Abstract
Background
Laparoscopic operations have become longer and more complex and applied to a broader patient population in the last decades. Prolonged gynecological laparoscopic surgeries require prolonged pneumoperitoneum and Trendelenburg position, which can influence respiratory dynamics and other measurements of pulmonary function. We investigated the differences between volume-controlled ventilation (VCV) and pressure-controlled ventilation (PCV) and tried to determine the more efficient ventilation mode during prolonged pneumoperitoneum in gynecological laparoscopy.
Methods
Twenty-six patients scheduled for laparoscopic radical hysterectomy combined with or without laparoscopic pelvic lymphadenectomy were randomly allocated to be ventilated by either VCV or PCV. Standard anesthesic management and laparoscopic procedures were performed. Measurements of respiratory and hemodynamic dynamics were obtained after induction of anesthesia, at 10, 30, 60, and 120 min after establishing pneumoperitoneum, and at 10 min after return to supine lithotomy position and removal of carbon dioxide. The logistic regression model was applied to predict the corresponding critical value of duration of pneumoperitoneum when the Ppeak was higher than 40 cmH2O.
Results
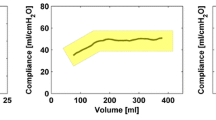
Prolonged pneumoperitoneum and Trendelenburg position produced significant and clinically relevant changes in dynamic compliance and respiratory mechanics in anesthetized patients under PCV and VCV ventilation. Patients under PCV ventilation had a similar increase of dead space/tidal volume ratio, but had a lower Ppeak increase compared with those under VCV ventilation. The critical value of duration of pneumoperitoneum was predicted to be 355 min under VCV ventilation, corresponding to the risk of Ppeak higher than 40 cmH2O.
Conclusions
Both VCV and PCV can be safely applied to prolonged gynecological laparoscopic surgery. However, PCV may become the better choice of ventilation after ruling out of other reasons for Ppeak increasing.





Similar content being viewed by others
References
Neira VM, Kovesi T, Guerra L et al (2015) The impact of pneumoperitoneum and Trendelenburg positioning on respiratory system mechanics during laparoscopic pelvic surgery in children: a prospective observational study. Can Anaesth Soc J 62(7):798–806
Suh MK, Seong KW, Jung SH et al (2010) The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol 59(5):329–334
Balick-Weber CC, Nicolas P, Hedreville-Montout M, Blanchet P, Stéphan F (2007) Respiratory and haemodynamic effects of volume-controlled vs pressure-controlled ventilation during laparoscopy: a cross-over study with echocardiographic assessment. Br J Anaesth 99:429–435
Choi EM, Na S, Choi SH et al (2011) Comparison of volume-controlled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth 23(3):183–188
Campbell RS, Davis BR (2002) Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care 47:416–424
Fahy BG, Barnas GM, Nagle SE et al (1996) Effects of Trendelenburg and reverse Trendelenburg postures on lung and chest wall mechanics. J Clin Anesth 8:236–244
Tweed WA, Phua WT, Chong KY et al (1991) Large tidal volume ventilation improves pulmonary gas exchange during lower abdominal surgery in Trendelenburg’s position. Can J Anaesth 38:989–995
Takahata O, Kunisawa T, Nagashima M et al (2007) Effect of age on pulmonary gas exchange during laparoscopy in the Trendelenburg lithotomy position. Acta Anaesthesiol Scand 51(6):687–692
Nguyen NT, Anderson JT, Budd M et al (2004) Effects of pneumoperitoneum on intraoperative pulmonary mechanics and gas exchange during laparoscopic gastric bypass. Surg Endosc 18(1):64–71
Hardman JG, Aitkenhead AR (2003) Estimating alveolar dead space from the arterial to end-tidal CO2 gradient: a modeling analysis. Anesth Analg 97:1846–1851
Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D (2008) Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth 100:709–716
De Baerdemaeker LE, Van der HC, Gillardin JM et al (2008) Comparison of volume-controlled and pressure-controlled ventilation during laparoscopic gastric banding in morbidly obese patients. Obes Surg 18:680–685
Sun MTA, Shi CL (2002) Recent advances in the clinical application of heart-lung interactions. Curr Opin Crit Care 8(1):26–31
Sizlan A, Karaşahin E, Coşar A et al (2010) Pressure-Controlled vs Volume-Controlled Ventilation During Laparoscopic Gynecological Surgery. J Minim Invasive Gynecol 17(3):295–300
Salihoglu Z, Demiroluk S, Cakmakkaya S, Gorgun E, Kose Y (2002) Influence of the patient positioning on respiratory mechanics during pneumoperitoneum. Middle East J Anesthesiol 16:521–528
Mäkinen MT, Yli-Hankala A (1996) The effect of laparoscopic cholecystectomy on respiratory compliance as determined by continuous spirometry. J Clin Anesth 8:119–122
Bardoczky GI, Engelman E, Levarlet M et al (1993) Ventilatory effects of pneumoperitoneum monitored with continuous spirometry. Anaesthesia 48(4):309–311
Nyarwaya JB, Mazoit JX, Samii K (1994) Are pulse oximetry and end-tidal carbon dioxide tension monitoring reliable during laparoscopic surgery? Anaesthesia 49:775–778
Yamanaka MK, Sue DY (1987) Comparison of arterial-end-tidal PCO2 difference and dead space/tidal volume ratio in respiratory failure. Chest 92:832–835
Subrata S, Donn SM (2007) In support of pressure support. Clin Perinatol 34(1):117–128
Meininger D, Zwissler B, Byhahn C, Probst M, Westphal K, Bremerich DH (2006) Impact of overweight and pneumoperitoneum on hemodynamics and oxygenation during prolonged laparoscopic surgery. World J Surg 30:520–526
Dreyfuss D, Saumon G (2014) Ventilator-induced Lung Injury. N Engl J Med 370(10):979–980
Acknowledgments
This study was supported by the research project of the Key Discipline and Specialty in the Department of Anesthesiology of Shanghai General Hospital (Project Number 040526).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Ming Lian, Xiao Zhao, Hong Wang, Lianhua Chen, and Shitong Li have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Lian, M., Zhao, X., Wang, H. et al. Respiratory dynamics and dead space to tidal volume ratio of volume-controlled versus pressure-controlled ventilation during prolonged gynecological laparoscopic surgery. Surg Endosc 31, 3605–3613 (2017). https://doi.org/10.1007/s00464-016-5392-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5392-x