Abstract
Background
A significant proportion of patients, especially the elderly undergoing colon resections, are likely to be discharged to a skilled care facility. This study aims to examine whether the technique of colectomy, open versus laparoscopic, contributed to their discharge to a skilled care facility.
Methods
This was a retrospective analysis using discharge data from the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality. Adult patients who underwent colectomy in 2009 were evaluated. SAS and SUDAAN software were used to provide weighted estimates and to account for the complex sampling design of the NIS. We compared routine discharge to nonroutine discharge, defined as transfer to short-term hospital, skilled nursing facility, intermediate care, home health, or another type of facility.
Results
A weighted total of 221,294 adult patients underwent colectomy in 2009 and had the primary outcome of discharge available. Of these colon resections, 70,361 (32 %) were performed laparoscopically and 150,933 (68 %) by open technique. A total of 139,047 (62.8 %) patients had routine discharge and 73,572 (33.3 %) nonroutine. A total of 8,445 (3.8 %) patients died while in the hospital, and 229 (0.1 %) left against medical advice and were excluded from further analysis. On univariate analysis, age ≥65 years, female gender, Black/Hispanic race, open technique (compared to laparoscopic), Medicare/Medicaid insurance status, comorbidity index of ≥1, and malignant primary diagnosis predicted nonroutine discharge. A multivariate logistic model was then used to predict nonroutine discharge in these patients using variables significant in the univariate analysis at the α = 0.05 significance level. In the multivariate analysis, open compared to laparoscopic technique was independently associated with increased likelihood of discharge to skilled care facilities (odds ratio 2.85, 95 % confidence interval 2.59–3.14).
Conclusions
In addition to the expected factors like advancing age, female gender, and increasing comorbidity index, open compared to laparoscopic technique for colectomy is associated with an increased likelihood of discharge to skilled care facilities. When feasible, the laparoscopic technique should be considered as an option, especially in the elderly patients who require colon resection, because it may reduce their likelihood of discharge to a skilled care facility.
Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Kemp JA, Finlayson SR (2008) Outcomes of laparoscopic and open colectomy: a national population-based comparison. Surg Innov 15(4):277–283
COST Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, Guillou PJ, Thorpe H, Brown J, Delgado S, Kuhrij E, Haglind E, Påhlman L, Transatlantic Laparoscopically Assisted vs Open Colectomy Trials Study Group (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142(3):298–303
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomized trial. Lancet 359:2224–2229
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Colon Cancer Laparoscopic or Open Resection Study Group (COLOR) (2005) Laparoscopic surgery versus open surgery for colon cancer: shortterm outcomes of a randomised trial. Lancet Oncol 6:477–484
Delaney CP, Chang E, Senagore AJ, Broder M (2008) Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg 247(5):819–824
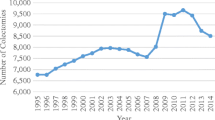
Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikov D (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg 256(3):462–468
Cone MM, Herzig DO, Diggs BS, Rea JD, Hardiman KM, Lu KC (2012) Effect of surgical approach on 30-day mortality and morbidity after elective colectomy: a NSQIP study. J Gastrointest Surg 16(6):1212–1217
Collins TC, Daley J, Henderson WH, Khuri SF (1999) Risk factors for prolonged length of stay after major elective surgery. Ann Surg 230(2):251–259
Leung JM, Dzankic S (2001) Relative importance of preoperative health status versus intraoperative factors in predicting postoperative adverse outcomes in geriatric surgical patients. J Am Geriatr Soc 49(8):1080–1085
Legner VJ, Doerner D, Reilly DF, McCormick WC (2004) Risk factors for nursing home placement following major nonemergent surgery. Am J Med 117(2):82–86
Legner VJ, Massarweh NN, Symons RG, McCormick WC, Flum DR (2009) The significance of discharge to skilled care after abdominopelvic surgery in older adults. Ann Surg 249(2):250–255
Oyetunji TA, Turner PL, Onguti SK, Ehanire ID, Dorsett FO, Fullum TM, Cornwell EE III, Haider AH (2013) Predictors of postdischarge complications: role of in-hospital length of stay. Am J Surg 205(1):71–76
Masoomi H, Kang CY, Chen A, Mills S, Dolich MO, Carmichael JC, Stamos MJ (2012) Predictive factors of in-hospital mortality in colon and rectal surgery. J Am Coll Surg 215(2):255–261
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139
Disclosures
Abhijit Shaligram, Lynette Smith, Pradeep Pallati, Anton Simorov, Jane Meza, and Dmitry Oleynikov have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaligram, A., Smith, L., Pallati, P. et al. Can laparoscopy for colon resection reduce the need for discharge to skilled care facility?. Surg Endosc 27, 4038–4043 (2013). https://doi.org/10.1007/s00464-013-3052-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3052-y