Abstract
Objective
To evaluate the effect of three-dimensional (3D) visualization on operative performance during elective laparoscopic liver resection (LLR).
Background
Major limitations of conventional laparoscopy are lack of depth perception and tactile feedback. Introduction of robotic technology, which employs 3D imaging, has removed only one of these technical obstacles. Despite the significant advantages claimed, 3D systems have not been widely accepted.
Methods
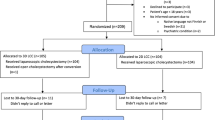
In this single institutional study, 20 patients undergoing LLR by high-definition 3D laparoscope between April 2014 and August 2014 were matched to a retrospective control group of patients who underwent LLR by two-dimensional (2D) laparoscope.
Results
The number of patients who underwent major liver resection was 5 (25 %) in the 3D group and 10 (25 %) in the 2D group. There was no significant difference in contralateral wedge resection or combined resections between the 3D and 2D groups. There was no difference in the proportion of patients undergoing previous abdominal surgery (70 vs. 77 %, p = 0.523) or previous hepatectomy (20 vs. 27.5 %, p = 0.75). The operative time was significantly shorter in the 3D group when compared to 2D (225 ± 109 vs. 284 ± 71 min, p = 0.03). There was no significant difference in blood loss in the 3D group when compared to 2D group (204 ± 226 in 3D vs. 252 ± 349 ml in 2D group, p = 0.291). The major complication rates were similar, 5 % (1/20) and 7.5 % (3/40), respectively, (p ≥ 0.99).
Conclusion
3D visualization may reduce the operating time compared to high-definition 2D. Further large studies, preferably prospective randomized control trials are required to confirm this.
Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiology
- LLR:
-
Laparoscopic liver resection
- LMH:
-
Laparoscopic major hepatectomy
- POD:
-
Postoperative day
References
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) World consensus conference on laparoscopic surgery. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg 250:825–830
Cheung TT, Poon RT, Yuen WK, Chok KS, Jenkins CR, Chan SC, Fan ST, Lo CM (2013) Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 257:506–511
Soubrane O, Schwarz L, Cauchy F, Perotto LO, Brustia R, Bernard D, Scatton O (2014) A conceptual technique for laparoscopic right hepatectomy based on facts and oncologic principles: the caudal approach. Ann Surg. doi:10.1097/SLA.0000000000000737
Soubrane O, Goumard C, Laurent A, Tranchart H, Truant S, Gayet B, Salloum C, Luc G, Dokmak S, Piardi T, Cherqui D, Dagher I, Boleslawski E, Vibert E, Sa Cunha A, Belghiti J, Pessaux P, Boelle PY, Scatton O (2014) Laparoscopic resection of hepatocellular carcinoma: a French survey in 351 patients. HPB (Oxford) 16:357–365
Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F (2008) Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc 22(10):2208–2213
Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM (2012) Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol 18:6657–6668
López-Ben S, Palacios O, Codina-Barreras A, Albiol MT, Falgueras L, Castro E, Figueras J (2014) Pure laparoscopic liver resection reduces surgical site infections and hospital stay. Results of a case-matched control study in 50 patients. Langenbecks Arch Surg 399:307–314
Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, Dagher I (2010) Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc 24:1170–1176
Truant S, Bouras AF, Hebbar M, Boleslawski E, Fromont G, Dharancy S, Leteurtre E, Zerbib P, Pruvot FR (2011) Laparoscopic resection vs. open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc 25:3668–3677
Sahu D, Mathew MJ, Reddy PK (2014) 3D laparoscopy—help or hype; initial experience of a tertiary health centre. J Clin Diagn Res 8(7):1–3
Gayet B, Cavaliere D, Vibert E, Perniceni T, Levard H, Denet C, Christidis C, Blain A, Mal F (2007) Totally laparoscopic right hepatectomy. Am J Surg 194:685–689
Gumbs AA, Gayet B (2007) Totally laparoscopic left hepatectomy. Surg Endosc 21:1221
Gumbs AA, Bar-Zakai B, Gayet B (2008) Totally laparoscopic extended left hepatectomy. J Gastrointest Surg 12:1152
Gumbs AA, Gayet B (2008) Multimedia article. Totally laparoscopic extended right hepatectomy. Surg Endosc 22:2076–2077
Gumbs AA, Gayet B (2008) Totally laparoscopic central hepatectomy. J Gastrointest Surg 12:1153
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964
Belli G, Gayet B, Han HS, Wakabayashi G, Kim KH, Cannon R, Kaneko H, Gamblin T, Koffron A, Dagher I, Buell JF (2013) Laparoscopic left hemihepatectomy a consideration for acceptance as standard of care. Surg Endosc 27:2721–2726
Nomi T, Fuks D, Agrawal A, Kawaguchi Y, Ogiso S, Gayet B (2015) Totally laparoscopic right hepatectomy combined with resection of the inferior vena cava by anterior approach. Ann Surg Oncol 22:851
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B (2014) Laparoscopic major hepatectomy for colorectal liver metastases in elderly patients: a single-center, case-matched study. Surg Endosc. doi:10.1007/s00464-014-3806-1
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828; discussion 828–829
Ishizawa T, Hasegawa K, Kokudo N, Sano K, Imamura H, Beck Y, Sugawara Y, Makuuchi M (2009) Risk factors and management of ascites after liver resection to treat hepatocellular carcinoma. Arch Surg 144:46–51
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Buchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Van Bergen P, Kunert W, Buess GF (2000) The effect of high definition imaging on surgical task efficiency in minimally invasive surgery: an experimental comparison between three dimensional imaging and direct vision through a stereoscopic TEM rectoscope. Surg Endosc 14(1):71–74
Gallagher AG, Ritter EM, Lederman AB, McClusky DA 3rd, Smith CD (2005) Video-assisted surgery represents more than a loss of three-dimensional vision. Am J Surg 189(1):76–80
Hubber JW, Taffinder N, Russell RC, Darzi A (2003) The effects of different viewing conditions on performance in simulated minimal access surgery. Ergonomics 46(10):999–1016
Wagner OJ, Hagen M, Kurmann A, Horgan S, Candinas D, Vorburger SA (2012) Three-dimensional vision enhances task performance independently of the surgical method. Surg Endosc 26(10):2961–2968
Smith R, Day A, Rockall T, Ballard K, Bailey M, Jourdan I (2012) Advanced stereoscopic projection technology significantly improves novice performance of minimally invasive surgical skills. Surg Endosc 26(6):1522–1527
Storz P, Buess GF, Kunert W, Kirschniak A (2012) 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 26(5):1454–1460
Honeck P, Wendt-Nordahl G, Rassweiler J, Knoll T (2012) 3D laparoscopic imaging improves surgical performance on standardized ex vivo laparoscopic tasks. J Endourol 26(8):1085–1088
LaGrange CA, Clark CJ, Gerber EW, Strup SE (2008) Evaluation of three laparoscopic modalities: robotics versus three-dimensional vision laparoscopy versus standard laparoscopy. J Endourol 22(3):511–516
Alaraimi B, El Bakbak W, Sarker S, Makkiyah S, Al-Marzouq A, Goriparthi R, Bouhelal A, Quan V, Patel B (2014) A randomized prospective study comparing acquisition of laparoscopic skills in three-dimensional (3D) vs. two-dimensional (2D) laparoscopy. World J Surg 38(11):2746–2752
Wilhelm D, Reiser S, Kohn N, Witte M, Leiner U, Mühlbach L, Ruschin D, Reiner W, Feussner H (2014) Comparative evaluation of HD 2D/3D laparoscopic monitors and benchmarking to a theoretically ideal 3D pseudodisplay: even well-experienced laparoscopists perform better with 3D. Surg Endosc 28(8):2387–2397
Bhayani SB, Andriole GL (2005) Three-dimensional (3D) vision: does it improve laparoscopic skills? An assessment of a 3D head-mounted visualization system. Rev Urol 7(4):211–214
Hanna GB, Shimi SM, Cuschieri A (1998) Randomized study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic procedures. Lancet 351:248–251
Gurusamy KS, Sahay S, Davidson BR (2011) Three dimensional versus two dimensional imaging for laparoscopic cholecystectomy. Cochrane Database Syst Rev. doi:10.1002/14651858.CD006882.pub2
Bilgen K, Ustün M, Karakahya M, Işik S, Sengül S, Cetinkünar S, Küçükpinar TH (2013) Comparison of 3D imaging and 2D imaging for performance time of laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 23(2):180–183
Kong SH, Oh BM, Yoon H, Ahn HS, Lee HJ, Chung SG, Shiraishi N, Kitano S, Yang HK (2010) Comparison of two- and three-dimensional camera systems in laparoscopic performance: a novel 3D system with one camera. Surg Endosc 24(5):1132–1143
Jourdan IC, Dutson E, Garcia A, Vleugels T, Leroy J, Mutter D, Marescaux J (2004) Stereoscopic vision provides a significant advantage for precision robotic laparoscopy. Br J Surg 91:879–885
Byrn JC, Schluender S, Divino CM, Conrad J, Gurland B, Shlasko E, Szold A (2007) Three-dimensional imaging improves surgical performance for both novice and experienced operators using the da Vinci Robot System. Am J Surg 193:519–522
Votanopoulos K, Brunicardi FC, Thornby J, Bellows CF (2008) Impact of three-dimensional vision in laparoscopic training. World J Surg 32:110–118
Patel HR, Ribal MJ, Arya M, Nauth-Misir R, Joseph JV (2007) Is it worth revisiting laparoscopic three-dimensional visualization? A validated assessment. Urology 70:47–49
Disclosures
Vimalraj Velayutham, David Fuks, Takeo Nomi, Yoshikuni Kawaguchi and Brice Gayet have no conflict of interest. Brice Gayet is consultant for Olympus.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Velayutham, V., Fuks, D., Nomi, T. et al. 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc 30, 147–153 (2016). https://doi.org/10.1007/s00464-015-4174-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4174-1