Abstract
Background
While energy devices are ubiquitous in the operating room, they remain poorly understood and can result in significant complications. The purpose of this study was to estimate the extent to which adding a novel bench-top component improves learning of SAGES’ Fundamental Use of Surgical Energy™ (FUSE) electrosurgery curriculum among surgical trainees.
Methods
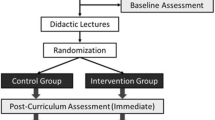
Surgical residents participated in a 1-h didactic electrosurgery (ES) course, based on the FUSE curriculum. They were then randomized to one of two groups: an unstructured hands-on session where trainees used ES devices (control group) or a goal-directed hands-on training session (Sim group). Pre- and post-curriculum (immediate and at 3 months) assessments included knowledge of ES (multiple-choice examination), self-perceived competence for each of the 35 course objectives (questionnaire), and self-perceived comfort with performance of seven tasks related to safe use of ES. Data expressed as median[interquartile range], *p < 0.05.
Results
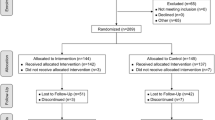
56 (29 control; 27 Sim) surgical trainees completed the curriculum and assessments. Baseline characteristics, including pre-curriculum exam and questionnaire scores, were similar. Total score on the exam improved from 46 %[40;54] to 84 %[77;91]* for the entire cohort, with higher immediate post-curriculum scores in the Sim group compared to controls (89 %[83;94] vs. 83 %[71;86]*). At 3 months, performance on the exam declined in both groups, but remained higher in the Sim group (77 %[69;90] vs 60 %[51;80]*). Participants in both groups reported feeling greater comfort and competence post-curriculum (immediate and at 3 months) compared to baseline. This improvement was greater in the Sim group with a higher proportion feeling “Very Comfortable” or “Fully Competent” (Sim: 3/7 tasks and 28/35 objectives; control: 0/7 tasks and 10/35 objectives).
Conclusions
A FUSE-based curriculum improved surgical trainees’ knowledge and comfort in the safe use of electrosurgical devices. The addition of a structured interactive bench-top simulation component further improved learning and retention at 3 months.


Similar content being viewed by others
References
ECRI Institute (2010) Health devices: top 10 health technology hazards for 2011. ECRI Institute, Plymouth Meeting
Mann D (2000) Reducing the hazard of burns and bovie pads. Plast Reconstr Surg 106:947
Nduka CC, Super PA, Monson JR, Darzi AW (1994) Cause and prevention of electrosurgical injuries in laparoscopy. J Am Coll Surg 179:161–170
Sankaranarayanan G, Resapu RR, Jones DB, Schwaitzberg S, De S (2013) Common uses and cited complications of energy in surgery. Surg Endosc 27:3056–3072
Agarwal BB, Gupta M, Agarwal S, Mahajan K (2007) Anatomical footprint for safe laparoscopic cholecystectomy without using any energy source: a modified technique. Surg Endosc 21:2154–2158
Polychronidis A, Tsaroucha AK, Karayiannakis AJ, Perente S, Efstathiou E, Simopoulos C (2005) Delayed perforation of the large bowel due to thermal injury during laparoscopic cholecystectomy. J Int Med Res 33:360–363
Darai E, Ackerman G, Bazot M, Rouzier R, Dubernard G (2007) Laparoscopic segmental colorectal resection for endometriosis: limits and complications. Surg Endosc 21:1572–1577
Market engineering research for the U. S. market for general surgery laparoscopy access and closure instruments. Medical and Healthcare Marketplace Guide. Frost and Sullivan, London (1999). http://www.dialogselect.com/business/cgi/present
Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD, Force FT (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Feldman L, Fuchshuber P, Jones D (eds) (2012) The SAGES manual on the Fundamental Use of Surgical Energy (FUSE). Springer, New York
Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ (2014) A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy. Ann Surg 259:236–248
Palter VN, Orzech N, Reznick RK, Grantcharov TP (2013) Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 257:224–230
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199:115–120
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 (discussion 463–454)
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Feldman LS, Brunt LM, Fuchshuber P, Jones DB, Jones SB, Mischna J, Munro MG, Rozner MA, Schwaitzberg SD, Committee SF (2013) Rationale for the Fundamental Use of Surgical Energy (FUSE) curriculum assessment: focus on safety. Surg Endosc 27:4054–4059
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525 (discussion 525–518)
Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, Minter RM (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243:854–860 (discussion 860–853)
Hyltander A, Liljegren E, Rhodin PH, Lonroth H (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA 3rd, Ramel S, Smith CD, Arvidsson D (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, Hutchison C (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177:167–170
Tsuda S, Scott D, Doyle J, Jones DB (2009) Surgical skills training and simulation. Curr Probl Surg 46:271–370
Dale E (1969) Audiovisiual methods in teaching, 3rd edn. Holt, Reinhart & Winston, New York
Masters K (2013) Edgar Dale’s Pyramid of Learning in medical education: a literature review. Med Teach 35:e1584–e1593
Ericsson K, Krampe R, Tesch-Romer C (1993) The role of deliberate practice in the acquisition of expert performance. Psychol Rev 100:363–406
Ericsson KNC (1994) Expert performance: its structure and acquisition. Am Psychol 49:725–747
Jowett N, LeBlanc V, Xeroulis G, MacRae H, Dubrowski A (2007) Surgical skill acquisition with self-directed practice using computer-based video training. Am J Surg 193:237–242
Schulz KF, Altman DG, Moher D, CONSORT Group (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332
Acknowledgments
We acknowledge the SAGES FUSE task force for the development of the FUSE curriculum and presentation slides, as well as the facilitators who assisted in conducting the electrosurgery course. This study was funded by the Canadian Association of General Surgeons Ethicon© Research Award and an unrestricted educational grant from ConMed Canada©. AM is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Covidien©.
Disclosures
Drs Amin Madani, Yusuke Watanabe, Daniel B Jones and Pascal Fuchshuber have no conflicts of interest or financial ties to disclose. Dr Liane Feldman is a consultant for Covidien and received an investigator-initiated research Grant from Ethicon. Drs Melina Vassiliou and Gerald M. Fried and have received unrestricted educational Grants from Covidien. Dr. Steven D Schwaitzberg has served on advisory panels and has received an honorarium from Stryker and Olympus. He has served on advisory panels for Neatstitch and Surgicquest. He has also received a Grant from Ethicon.
Funding
This study was funded by the Canadian Association of General Surgeons Ethicon© Research Award and an unrestricted educational grant from ConMed Canada©. AM is supported by the Quebec Health Science Research Scholarship (FRQ-S) and the McGill Surgeon-Scientist Program. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Covidien©.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the SAGES FUSE Task Force: Sharon L. Bachman, L. Michael Brunt, Bipan Chand, Suvranu De, Warren S. Grundfest, Daniel M. Herron, Gretchen Purcell Jackson, Daniel Bougere Jones, Dean J. Mikami, Chan W. Park, William S. Richardson.
Appendices
Appendices
Appendix 1: Electrosurgery course objectives
By the end of the curriculum, trainees should be able to
-
1.
Define proper electrosurgery terms
-
2.
In a clinical situation, identify the application of ohm’s law, power equation, and energy
-
3.
Explain the function (input and output) of a radiofrequency (RF) electrosurgical generator
-
4.
Identify the characteristics and differences between monopolar and bipolar instruments
-
5.
Identify the characteristics of the RF electromagnetic spectrum and why it is used for surgical applications
-
6.
Explain how RF electrical energy causes effects in cells and tissue
-
7.
Identify the different effects of ranges of temperature on cells and tissue
-
8.
Explain the clinical effects of changing current densities
By the end of the curriculum, trainees should be able to identify
-
9.
General patient protection measures for the electrosurgical generator
-
10.
Various mechanisms whereby electrosurgical injuries may occur
Circumstances, mechanisms and prevention of
-
11.
Dispersive electrode-related injury
-
12.
Direct coupling-related injury
-
13.
Insulation failure-related injury
-
14.
Injury due to unintentional activation of the active electrode
-
15.
Injury due to direct thermal extension from the active electrode
-
16.
Alternate site-related injury
-
17.
Capacitive coupling/induced current-related injury
-
18.
Injury from residual heat from instrument tip
-
19.
Energy-related single port access injury
-
20.
Burn injury by the operative team
-
21.
Hazards of byproducts and smoke produced during electrosurgery
-
22.
Circumstances which promote OR fires and identify prevention strategies
-
23.
Circumstances, mechanisms, and prevention of tracheotomy-related fires
-
24.
How to respond to an OR fire
-
25.
Problems that can occur when simultaneously using multiple energy devices
-
26.
The characteristics of basic and advanced bipolar electrosurgical instruments
-
27.
Clinical scenarios when basic bipolar instruments are indicated and identify appropriate power settings for use
-
28.
Performance optimization methods for advanced bipolar instruments
-
29.
Differences between bipolar and monopolar instruments as it relates to coupling, underwater use, current density, and lateral thermal spread
-
30.
Tissue characteristics that reduce the effectiveness of advanced bipolar instruments
-
31.
Considerations for electrosurgical device settings in infants and children
-
32.
Considerations for choice and placement of dispersive electrodes for infants and children
-
33.
Implanted devices that are affected by RF energy
-
34.
Surgical devices that can cause electromagnetic interference (EMI)
-
35.
Strategies to minimize interference from RF energy on a Cardiac Implanted Electronic Device (CIED)
Appendix 2: Simulation modules
Module 1: System setup
-
Objectives: At the end of module 1, participants will be able to
-
Describe and setup components of an ESU explaining their purpose and relationship to one another
-
Explain and demonstrate the relationship between the design of the dispersive electrode and patient safety
-
Describe circumstances, mechanisms, and prevention of dispersive electrode-related injury
-
-
Scenario: mannequin on the OR table with electrosurgical equipment
-
monopolar
-
bipolar
-
laparoscopic monopolar
-
-
Task A:
-
Identify all the components of the circuit
-
Identify all the jacks and controls on the ESU
-
Identify how to modify the waveform and power settings on the ESU
-
Setup a circuit using the monopolar hand device
-
For a laparotomy
-
For a right hip replacement
-
For a right humerus ORIF
-
For a median sternotomy
-
For a craniotomy
-
Setup a circuit using the monopolar laparoscopic device with a foot pedal
-
Setup a circuit using the bipolar foot-activated device
-
-
Task B:
-
Construct a circuit using monopolar ESU, 60 W light bulb, placing the split-pad dispersive elecrode on your arm and holding the light bulb in the same hand
-
Repeat with 20 W light bulb
-
Switch light bulb into other hand
-
Slowly unravel the dispersive electrode and observe the ESU’s response; describe how this would differ if a single-pad dispersive electrode was used
-
Module 2: Tissue effect
-
Objectives: at the end of module 2, participants will be able to
-
Demonstrate the appropriate technical skills required to handle and operate the electrosurgical device
-
Explain the different tissue and cellular effects that can be created by RF electrosurgical instruments
-
Identify the different effects of ranges of temperature on cells and tissue
-
Explain and demonstrate how to create desired tissue effects by altering current density, by varying: power, waveform, electrode contact with tissue
-
-
Scenario: steak will be placed on a bench-top and connected to a monopolar ESU using a single-pad dispersive electrode (Task A without the oscilloscope/analyzer; Task B with the oscilloscope/analyzer)
-
Task A:
-
Using proper technique, make series of parallel 5 cm long, 1 cm deep incisions with monopolar hand electrode on the steak, 1 cm apart with the following settings:
-
Tissue vaporization with minimal desiccation at 20 W, 50 W and 70 W, using pure and blend modalities
-
Desiccation of tissue at 20 W, 50 W and 70 W, using pure and blend modalities
-
Fulgurate an area of 1 cm × 1 cm on the steak
-
Using the ESU at 30 W and on fulguration, activate the flat side of the device tip first using pure “cut” and subsequently using “coag”
-
Using the ESU at 30 W and on “cut,” apply the electrode tip on the steak for a total of 5 s. Do this first using the tip only, and then using the flat side of the device tip
-
Using a scalpel to make a 1 cm perpendicular incision across the electrosurgical incisions, describe the tissue effects of each incision
-
-
Task B:
-
Using the monopolar device, connect the ES Analyzer and oscilloscope to the circuit and observe the waveforms created on the oscilloscope while using the monopolar device on the steak at 30 W in “cut”, “coag”, “blend 1”, “blend 2”, “blend 3” modes
-
Module 3: Mechanisms of electrosurgical injuries—I
-
Objectives: at the end of module 3, participants will be able to
-
Identify circumstances and mechanisms of:
-
Capacitive coupling/induced current-related injury
-
Injury from metal-to-metal arcing
-
Direct burn injury to the operator
-
-
Scenario: steak will be placed on a bench-top and connected to a monopolar ESU using a single-pad dispersive electrode
-
Task A: Demonstrate metal-to-metal arcing on a stapler line using a monopolar ESU set at 40 W coag
-
Task B: Induced current and capacitive-coupling
-
Wrap the cord of the monopolar hand electrode around the light bulb and activate using “cut” and “coag” at 50 W, with and without contact to the steak
-
Hold tissue forceps in one hand and hold monopolar hand electrode in other hand without touching the steak and activate using “cut” at 50 W, while instituting a small contact area between the tissue forceps and the steak. Do this while also making contact between monopolar electrode and steak. Repeat while wrapping the cord several times around your neck
-
-
Task C: Direct burn injury to the operator
-
Place a water-filled glove on the steak and activate the monopolar hand electrode on the glove using desiccation at 40 W
-
Module 4: Mechanisms of electrosurgical injuries—II
-
Objectives: at the end of module 3, participants will be able to
-
Identify circumstances and mechanisms of the following in relation to laparoscopy:
-
Capacitive coupling/induced current-related injury
-
Injury from insulation failure
-
-
Scenario: steak will be placed on a bench-top and connected to a laparoscopic foot-pedal activated monopolar ESU circuit using a single-pad dispersive electrode
-
Task A: Insulation failure
-
Attach laparoscopic graspers with insulation failure to the monopolar electrode and activate in proximity to steak at 50 W using coagulation waveform.
-
-
Task B: Induced current and capacitive-coupling
-
Wrap piece of ham around laparoscopic monopolar electrode and activate using “cut” at 50 W while instituting a small contact area between the steak and ham
-
Hold laparoscopic needle-driver in one hand and hold monopolar hand electrode connected to laparoscopic hook in other hand without touching the steak and activate using “cut” at 50 W, while instituting a small contact area between the needle-driver and the steak. Do this while maximizing contact between needle-driver and hook laparoscopic instruments.
-
Each station of the bench-top simulation included a variety of electrosurgical equipment with monopolar, bipolar, and laparoscopic setups, as well as an oscilloscope to depict waveform.

Rights and permissions
About this article
Cite this article
Madani, A., Watanabe, Y., Vassiliou, M.C. et al. Impact of a hands-on component on learning in the Fundamental Use of Surgical Energy™ (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28, 2772–2782 (2014). https://doi.org/10.1007/s00464-014-3544-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3544-4