Abstract
Background
Laparoendoscopic single-site (LESS) surgery is beginning to include advanced laparoscopic operations such as Heller myotomy with anterior fundoplication. However, the efficacy of LESS Heller myotomy has not been established. This study aimed to evaluate the authors’ initial experience with LESS Heller myotomy for achalasia.
Methods
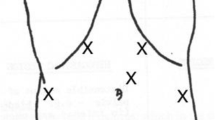
Transumbilical LESS Heller myotomy with concomitant anterior fundoplication for achalasia was undertaken for 66 patients after October 2007. Outcomes including operative time, complications, and length of hospital stay were recorded and compared with those for an earlier contiguous group of 66 consecutive patients undergoing conventional multi-incision laparoscopic Heller myotomy with anterior fundoplication. Symptoms before and after myotomy were scored by the patients using a Likert scale ranging from 0 (never/not severe) to 10 (always/very severe). Data were analyzed using the Mann–Whitney U test, the Wilcoxon matched-pairs test, and Fisher’s exact test where appropriate.
Results
Patients undergoing LESS Heller myotomy were similar to those undergoing conventional laparoscopic Heller myotomy in gender, age, body mass index (BMI), blood loss, and length of hospital stay. However, the patients undergoing LESS Heller myotomies had operations of significantly longer duration (median, 117 vs. 93 min with the conventional laparoscopic approach) (p < 0.003). For 11 patients (16%) undergoing LESS Heller myotomy, additional ports/incisions were required. No patients were converted to “open” operations, and no patients had procedure-specific complications. Symptom reduction was dramatic and satisfying after both LESS and conventional laparoscopic myotomy with fundoplication. The symptom reduction was similar with the two procedures. The LESS approach left no apparent umbilical scar.
Conclusion
Heller myotomy with anterior fundoplication effectively treats achalasia. The findings showed LESS Heller myotomy with anterior fundoplication to be feasible, safe, and efficacious. Although the LESS approach increases operative time, it does not increase procedure-related morbidity or hospital length of stay and avoids apparent umbilical scarring. Laparoendoscopic single-site surgery represents a paradigm shift to more minimally invasive surgery and is applicable to advanced laparoscopic operations such as Heller myotomy and anterior fundoplication.











Similar content being viewed by others
References
Cowgill S, Villadolid D, Boyle R, Al-Saadi S, Ross S, Rosemurgy A (2009) Laparoscopic Heller myotomy for achalasia: results after 10 years. Surg Endosc 23:2644–2649
Campos G, Vittinghoff E, Rabl C, Takata M, Gadenstatter M, Lin F, Ciovica R (2009) Endoscopic and surgical treatments of achalasia: a systemic review and meta-analysis. Ann Surg 249:45–57
Walzer N, Hirano I (2008) Achalasia. Gastroenterol Clin North Am 37:807–825
Eckardt A, Eckardt V (2009) Current clinical approach to achalasia. World J Gastroenterol 15:3969–3975
Lacey B, Weiser K (2008) Esophageal motility disorders: medical therapy. J Clin Gastroenterol 42:652–658
Rosemurgy A, Villadolid D, Thometz D, Kalipersad, Rakita S, Albrink M, Johnson M, Boyce W (2005) Laparoscopic Heller myotomy provides durable relief from achalasia and salvages failures after Botox or dilation. Ann Surg 241:725–735
Bloomston M, Boyce W, Mamel J, Albrink M, Murr M, Durkin A, Rosemurgy A (2000) Videoscopic Heller myotomy for achalasia: results beyond short-term follow-up. J Surg Res 92:150–156
Katilius M, Velanovich V (2001) Heller myotomy for achalasia: quality-of-life comparison of laparoscopic and open approaches. JSLS 5:227–231
Jeansonne L, White B, Pilger K, Shane M, Zagorski S, Davis S, Hunter J, Lin E, Smith C (2007) Ten-year follow-up of laparoscopic Heller myotomy for achalasia shows durability. Surg Endosc 21:1498–1502
Youssef Y, Richards W, Sharp K, Holtzman M, Sekhar N, Kaiser J, Torquati A (2007) Relief of dysphagia after laparoscopic Heller myotomy improves long-term quality of life. J Clin Gastroenterol 11:309–313
Cowgill S, Villadolid D, Al-Saadi S, Hedgecock J, Rosemurgy A (2007) Postmyotomy recollection of premyotomy symptoms of achalasia is very accurate, supporting longtitudinal studies of symptoms improvement. Surg Endosc 21:2183–2186
Bloomston M, Serafini F, Rosemurgy A (2001) Videoscopic Heller myotomy as first-line therapy for severe achalasia. Am Surg 67:1105–1109
Rosen M, Novitsky Y, Cobb W, Kercher K, Heniford T (2007) Laparoscopic Heller myotomy for achalasia in 101 patients: can successful symptomatic outcomes be predicted? Surg Innov 14:177–183
Sharp K, Khaitan L, Scholz S, Holzman M, Richards W (2002) 100 Consecutive minimally invasive heller myotomies: lessons learned. Ann Surg 235:631–639
Patti M, Pellegrini C, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Diener U, Eubanks T, Way L (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230:587–594
Leonard B, Broe P (2009) Oesophageal achalasia: an argument for primary surgical management. Surgeon 7:101–113
Cowgill S, Villadolid D, Al-Saadi S, Rosemurgy A (2007) Difficult myotomy is not determined by preoperative therapy and does not impact outcome. JSLS 11:336–343
Vaziri K, Soper N (2008) Laparoscopic Heller myotomy: technical aspects and operative pitfalls. J Gastrointest Surg 12:1586–1591
Rebecchi F, Giaccone C, Farinella E, Campaci R, Morino M (2008) Randomized controlled trial of laparoscopic Heller myotomy plus Dor fundoplication versus Nissen fundoplication for achalasia: long-term results. Ann Surg 248:1023–1030
Tapper D, Morton C, Kraemer E, Villadolid D, Ross S, Cowgill S, Rosemurgy A (2008) Does concomitant anterior fundoplication promote dysphasia after laparoscopic Heller myotomy? Am Surg 74:626–634
Tourquati A, Lutfi R, Khaitan K, Sharp W, Richards W (2006) Heller myotomy vs Heller myotomy plus Dor fundoplication: cost-utility analysis of a randomized trial. Surg Endosc 20:389–393
Tsuboi K, Omura N, Yano F, Kashiwagi H, Yanaga K (2009) Results after laparoscopic Heller-Dor operation for esophageal achalasia in 100 consecutive patients. Dis Esophagus 22:169–179
Hodgett S, Hernandez J, Morton C, Ross S, Albrink M, Rosemurgy A (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
Hernandez J, Morton C, Ross S, Albrink M, Rosemurgy A (2009) Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg 75:681–685
Bloomston M, Serafini F, Boyce W, Rosemurgy A (2002) The “learning curve” in videoscopic Heller myotomy. JSLS 6:41–47
Bloomston M, Durkin A, Boyce W, Johnson M, Rosemurgy A (2004) Early results of laparoscopic Heller myotomy do not necessarily predict long-term outcome. Am J Surg 187:403–407
Disclosures
Sharona Ross and Alexander S. Rosemurgy have received educational and research grants from Covidien Ltd., Olympus America Inc., and Stryker Corp. Linda Barry, Sujat Dahal, Connor Morton, Chinyere Okpaleke, and Melissa Rosas have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barry, L., Ross, S., Dahal, S. et al. Laparoendoscopic single-site Heller myotomy with anterior fundoplication for achalasia. Surg Endosc 25, 1766–1774 (2011). https://doi.org/10.1007/s00464-010-1454-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1454-7