Abstract
Background
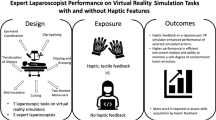
Surgeons performing laparoscopy need a high degree of psychomotor skills, which can be trained and assessed on virtual reality (VR) simulators. VR simulators simulate the surgical environment and assess psychomotor skills according to predefined parameters. This study aimed to validate a proficiency-based training setup that consisted of two tasks with predefined threshold values and handles with haptic feedback on the LapSim® VR simulator. The two tasks have been found to have construct validity in previous studies using handles without haptic feedback.
Methods
The participants were divided into three groups: novices (0–50 laparoscopic procedures), intermediates (51–300 laparoscopic procedures), and experts (more than 300 procedures). It was assumed that psychomotor skills increase with experience. All participants conducted the tasks lifting and grasping and fine dissection 20 times each. Validity of the training setup was investigated by comparing the number of times each participant passed a predefined threshold level for a set of 19 parameters.
Results
Construct validity was established for one parameter; “misses on right side” on the lifting and grasping task, whereas the other 18 parameters did not show construct validity.
Conclusion
The setup employed in this study failed to establish construct validity for more than one parameter. This indicates that the simulation of haptic feedback influences the training performance on laparoscopic simulators and is an important part of validating a training setup. A haptic device should generate haptic sensations in a realistic manner, without introducing frictional forces that are not inherent to laparoscopy.







Similar content being viewed by others
Abbreviations
- VR:
-
Virtual reality
- OR:
-
Operating room
References
Darzi A, Smith S, Taffinder N (1999) Assessing operative skill. Needs to become more objective. BMJ 318:887–888
Gallagher AG, Satava RM (2002) Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Learning curves and reliability measures. Surg Endosc 16:1746–1752
Kneebone R (2003) Simulation in surgical training: educational issues and practical implications. Med Educ 37:267–277
Gallagher AG, Richie K, McClure N, McGuigan J (2001) Objective psychomotor skills assessment of experienced, junior, and novice laparoscopists with virtual reality. World J Surg 25:1478–1483
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Kolozsvari NO, Feldman LS, Vassiliou MC, Demyttenaere S, Hoover ML (2011) Sim one, do one, teach one: considerations in designing training curricula for surgical simulation. J Surg Educ 68:421–427
Gauger PG, Hauge LS, Andreatta PB, Hamstra SJ, Hillard ML, Arble EP, Kasten SJ, Mullan PB, Cederna PS, Minter RM (2010) Laparoscopic simulation training with proficiency targets improves practice and performance of novice surgeons. Am J Surg 199:72–80
Aggarwal R, Moorthy K, Darzi A (2004) Laparoscopic skills training and assessment. Br J Surg 91:1549–1558
Moorthy K, Munz Y, Sarker SK, Darzi A (2003) Objective assessment of technical skills in surgery. BMJ 327:1032–1037
Duffy AJ, Hogle NJ, McCarthy H, Lew JI, Egan A, Christos P, Fowler DL (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19:401–405
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191:28–32
Thijssen AS, Schijven MP (2010) Contemporary virtual reality laparoscopy simulators: quicksand or solid grounds for assessing surgical trainees? Am J Surg 199:529–541
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244:310–314
Satava RM (2008) Historical review of surgical simulation—a personal perspective. World J Surg 32:141–148
Fried MP, Gallagher AG, Satava RM (2004) Training to proficiency: aircraft to OR. Arch Otolaryngol Head Neck Surg 130:1145–1146
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA 3rd, Ramel S, Smith CD, Arvidsson D (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
Brinkman WM, Buzink SN, Alevizos L, de Hingh IH, Jakimowicz JJ (2012) Criterion-based laparoscopic training reduces total training time. Surg Endosc 26:1095–1101
Brunner WC, Korndorffer JR Jr, Sierra R, Dunne JB, Yau CL, Corsetti RL, Slakey DP, Townsend MC, Scott DJ (2005) Determining standards for laparoscopic proficiency using virtual reality. Am Surg 71:29–35
Datta V, Bann S, Aggarwal R, Mandalia M, Hance J, Darzi A (2006) Technical skills examination for general surgical trainees. Br J Surg 93:1139–1146
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2003) Learning curves and impact of previous operative experience on performance on a virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185:146–149
Aggarwal R, Ward J, Balasundaram I, Sains P, Athanasiou T, Darzi A (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246:771–779
Haluck RS, Krummel TM (2000) Computers and virtual reality for surgical education in the 21st century. Arch Surg 135:786–792
van Dongen KW, Tournoij E, van der Zee DC, Schijven MP, Broeders IA (2007) Construct validity of the LapSim: can the LapSim virtual reality simulator distinguish between novices and experts? Surg Endosc 21:1413–1417
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, Jarvi KA (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240:374–381
Melvin WS, Johnson JA, Ellison EC (1996) Laparoscopic skills enhancement. Am J Surg 172:377–379
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, MacAulay C, Mancini ME, Morimoto T, Soper N, Ziv A, Reznick R (2010) Training and simulation for patient safety. Qual Saf Health Care 19(Suppl 2):i34–i43
Hyltander A, Liljegren E, Rhodin PH, Lonroth H (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328
Rehrig ST, Powers K, Jones DB (2008) Integrating simulation in surgery as a teaching tool and credentialing standard. J Gastrointest Surg 12:222–233
Gallagher AG, Ritter EM, Satava RM (2003) Fundamental principles of validation, and reliability: rigorous science for the assessment of surgical education and training. Surg Endosc 17:1525–1529
Carter FJ, Schijven MP, Aggarwal R, Grantcharov T, Francis NK, Hanna GB, Jakimowicz JJ (2005) Consensus guidelines for validation of virtual reality surgical simulators. Surg Endosc 19:1523–1532
Feldman LS, Sherman V, Fried GM (2004) Using simulators to assess laparoscopic competence: ready for widespread use? Surgery 135:28–42
Haluck RS, Marshall RL, Krummel TM, Melkonian MG (2001) Are surgery training programs ready for virtual reality? A survey of program directors in general surgery. J Am Coll Surg 193:660–665
Gurusamy KS, Aggarwal R, Palanivelu L, Davidson BR (2009) Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev (1):CD006575
Seymour NE (2008) VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg 32:182–188
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 discussion 463-454
Fairhurst K, Strickland A, Maddern G (2011) The LapSim virtual reality simulator: promising but not yet proven. Surg Endosc 25(2):343–355
Schout BM, Hendrikx AJ, Scheele F, Bemelmans BL, Scherpbier AJ (2010) Validation and implementation of surgical simulators: a critical review of present, past, and future. Surg Endosc 24:536–546
Schijven M, Jakimowicz J (2003) Virtual reality surgical laparoscopic simulators. Surg Endosc 17:1943–1950
Satava RM (2001) Surgical education and surgical simulation. World J Surg 25:1484–1489
Ottermo MV, Ovstedal M, Langø T, Stavdahl O, Yavuz Y, Johansen TA, Mårvik R (2006) The role of tactile feedback in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 16:390–400
van der Meijden OA, Schijven MP (2009) The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surg Endosc 23:1180–1190
Westebring-van der Putten EP, Goossens RH, Jakimowicz JJ, Dankelman J (2008) Haptics in minimally invasive surgery—a review. Minim Invasive Ther Allied Technol 17:3–16
Sherman V, Feldman LS, Stanbridge D, Kazmi R, Fried GM (2005) Assessing the learning curve for the acquisition of laparoscopic skills on a virtual reality simulator. Surg Endosc 19:678–682
Ro CY, Toumpoulis IK, Ashton RC Jr, Jebara T, Schulman C, Todd GJ, Derose JJ Jr, McGinty JJ (2005) The LapSim: a learning environment for both experts and novices. Stud Health Technol Inform 111:414–417
Botden SM, Buzink SN, Schijven MP, Jakimowicz JJ (2007) Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg 31:764–772
Aggarwal R, Tully A, Grantcharov T, Larsen CR, Miskry T, Farthing A, Darzi A (2006) Virtual reality simulation training can improve technical skills during laparoscopic salpingectomy for ectopic pregnancy. BJOG 113:1382–1387
Larsen CR, Grantcharov T, Aggarwal R, Tully A, Sorensen JL, Dalsgaard T, Ottesen B (2006) Objective assessment of gynecologic laparoscopic skills using the LapSimGyn virtual reality simulator. Surg Endosc 20:1460–1466
Hassan I, Maschuw K, Rothmund M, Koller M, Gerdes B (2006) Novices in surgery are the target group of a virtual reality training laboratory. Eur Surg Res 38:109–113
Eriksen JR, Grantcharov T (2005) Objective assessment of laparoscopic skills using a virtual reality stimulator. Surg Endosc 19:1216–1219
Langelotz C, Kilian M, Paul C, Schwenk W (2005) LapSim virtual reality laparoscopic simulator reflects clinical experience in German surgeons. Langenbecks Arch Surg 390:534–537
van Dongen KW, Ahlberg G, Bonavina L, Carter FJ, Grantcharov TP, Hyltander A, Schijven MP, Stefani A, van der Zee DC, Broeders IA (2011) European consensus on a competency-based virtual reality training program for basic endoscopic surgical psychomotor skills. Surg Endosc 25(1):166–171
Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B (2005) A virtual reality simulator for objective assessment of surgeons’ laparoscopic skill. Chirurg 76:151–156
Danila R, Gerdes B, Ulrike H, Dominguez Fernandez E, Hassan I (2009) Objective evaluation of minimally invasive surgical skills for transplantation. Surgeons using a virtual reality simulator. Chirurgia (Bucur) 104:181–185
Tanoue K, Uemura M, Kenmotsu H, Ieiri S, Konishi K, Ohuchida K, Onimaru M, Nagao Y, Kumashiro R, Tomikawa M, Hashizume M (2010) Skills assessment using a virtual reality simulator, LapSim, after training to develop fundamental skills for endoscopic surgery. Minim Invasive Ther Allied Technol 19:24–29
Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L (2006) Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 296:1094–1102
Reznick RK, MacRae H (2006) Teaching surgical skills—changes in the wind. N Engl J Med 355:2664–2669
Chmarra MK, Grimbergen CA, Jansen FW, Dankelman J (2010) How to objectively classify residents based on their psychomotor laparoscopic skills? Minim Invasive Ther Allied Technol 19:2–11
Sutherland LM, Middleton PF, Anthony A, Hamdorf J, Cregan P, Scott D, Maddern GJ (2006) Surgical simulation: a systematic review. Ann Surg 243:291–300
Chmarra MK, Jansen FW, Grimbergen CA, Dankelman J (2008) Retracting and seeking movements during laparoscopic goal-oriented movements. Is the shortest path length optimal? Surg Endosc 22:943–949
Chmarra MK, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2008) Force feedback and basic laparoscopic skills. Surg Endosc 22:2140–2148
Meneghetti AT, Pachev G, Zheng B, Panton ON, Qayumi K (2012) Objective assessment of laparoscopic skills: dual-task approach. Surg Innov 1553350611430673
Tholey G, Desai JP, Castellanos AE (2005) Force feedback plays a significant role in minimally invasive surgery: results and analysis. Ann Surg 241:102–109
van den Dobbelsteen JJ, Schooleman A, Dankelman J (2007) Friction dynamics of trocars. Surg Endosc 21:1338–1343
Buzink SN, Goossens RH, De Ridder H, Jakimowicz JJ (2010) Training of basic laparoscopy skills on SimSurgery SEP. Minim Invasive Ther Allied Technol 19:35–41
Våpenstad C, Buzink SN (2012) Procedural virtual reality simulation in minimally invasive surgery. Surg Endosc. doi:10.1007/s00464-012-2503-1
Picod G, Jambon AC, Vinatier D, Dubois P (2005) What can the operator actually feel when performing a laparoscopy? Surg Endosc 19:95–100
Thompson JR, Leonard AC, Doarn CR, Roesch MJ, Broderick TJ (2011) Limited value of haptics in virtual reality laparoscopic cholecystectomy training. Surg Endosc 25:1107–1114
Sjoerdsma W, Herder JL, Horward MJ, Jansen A, Bannenberg JJG, Grimbergen CA (1997) Force transmission of laparoscopic grasping instruments. Minim Invasive Ther Allied Technol 6:274–278
Botden SM, Torab F, Buzink SN, Jakimowicz JJ (2008) The importance of haptic feedback in laparoscopic suturing training and the additive value of virtual reality simulation. Surg Endosc 22:1214–1222
Zhou M, Tse S, Derevianko A, Jones DB, Schwaitzberg SD, Cao CG (2012) Effect of haptic feedback in laparoscopic surgery skill acquisition. Surg Endosc 26:1128–1134
Lamata P, Gomez EJ, Bello F, Kneebone RL, Aggarwal R, Lamata F (2006) Conceptual framework for laparoscopic VR simulators. IEEE Comput Graph 26:69–79
Salkini MW, Doarn CR, Kiehl N, Broderick TJ, Donovan JF, Gaitonde K (2010) The role of haptic feedback in laparoscopic training using the LapMentor II. J Endourol 24:99–102
Panait L, Akkary E, Bell RL, Roberts KE, Dudrick SJ, Duffy AJ (2009) The role of haptic feedback in laparoscopic simulation training. J Surg Res 156:312–316
Acknowledgments
The National Centre for Advanced Laparoscopic Surgery, SINTEF, the National Centre for Ultrasound and Image-Guided Therapy, and the Norwegian University of Science and Technology (all Trondheim, Norway) have supported this work. We thank all those who participated in the study, in addition to Sébastien Müller for help with the statistics
Disclosures
Cecilie Våpenstad, Erlend Fagertun Hofstad, Lars Eirik Bø, Magdalena Karolina Chmarra, Esther Kuhry, Gjermund Johnsen, Ronald Mårvik, and Thomas Langø have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Våpenstad, C., Hofstad, E.F., Bø, L.E. et al. Limitations of haptic feedback devices on construct validity of the LapSim® virtual reality simulator. Surg Endosc 27, 1386–1396 (2013). https://doi.org/10.1007/s00464-012-2621-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2621-9