Sachiyo Nomura, and Yasuyuki Seto have no conflicts of interest or financial ties to disclose.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Yoshimura, S., Mori, K., Yamagata, Y. et al. Quality of life after robot-assisted transmediastinal radical surgery for esophageal cancer. Surg Endosc 32, 2249–2254 (2018). https://doi.org/10.1007/s00464-017-5918-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5918-x