Abstract
Background
Respiratory functions are usually impaired during pneumoperitoneum for laparoscopic surgery. This randomized, controlled and single-blinded study was performed to evaluate whether intraoperative protective lung ventilation influences postoperative pulmonary complications after laparoscopic hepatobiliary surgery.
Methods
Sixty-two patients were randomized to receive either conventional ventilation with alveolar recruitment maneuver (tidal volume of 10 ml/kg with inspiratory pressure of 40 cmH2O for 30 s after the end of pneumoperitoneum, group R), or protective lung ventilation (low tidal volume of 6 ml/kg with positive end-expiratory pressure [PEEP] of 5 cmH2O, group P). Induction and maintenance of anesthesia were done with balanced anesthesia. Respiratory complications such as atelectasis, pneumonia or desaturation were observed postoperatively. The length of hospital stay, arterial blood gas analysis, peak inspiratory pressure and hemodynamic variables were also recorded. Results are presented as mean ± SD or number of patients (%).
Results
Postoperative pulmonary complications (P = 0.023) and desaturation below 90 % (P = 0.016) occurred less frequently in group P than in group R. Eight patients of group R and 3 patients of group P showed atelectasis. Pneumonia was diagnosed in 1 patient of group R. No differences were observed in the length of hospital stay, arterial blood gas analysis (pH, PaO2, PaCO2 and PAO2) and hemodynamic variables except PAO2, AaDO2 and peak inspiratory pressure between the two groups.
Conclusion
Protective lung ventilation (low tidal volume with PEEP) during pneumoperitoneum was associated with less incidences of pulmonary complications than conventional ventilation with alveolar recruitment maneuver after laparoscopic hepatobiliary surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopy is a routinely performed approach for many surgical procedures due to reduction in postoperative complications and recovery profiles [1]. However, respiratory function is impaired in patients with laparoscopic surgery under general anesthesia. This has been attributed to the formation of atelectasis and ventilation/perfusion mismatch by the combined effects of supine position and muscle paralysis [2, 3]. In addition, pneumoperitoneum (PnP) with carbon dioxide (CO2) during laparoscopy causes cephalad displacement of the diaphragm and accelerates atelectasis formation [4]. Induced PnP also causes decrease in respiratory compliance and arterial oxygenation [5, 6]. These effects may lead to postoperative pulmonary complications and prolonged hospital stay.
Various ventilatory strategies including positive end-expiratory pressure (PEEP), reverse Trendelenburg position and alveolar recruitment maneuver (ARM) have been introduced to improve gas exchange during surgery [7]. Among intraoperative ventilatory strategies, ARM using inspiratory pressure of 40 cm H2O sustained for 15 s followed by PEEP of 8 cmH2O has been shown to improve intraoperative arterial oxygenation in patients undergoing pelviscopic gynecologic surgery [8]. Additionally, PEEP of 5 cmH2O during PnP has been investigated to attenuate the fall in the partial pressure of arterial oxygen (PaO2) [4].
Protective lung ventilation (PLV) consists of low tidal volume with PEEP to prevent alveolar collapse at end-expiration, which was shown to improve outcome in critically ill patients with acute respiratory distress syndrome [7]. To the best of our knowledge, however, there has been little evidence regarding a potential beneficial effect of PLV during surgery, especially in patients with healthy lungs. In addition, the effectiveness of PLV strategies on the postoperative pulmonary complications has not been demonstrated in patients undergoing laparoscopic surgery. Therefore, we set out this prospective, randomized and controlled study to compare the effect of intraoperative conventional ventilation (combined with ARM) with PLV strategy on postoperative respiratory complications and intraoperative respiratory parameters in patients undergoing laparoscopic hepatobiliary surgery under general anesthesia.
Materials and methods
Patients
After approval with Institutional Review Board of Seoul National University Bundang Hospital (B-1211/180-010) and registration at http://cris.nih.go.kr (registration number KCT0001034), written informed consent to participate in this randomized controlled study was given. Sixty-two, 18–70 aged patients with American Society of Anesthesiologists (ASA) physical class I–II undergoing elective laparoscopic hepatobiliary surgery under general anesthesia from November 2012 to June 2014 were recruited in this prospective, randomized and controlled trial. Patients with cardiopulmonary or hepatorenal disease, recent infections, recent ventilator support, previous thromboembolic disease or denial of informed consent were excluded from the study.
Anesthesia
Patients were premedicated with midazolam 0.03 mg/kg at the reception area of the operating room. Standard monitoring including electrocardiography, SpO2 and noninvasive blood pressure was used. Anesthetic induction was achieved with a bolus dose of propofol 2 mg/kg, an infusion of remifentanil 3 ng/ml with target controlled infusion (TCI) Orchestra® infusion pump system (Fresenius vial, Brezins, France) and desflurane. Intubation was facilitated with rocuronium 0.6 mg/kg and additional dose of rocuronium 0.15 mg/kg as needed to keep a single twitch on the train-of-four stimulation of the ulnar nerve (TOF-Watch SX; Organon Ltd., Dublin, Ireland). After induction of anesthesia, a 20-gauge radial arterial catheter was inserted. Maintenance of anesthesia was provided with desflurane and the continuous infusion of remifentanil (2–4 ng/ml). Bispectral Index™ (BIS) monitor (A-2000 BISTM monitor, Aspect® Medical systems Inc., Natick, MA, USA) was attached to monitor anesthetic depth and monitored throughout the operation. The BIS value was maintained between 40 and 60. At the end of surgery, the patient-controlled analgesia (PCA, 12 μg/ml fentanyl, total 100 ml) programmed to run with a 2-ml bolus dose, and a 10-min lockout time was connected to the patient. Patients were extubated after they were fully recovered and awakened and then transferred to the post-anesthesia care unit (PACU).
Randomization and intervention
Randomization was performed before the induction of anesthesia by an anesthesiologist not otherwise involved in the study. A computer-generated random number table (Random Allocation Software, version 1.0®, Isfahan University of Medical Sciences, Isfahan, Iran) with block size 4 was used. From a table of random numbers, patients were allocated to conventional ventilation with ARM (R group, n = 31) or PLV strategy group (P group, n = 31). Patients and outcome assessors were blinded to the group assignment. However, the anesthesiologist responsible for ventilator setting and the care of the patients during surgery was not blinded to the assigned group.
In all groups, the ventilator mode used was volume-controlled ventilation, inspiration to expiration ratio of 1:2 and a fraction of inspired oxygen (FiO2) of 0.5 in the medical air. These ventilator parameters were maintained throughout the study, and the end-tidal CO2 was kept between 35 and 40 mmHg by adjusting the respiratory rate, whenever necessary. In group R patients, ventilation was performed with tidal volume of 10 ml/kg (ideal body weight) and received ARM just after the end of PnP. The ARM was performed using sustained inspiratory pressure of 40 cmH2O for 30 s applied [9]. Patients with Group P received tidal volume of 6 ml/kg (ideal body weight) with PEEP of 5 cm H2O till the end of surgery (Fig. 1).
Pneumoperitoneum (PnP) was achieved by introduction of a Veress needle at the umbilicus and CO2 insufflation (Wolf Company, Knittlingen, Germany). The intraabdominal pressure was maintained between 11 and 13 mmHg during surgery. Patients’ position was changed with 30° reverse Trendelenburg and 20° left lateral tilt to improve surgical access. Auscultation of both lung fields was performed to rule out one-lung ventilation during PnP [10].
Outcomes
The primary outcome of this study was the incidence of postoperative pulmonary complications including atelectasis, pneumonia or pulmonary edema. The definition of atelectasis was the collapse of a part of the lung presented with a linear increase density on chest images [11]. All patients have preoperative chest images as one of the preoperative evaluations. Postoperative chest images were compared to the preoperative ones and interpreted by the blinded radiologist at immediately after operation, 1 and 2 days after surgery.
Secondary outcomes were the incidence of postoperative desaturation (SpO2 < 90 %), respiratory parameters (PaO2, AaDO2, PAO2, PaCO2, arterial pH, and peak inspiratory pressure [PIP]), hemodynamic variables (mean arterial pressure [MAP] and heart rate [HR]) and the length of hospital stay. Pulse oximetry was monitored continuously until discharge from PACU. Arterial blood gas analysis (ABGA) was performed at the following time intervals: before the induction of PnP, 10 min after PnP formation, right before the end of PnP and at the end of surgery. Patients were evaluated every 15 min using the modified Aldrete scoring system [12] until ready for discharge from the PACU. Modified Aldrete score system includes oxygenation, respiration, circulation, consciousness and activity [12], and the criterion used for patient discharge was the achievement of a modified Aldrete score of 9. Patients were provided O2 at discharge from PACU if SpO2 was less than 90 % without oxygen.
Statistical analysis
Sample size calculation was based on the incidence of atelectasis after laparoscopic surgery using G* power 3.0 (Dusseldorf, Germany). The previous study reported that the incidence of atelectasis after laparoscopic cholecystectomy was 30 % [13]. The reduction of the incidence by 90 % (30–3 %) was considered to be significant, and 26 patients per group were calculated using an alpha value of 0.05 and power of 80 %. Thirty-one patients per group were determined as the final sample size, considering 20 % drop-out rate.
Statistical analysis was performed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA). Normality of data distribution was assessed with the Shapiro–Wilk test. Continuous variables (age, height, weight, BMI, tidal volume, preoperative hemoglobin, PnP duration, operation time, anesthesia time and pain NRS) were analyzed with t test or Mann–Whitney test. The Chi-square test or Fisher’s exact test was used to compare incidences variables (postoperative pulmonary complications including atelectasis, pneumonia, or desaturation). Repeated-measures analysis of variance (ANOVA) was used to analyze changes in respiratory parameters (PaO2, AaDO2, PAO2, PaCO2, arterial pH, PIP) and hemodynamic variables (MAP and HR) over time, using time as the between-subject factor. Intergroup differences at the time points were analyzed if there is a significant change over time. Data were expressed as the mean ± SD, median (interquartile) or number (%). A P values <0.05 were considered to indicate statistical significance.
Results
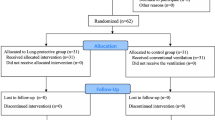
Sixty-five patients were screened for eligibility of this trial, and written informed consent to participate in this study was given to 62 patients. Patients were randomized into two groups. After randomization, 12 patients in group R and 10 patients in group P were excluded due to conversion to open surgery and intensive care unit admission without extubation. Thirty-nine patients (19 patients in group R and 20 patients in group P) completed the study and were analyzed from November 2012 to June 2014 (Fig. 2). There were no significant differences in patients and surgical characteristics between the two groups except intraoperative tidal volume (Table 1).
CONSORT diagram for the trial. Sixty-two patients were randomized into two groups. After randomization, 12 patients in Group R and 10 patients in Group P were excluded due to conversion to open surgery and intensive care unit admission without extubation. Thirty-nine patients (19 patients in group R and 20 patients in group P) completed the study and were included in final analysis. Group R: Conventional ventilation with alveolar recruitment maneuver (ARM) group; Group P: protective lung ventilation group
Postoperative pulmonary complication occurred less frequently in group P than in group R (P = 0.023, Table 2). Postoperative chest images suggested atelectasis in 8 patients of group R and 3 patients of group P. Pneumonia was diagnosed in 1 patients of group R. Desaturation below 90 % occurred more frequently in group R compared with group P (P = 0.016, Table 2). More patients in group R needed O2 via nasal cannula during transfer from PACU to ward (P = 0.049, Table 2). There was no statistical significance between two groups regarding the length of hospital stay (P = 0.499, Table 2), and none of the patients required major adverse events including barotrauma, postoperative ventilatory assistance and intensive care unit admission.
Repeated-measures ANOVA with serial ABGA revealed that there has been no difference in PaO2 (partial pressure arterial oxygen) between the two groups over time. In addition, PnP in the reverse Trendelenburg position did not decrease PaO2 in both groups. PAO2 (alveolar O2 concentrations) was significantly lower in group P compared with group R during PnP (P < 0.05), and AaDO2 (alveolar-arterial oxygen gradient) was significantly lower in group P compared with group R throughout the operation (P < 0.05, Fig. 3).
Oxygenation of the patients with PaO2, PAO2 and AaDO2. Group R: Conventional ventilation with alveolar recruitment maneuver (ARM) group; Group P: protective lung ventilation group; PreCO2: after the anesthetic induction; CO2_10 min: 10 min after pneumoperitoneum; CO2_20 min: 20 min after pneumoperitoneum; CO2_end: end of pneumoperitoneum; Op_end: operation end; PACU: post-anesthesia care unit; POD#1: postoperative 24 h; POD#2: postoperative 48 h *P < 0.05 compared with group R
There was no difference in PaCO2 and arterial pH over time between the two groups (P > 0.05) and PaCO2 increased and arterial pH decreased after the PnP and slowly recovered to baseline value after CO2 off in both groups (Fig. 4).
PaCO2 and arterial pH. Group R: Conventional ventilation with alveolar recruitment maneuver (ARM) group; Group P: protective lung ventilation group; PreCO2: after the anesthetic induction; CO2_10 min: 10 min after pneumoperitoneum; CO2_20 min: 20 min after pneumoperitoneum; CO2_end: end of pneumoperitoneum; Op_end: operation end; PACU: post-anesthesia care unit; POD#1: postoperative 24 h; POD#2: postoperative 48 h; *P < 0.05 compared with group R
Repeated-measures ANOVA revealed that PIPs were significantly lower in group P compared with those of group R throughout the surgery (Fig. 5). Peak inspiratory pressures (PIPs) were increased significantly after PnP in both groups, and this was continued until the end of the PnP (Fig. 5). There was no difference in MAP and HR between the two groups over time (Fig. 5).
Peak inspiratory pressures (PIP) and hemodynamic variables. Group R: Conventional ventilation with alveolar recruitment maneuver (ARM) group; Group P: protective lung ventilation group; PreCO2: after the anesthetic induction; CO2_10 min: 10 min after pneumoperitoneum; CO2_20 min: 20 min after pneumoperitoneum; CO2_end: end of pneumoperitoneum; MAP Mean arterial pressures; HR heart rates; Op_end operation end; *P < 0.05 compared with group R
Discussion
The present study showed that the use of PLV strategy with low tidal volume (6 ml/kg) and PEEP (5 cmH2O) provided beneficial effects for postoperative respiratory complications in patients undergoing laparoscopic surgery. Intraoperative PLV strategy decreased the incidence of postoperative atelectasis and desaturation compared with conventional ventilation (tidal volume of 10 ml/kg) and ARM (40 cm H2O for 30 s).
During PnP and general anesthesia for laparoscopic surgery, intraabdominal pressure is higher than airway pressure, and this pressure gradient displaces diaphragm, a thin fibromuscular layer. This pressure gradient frequently collapses adjacent pulmonary tissues and forms atelectasis [14]. In the current study, the incidences of postoperative pulmonary complications including atelectasis and pneumonia were lower in PLV group (low tidal volume with PEEP) than in conventional ventilation with ARM group during postoperative 2 days. Pneumonia occurred in only one patient of conventional ventilation with ARM group. In this study, ARM was conducted one time right after the end of PnP since ARM was expected to re-expand atelectasis occurring due to PnP. On the other hand, PEEP at levels greater than the opposing pressures on the lung during PnP was considered to prevent the redevelopment of atelectasis. Since the increase of intraabdominal pressure during PnP leads atelectasis formation during the expiratory phase of the respiratory cycle, PEEP prevents end-expiratory airway closure by increasing functional residual capacity and keeping the airways to remain open in patients with a decreased lung volume during PnP [4].
There were no differences in arterial oxygenation (PaO2) between conventional ventilation with ARM and PLV group, whereas alveolar O2 concentrations (PAO2) were significantly lower in PLV group compared with conventional ventilation with ARM group during PnP. The previous study conducted in patients with gynecological laparoscopic surgery with Trendelenburg lithotomy position showed that ARM applied before PnP improved oxygenation during operation [8]. Pang et al. [9] also reported that repeated ARMs during laparoscopic cholecystectomy improved arterial oxygenation compared with conventional ventilation. The effect of ARM on oxygenation could be attributed to optimal alveolar recruitment and improved regional ventilation, whereas the effect of PEEP is due to keeping the airways opened at the end of the expiratory period and maintaining adequate gas exchange [7]. However, the AaDO2 was lower in PLV group than in conventional with ARM group during PnP. AaDO2 means alveolar-arterial oxygen gradient and the elevated AaDO2 may explain the source of hypoxemia. PEEP during PLV seemed to decrease shunt during expiratory phase and may contribute to decrease of AaDO2.
In both groups, the volume-controlled ventilation was used and respiration rate was adjusted to keep end-tidal CO2 between 35 and 40 mmHg, and therefore, there were no differences in PaCO2 and arterial pH between the two groups. The subsequent increase of PaCO2 and decrease of arterial pH over time in both groups after PnP may be due to CO2 uptake after CO2 insufflation.
Peak inspiratory pressures (PIPs) of conventional ventilation with ARM group were higher than that of LPS group over time, which could be explained by the tidal volume of each group (10 ml/kg for conventional ventilation with ARM vs. 6 ml/kg for PLV group). After PnP, PIPs were increased due to the pressure transmission from abdomen to thoracic cavity. Hemodynamic variables such as MAP and HR were not significantly different between the two groups over time. ARM with high airway pressure and high PEEP is also reported as risk factors for lung barotrauma, which did not occur in the present study. However, adverse effects such as hypotension or barotrauma should always be considered, particularly in patients with hypovolemia or lung disease such as pleural blebs and smoking.
This study has a few limitations. First, the analyzed case numbers are small (19 or 21 for each group). This was the prospective study and the case number of 31 was calculated through power analysis. More than twenty patients were excluded from the final analysis due to the conversion to open surgery. However, the statistics with Chi-square test was significant even with the smaller case number that was calculated from the power analysis. Second, atelectasis presented on chest radiography was chosen for the primary outcome of this study since the formation of atelectasis during anesthesia and PnP is one of major contributors to the postoperative impaired pulmonary function [15, 16]. However, the area and amount of atelectasis can be made with spiral computerized tomography [15, 16], and functional parameters such as oxygenation or respiratory mechanics may be selected for the outcomes of postoperative pulmonary functions [8, 14, 17, 18]. Third, hepatobiliary surgeries with reverse Trendelenburg position were chosen for this study because the duration of PnP and operation are usually longer than other laparoscopic surgeries such as cholecystectomy or gastrectomy. Respiratory mechanics are influence by patients’ position, and therefore, the results of this study may be applied limitedly to other laparoscopic surgeries with Trendelenburg position.
Conclusion
In conclusion, the results of the current study suggest that protective lung strategy with low tidal volume (6 ml/kg) and 5 cm H2O of PEEP reduced the incidence of postoperative pulmonary complications compared with conventional ventilation with alveolar recruitment maneuver in patients undergoing laparoscopic hepatobiliary surgery. This study was conducted with healthy patients without lung disease for postoperative 2 days. However, patients with obesity or pulmonary disease predispose to postoperative pulmonary complications after laparoscopic surgery [19–22]. Further study regarding the effect of protective lung strategy with these high-risk patients during laparoscopy is needed.
References
Rockall TA, Demartines N (2014) Laparoscopy in the era of enhanced recovery. Best Pract Res Clin Gastroenterol 28:133–142
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31:1327–1335
Hedenstierna G, Rothen HU (2000) Atelectasis formation during anesthesia: causes and measures to prevent it. J Clin Monit Comput 16:329–335
Meininger D, Byhahn C, Mierdl S, Westphal K, Zwissler B (2005) Positive end-expiratory pressure improves arterial oxygenation during prolonged pneumoperitoneum. Acta Anaesthesiol Scand 49:778–783
Hazebroek EJ, Haitsma JJ, Lachmann B, Bonjer HJ (2002) Mechanical ventilation with positive end-expiratory pressure preserves arterial oxygenation during prolonged pneumoperitoneum. Surg Endosc 16:685–689
Takahata O, Kunisawa T, Nagashima M, Mamiya K, Sakurai K, Fujita S, Fujimoto K, Iwasaki H (2007) Effect of age on pulmonary gas exchange during laparoscopy in the Trendelenburg lithotomy position. Acta Anaesthesiol Scand 51:687–692
Futier E, Constantin JM, Jaber S (2014) Protective lung ventilation in operating room: a systematic review. Minerva Anestesiol 80:726–735
Park HP, Hwang JW, Kim YB, Jeon YT, Park SH, Yun MJ, Do SH (2009) Effect of pre-emptive alveolar recruitment strategy before pneumoperitoneum on arterial oxygenation during laparoscopic hysterectomy. Anaesth Intensive Care 37:593–597
Pang CK, Yap J, Chen PP (2003) The effect of an alveolar recruitment strategy on oxygenation during laparascopic cholecystectomy. Anaesth Intensive Care 31:176–180
Eisner MD, Thompson BT, Schoenfeld D, Anzueto A, Matthay MA, Acute Respiratory Distress Syndrome N (2002) Airway pressures and early barotrauma in patients with acute lung injury and acute respiratory distress syndrome. Am J Respir Crit Care Med 165:978–982
Lee HY, Lu CH, Lu HF, Chen CL, Wang CH, Cheng KW, Wu SC, Jawan B, Huang CJ (2012) Relationship between postoperative lung atelectasis and position of the endotracheal tube in pediatric living-donor liver transplantation. Transpl Proc 44:875–877
Abdullah HR, Chung F (2014) Postoperative issues: discharge criteria. Anesthesiol Clin 32:487–493
Karayiannakis AJ, Makri GG, Mantzioka A, Karousos D, Karatzas G (1996) Postoperative pulmonary function after laparoscopic and open cholecystectomy. Br J Anaesth 77:448–452
Nguyen NT, Anderson JT, Budd M, Fleming NW, Ho HS, Jahr J, Stevens CM, Wolfe BM (2004) Effects of pneumoperitoneum on intraoperative pulmonary mechanics and gas exchange during laparoscopic gastric bypass. Surg Endosc 18:64–71
Reinius H, Jonsson L, Gustafsson S, Sundbom M, Duvernoy O, Pelosi P, Hedenstierna G, Freden F (2009) Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 111:979–987
Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR, Magnusson L (2002) Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 95:1788–1792 table of contents
Kim JY, Shin CS, Kim HS, Jung WS, Kwak HJ (2010) Positive end-expiratory pressure in pressure-controlled ventilation improves ventilatory and oxygenation parameters during laparoscopic cholecystectomy. Surg Endosc 24:1099–1103
Maracaja-Neto LF, Vercosa N, Roncally AC, Giannella A, Bozza FA, Lessa MA (2009) Beneficial effects of high positive end-expiratory pressure in lung respiratory mechanics during laparoscopic surgery. Acta Anaesthesiol Scand 53:210–217
Tusman G, Bohm SH, Warner DO, Sprung J (2012) Atelectasis and perioperative pulmonary complications in high-risk patients. Curr Opin Anaesthesiol 25:1–10
Cheng SP, Chang YC, Liu CL, Yang TL, Jeng KS, Lee JJ, Liu TP (2008) Factors associated with prolonged stay after laparoscopic cholecystectomy in elderly patients. Surg Endosc 22:1283–1289
Futier E, Constantin JM, Pelosi P, Chanques G, Kwiatkoskwi F, Jaber S, Bazin JE (2010) Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology 113:1310–1319
Talab HF, Zabani IA, Abdelrahman HS, Bukhari WL, Mamoun I, Ashour MA, Sadeq BB, El Sayed SI (2009) Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg 109:1511–1516
Acknowledgments
This work was supported by the Grant No. 02-2013-072 from Seoul National University Bundang Hospital Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Park, Ryu, Kim, Oh, Han (S.H) and Han (H.S) have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Park, S.J., Kim, B.G., Oh, A.H. et al. Effects of intraoperative protective lung ventilation on postoperative pulmonary complications in patients with laparoscopic surgery: prospective, randomized and controlled trial. Surg Endosc 30, 4598–4606 (2016). https://doi.org/10.1007/s00464-016-4797-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4797-x