Abstract
Background
Compared to end-to-side anastomosis with a circular stapler, the overlap method is favored for intracorporeal esophagojejunostomy because it facilitates handling of the stapler, even in narrow spaces, and wider anastomosis. However, it associates with technical difficulties during anastomosis, including difficult traction on the esophageal stump that necessitates stay sutures. Here, we introduce a new modified overlap method that employs knotless barbed sutures (MOBS) and report the outcomes of our case series.
Method
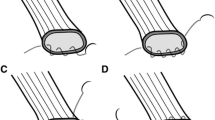
All consecutive patients who underwent intracorporeal esophagojejunostomy in 2015–2016 were included. All patients underwent surgery as follows: After esophageal transection with a linear stapler, two V-loc 90 sutures (Covidien, Mansfield, MA, USA) were sutured in the center of the stapled line. The opening was made between the two threads, and the intraluminal space was identified. The jejunum was ascended toward the esophageal stump by inserting a 45-mm-long linear staple. The anastomosis was made at the space between the right and left crura. After firing the linear stapler, the entry hole was closed bidirectionally using the pre-sutured threads.
Results
Forty patients underwent MOBS (27 by laparoscopy; 13 by robot). Mean total operative and MOBS procedural times were 180.6 and 22.4 min, respectively. Mean hospital stay was 6.9 days. Two patients had major complications (5.0 %). There were no anastomosis-related complications. Laparoscopy and robot subgroups did not differ in mean MOBS procedural times (22.2 vs. 22.7 min, p = 0.787).
Conclusion
MOBS is a safe and feasible method that is a good option for intracorporeal esophagojejunostomy after laparoscopic gastrectomy.





Similar content being viewed by others
References
Hur H, Han SU (2013) Totally laparoscopic surgery for gastric cancer. J Gastric Cancer 13:1–2
Woo J, Lee JH, Shim KN, Jung HK, Lee HM, Lee HK (2015) Does the difference of invasiveness between totally laparoscopic distal gastrectomy and laparoscopy-assisted distal gastrectomy lead to a difference in early surgical outcomes? A prospective randomized trial. Ann Surg Oncol 22:1836–1843
Zhang YX, Wu YJ, Lu GW, Xia MM (2015) Systematic review and meta-analysis of totally laparoscopic versus laparoscopic assisted distal gastrectomy for gastric cancer. World J Surg Oncol 13:116
Kim MG, Kim KC, Kim BS, Kim TH, Kim HS, Yook JH, Kim BS (2011) A totally laparoscopic distal gastrectomy can be an effective way of performing laparoscopic gastrectomy in obese patients (body mass index ≥30). World J Surg 35:1327–1332
Lee JH, Ahn SH, Park DJ, Kim HH, Lee HJ, Yang HK (2012) Laparoscopic total gastrectomy with D2 lymphadenectomy for advanced gastric cancer. World J Surg 36:2394–2399
Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I (2010) Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 211:e25–e29
Umemura A, Koeda K, Sasaki A, Fujuwara H, Kimura Y, Iwaya T, Akiyama Y, Wakabayashi G (2015) Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg 38:102–112
Oh DK, Hur H, Kim JY, Han SU, Cho YK (2010) V-shaped liver retraction during a laparoscopic gastrectomy for gastric cancer. J Gastric Cancer 10:133–136
Azagra JS, Goergen M, De Simone P, Ibanez-Aguirre J (1999) Minimally invasive surgery for gastric cancer. Surg Endosc 13:351–357
Chen K, Pan Y, Cai JQ, Wu D, Yan JF, Chen DW, Yu HM, Wang XF (2016) Totally laparoscopic versus laparoscopic-assisted total gastrectomy for upper and middle gastric cancer: a single-unit experience of 253 cases with meta-analysis. World J Surg Oncol. doi:10.1186/s12957-016-0860-2
Morimoto M, Kitagami H, Hayakawa T, Tanaka M, Matsuo Y, Takeyama H (2014) The overlap method is a safe and feasible for esophagojejunostomy after laparoscopic-assisted total gastrectomy. World J Surg Oncol. doi:10.1186/1477-7819-12-392
Kitagami H, Morimoto M, Nakamura K, Watanabe T, Kurashima Y, Nonoyama K, Watanabe K, Fujihata S, Yasuda A, Yamamoto M, Shimizu Y, Tanaka M (2015) Technique of Roux-en-Y reconstruction using overlap method after laparoscopic total gastrectomy for gastric cancer: 100 consecutively successful cases. Surg Endosc. doi:10.1007/s00464-015-4724-6
Nagai E, Ohuchida K, Nakata K, Miyasaka Y, Maeyama R, Toma H, Shimizu S, Tanaka M (2013) Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery 153:732–738
Acknowledgments
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (1320270). The funding source had no role in the design of this article and will not have any role during its execution or publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Sang-Yong Son, Long-Hai Cui, Ho-Jung Shin, Cheulsu Byun, Hoon Hur, Sang-Uk Han, Yong Kwan Cho have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Son, SY., Cui, LH., Shin, HJ. et al. Modified overlap method using knotless barbed sutures (MOBS) for intracorporeal esophagojejunostomy after totally laparoscopic gastrectomy. Surg Endosc 31, 2697–2704 (2017). https://doi.org/10.1007/s00464-016-5269-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5269-z