Abstract
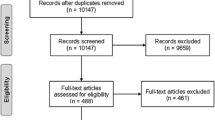
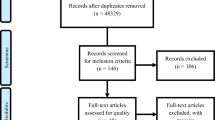
Foods and liquids have properties that are often modified as part of clinical dysphagia management to promote safe and efficient swallowing. However, recent studies have questioned whether this practice is supported by the evidence. To address this, a scoping review was conducted to answer the question: “Can properties of food and liquids modify swallowing physiology and function in adults?” Online search in six databases yielded a set of 4235 non-duplicate articles. Using COVIDENCE software, two independent reviewers screened the articles by title and abstract, and 229 full-text articles were selected for full-text review. One-hundred eleven studies met the inclusion criteria for qualitative synthesis and assessment of risk of bias. Three randomized controlled trials and 108 non-randomized studies were analyzed. Large amounts of variability in instrumental assessment, properties of food and liquids, and swallowing measures were found across studies. Sour, sweet, and salty taste, odor, carbonation, capsaicin, viscosity, hardness, adhesiveness, and cohesiveness were reported to modify the oral and pharyngeal phase of swallowing in both healthy participants and patients with dysphagia. Main swallow measures modified by properties of food and liquids were penetration/aspiration, oral transit time, lingual pressures, submental muscle contraction, oral and pharyngeal residue, hyoid and laryngeal movement, pharyngeal and upper esophageal sphincter pressures, and total swallow duration. The evidence pooled in this review supports the clinical practice of food texture and liquid consistency modification in the management of dysphagia with the caveat that all clinical endeavors must be undertaken with a clear rationale and patient-specific evidence that modifying food or liquid benefits swallow safety and efficiency while maintaining quality of life.

Similar content being viewed by others
References
Gonzalez-Fernandez M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after stroke: an overview. Curr Phys Med Rehabil Rep. 2013;1(3):187–96. https://doi.org/10.1007/s40141-013-0017-y.
Christmas C, Rogus-Pulia N. Swallowing disorders in the older population. J Am Geriatr Soc. 2019;67(12):2643–9. https://doi.org/10.1111/jgs.16137.
Rogus-Pulia N, Wirth R, Sloane P. Dysphagia in frail older persons: making the most of current knowledge. J Am Med Dir Assoc. 2018;19(9):736–40. https://doi.org/10.1016/j.jamda.2018.07.018.
Barczi S, Sullivan P, Robbins J. How should dysphagia care of older adults differ? Establishing optimal practice patterns. Semin Speech Lang. 2000;21(4):347–61. https://doi.org/10.1055/s-2000-8387.
Aslam M, Vaezi M. Dysphagia in the elderly. Gastroenterol Hepatol (N Y). 2013;9(12):784–95.
Humbert IA, Robbins J. Dysphagia in the elderly. Phys Med Rehabil Clin N Am. 2008;19(4):853–66. https://doi.org/10.1016/j.pmr.2008.06.002.
Sakai K, et al. Submental muscle activity and its role in diagnosing sarcopenic dysphagia. Clin Interv Aging. 2020;15:1991–9. https://doi.org/10.2147/CIA.S278793.
Robbins J, Hamilton J, Lof G, Kempster G. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103(3):823–9. https://doi.org/10.1016/0016-5085(92)90013-O.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A. 1995;50(5):M257–62. https://doi.org/10.1093/gerona/50a.5.m257.
Nicosia MA, et al. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A. 2000;55(11):M634–40. https://doi.org/10.1093/gerona/55.11.m634.
Rogus-Pulia N, Robbins J. Approaches to the rehabilitation of dysphagia in acute poststroke patients. Semin Speech Lang. 2013;34(03):154–69. https://doi.org/10.1055/s-0033-1358368.
Rogus-Pulia N, Malandraki G, Johnson S, Robbins J. Understanding dysphagia in dementia: the present and the future. Curr Phys Med Rehabil Rep. 2015;3(1):86–97. https://doi.org/10.1007/s40141-015-0078-1.
Ciucci M, Hoffmeister J, Wheeler-Hegland K. Management of dysphagia in acquired and progressive neurologic conditions. Semin Speech Lang. 2019;40(1098–9056):203–12. https://doi.org/10.1055/s-0039-1688981.
Ciucci M, et al. Early identification and treatment of communication and swallowing deficits in Parkinson disease. Semin Speech Lang. 2013;34(1098–9056):185–202. https://doi.org/10.1055/s-0033-1358367.
Perry B, Stipancic K, Martino R, Plowman E, Green J. Biomechanical biomarkers of tongue impairment during swallowing in persons diagnosed with amyotrophic lateral sclerosis. Dysphagia. 2021;36(1):147–56. https://doi.org/10.1007/s00455-020-10116-z.
Mittal B, et al. Swallowing dysfunction—preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J Radiat Oncol Biol Phys. 2003;57(5):1219–30. https://doi.org/10.1016/S0360-3016(03)01454-8.
Logemann JA. Dysphagia—evaluation and treatment. Folia Phoniatr Logop. 1995;47(3):140–64. https://doi.org/10.1159/000266348.
Logemann JA. Rehabilitation of oropharyngeal swallowing disorders. Acta Otorhinolaryngol Belg. 1994;48(2):207–15.
Clave P, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24(9):1385–94. https://doi.org/10.1111/j.1365-2036.2006.03118.x.
Rofes L, Arreola V, Mukherjee R, Swanson J, Clave P. The effects of a xanthan gum-based thickener on the swallowing function of patients with dysphagia. Aliment Pharmacol Ther. 2014;39(10):1169–79. https://doi.org/10.1111/apt.12696.
Newman R, Vilardell N, Clave P, Speyer R. Effect of bolus viscosity on the safety and efficacy of swallowing and the kinematics of the swallow response in patients with oropharyngeal dysphagia: white paper by the European Society for Swallowing Disorders (ESSD). Dysphagia. 2016;31(2):232–49. https://doi.org/10.1007/s00455-016-9696-8.
Bolivar-Prados M, et al. Effect of a gum-based thickener on the safety of swallowing in patients with poststroke oropharyngeal dysphagia. Neurogastroenterol Motil. 2019. https://doi.org/10.1111/nmo.13695.
O’Keeffe ST. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified? BMC Geriatr. 2018;18(1):167. https://doi.org/10.1186/s12877-018-0839-7.
Swan K, Speyer R, Heijnen BJ, Wagg B, Cordier R. Living with oropharyngeal dysphagia: effects of bolus modification on health-related quality of life—a systematic review. Qual Life Res. 2015;24(10):2447–56. https://doi.org/10.1007/s11136-015-0990-y.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63. https://doi.org/10.1161/01.STR.0000190056.76543.eb.
Roden DF, Altman KW. Causes of dysphagia among different age groups a systematic review of the literature. Otolaryngol Clin North Am. 2013;46(6):965. https://doi.org/10.1016/j.otc.2013.08.008.
Kalf JG, de Swart BJ, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord. 2012;18(4):311–5. https://doi.org/10.1016/j.parkreldis.2011.11.006.
Chen JEL. Food oral processing. Fundamentals of eating and sensory perception. New York: Wiley; 2012.
Cichero J. Age-related changes to eating and swallowing impact frailty: aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics (Basel). 2018. https://doi.org/10.3390/geriatrics3040069.
Kilcast D. Instrumental assessment of food sensory quality. A practical guide. Philadelphia: Woodhead Publishing Limited; 2013.
Organization IS (2008) ISO 5492:2008. Sensory analysis—vocabulary. https://www.iso.org/obp/ui/#iso:std:iso:5492:ed-2:v1:en
Loret C. Using sensory properties of food to trigger swallowing: a review. Crit Rev Food Sci Nutr. 2015;55(1):140–5. https://doi.org/10.1080/10408398.2011.649810.
Steele CM, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015. https://doi.org/10.1007/s00455-014-9578-x.
Flynn E, Smith CH, Walsh CD, Walshe M. Modifying the consistency of food and fluids for swallowing difficulties in dementia. Cochrane Database Sys Rev. 2018. https://doi.org/10.1002/14651858.CD011077.pub2.
Moher D, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340: c869. https://doi.org/10.1136/bmj.c869.
Sterne JAC, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019. https://doi.org/10.1002/14651858.CD201601.
Sterne, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919.
Logemann JA, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res. 2008;51(1):173–83. https://doi.org/10.1044/1092-4388(2008/013).
Pauloski BR, et al. Effects of enhanced bolus flavors on oropharyngeal swallow in patients treated for head and neck cancer. Head Neck. 2013;35(8):1124–31. https://doi.org/10.1002/hed.23086.
Ortega O, Rofes L, Martin A, Arreola V, Lopez I, Clave P. A comparative study between two sensory stimulation strategies after two weeks treatment on older patients with oropharyngeal dysphagia. Dysphagia. 2016;31(5):706–16. https://doi.org/10.1007/s00455-016-9736-4.
Murakami K, et al. Coordination of tongue pressure production, hyoid movement, and suprahyoid muscle activity during squeezing of gels. Archiv Oral Biol. 2020;111:104631. https://doi.org/10.1016/j.archoralbio.2019.104631.
Murakami K, et al. Effect of fracture properties of gels on tongue pressure during different phases of squeezing and swallowing. J Text Stud. 2021;52(1745–4603):303–13. https://doi.org/10.1111/jtxs.12593.
Hori K, et al. Comparison of mechanical analyses and tongue pressure analyses during squeezing and swallowing of gels. Food Hydrocolloids. 2015;44:145–55. https://doi.org/10.1016/j.foodhyd.2014.09.029.
Ishihara S, Nakauma M, Funami T, Tanaka T, Nishinari K, Kohyama K. Electromyography during oral processing in relation to mechanical and sensory properties of soft gels. J Text Stud. 2011;42(4):254–67. https://doi.org/10.1111/j.1745-4603.2010.00272.x.
Moritaka H, Nakazawa F. Flow velocity of a bolus in the pharynx and rheological properties of agar and gelatin. J Text Stud. 2010;41(2):139–52. https://doi.org/10.1111/j.1745-4603.2010.00218.x.
Inoue Y, Sasai M, Shiga S, Moritaka H. Effects of gel amount and mastication on the velocity of agar and gelatin gels passing through the Pharynx. J Jpn Soc Food Sci Technol (Jpn). 2009;56(5):261–70. https://doi.org/10.3136/nskkk.56.261.
Yokoyama S, et al. Tongue pressure modulation for initial gel consistency in a different oral strategy. PLoS ONE. 2014;9(3): e91920. https://doi.org/10.1371/journal.pone.0091920.
Park D, Shin CM, Ryu JS. Effect of different viscosities on pharyngeal pressure during swallowing: a study using high-resolution manometry. Arch Phys Med Rehabil. 2017;98(3):487–94. https://doi.org/10.1016/j.apmr.2016.07.013.
Matsuo K, Kawase S, Wakimoto N, Iwatani K, Masuda Y, Ogasawara T. Effect of viscosity on food transport and swallow initiation during eating of two-phase food in normal young adults: a pilot study. Dysphagia. 2013;28(1):63–8. https://doi.org/10.1007/s00455-012-9413-1.
Kim YTT, Ogoshi H. Effect of added salt on the ease of swallow and masticatory muscle activity for minced pork. Jpn Soc Cond Sci. 2010;43(5):294–300. https://doi.org/10.11402/cookeryscience.43.294.
Ding R, Logemann J, Larson C, Rademaker A. The effects of taste and consistency on swallow physiology in younger and older healthy individuals: a surface electromyographic study. J Speech Lang Hear Res. 2003;46(4):977–89. https://doi.org/10.1044/1092-4388(2003/076).
Shaker R, et al. Effect of aging and bolus variables on pharyngeal and upper esophageal sphincter motor function. Am J Physiol. 1993;264(0002–9513):G427–32. https://doi.org/10.1152/ajpgi.1993.264.3.G427.
Pouderoux P, Kahrilas P. Deglutitive tongue force modulation by volition, volume, and viscosity in humans. Gastroenterology. 1995;108(5):1418–26. https://doi.org/10.1016/0016-5085(95)90690-8.
Raut VV, McKee GJ, Johnston BT. Effect of bolus consistency on swallowing–does altering consistency help? Eur Arch Otorhinolaryngol. 2001;258(0937–4477):49–53. https://doi.org/10.1007/s004050000301.
Taniguchi H, Tsukada T, Ootaki S, Yamada Y, Inoue M. Correspondence between food consistency and suprahyoid muscle activity, tongue pressure, and bolus transit times during the oropharyngeal phase of swallowing. J Appl Physiol. 2008;105(3):791–9. https://doi.org/10.1152/japplphysiol.90485.2008.
Tsukada T, Taniguchi H, Ootaki S, Yamada Y, Inoue M. “Effects of food texture and head posture on oropharyngeal swallowing,” (in eng). J Appl Physiol. 2009;106(6):1848–57. https://doi.org/10.1152/japplphysiol.91295.2008.
Bülow M, Olsson R, Ekberg O. “Videoradiographic analysis of how carbonated thin liquids and thickened liquids affect the physiology of swallowing in subjects with aspiration on thin liquids,” (in eng). Acta Radiol. 2003. https://doi.org/10.1034/j.1600-0455.2003.00100.x.
Lee K, Kim W, Kim E, Lee J. Is swallowing of all mixed consistencies dangerous for penetration-aspiration? Am J Phys Med Rehabil. 2012;91(3):187–92. https://doi.org/10.1097/PHM.0b013e318238a0e3.
Matsuo K, Yokoyama M, Gonzalez-Fern M, Saitoh E, Kagaya H, Baba M, et al. Effects of Food Consistencies and Mastication on Bolus Transport and Swallow Initiation in Individuals with Hemispheric Stroke. J Neurol Neurophysiol. 2015. https://doi.org/10.4172/2155-9562.1000269.
Saitoh E, Shibata S, Matsuo K, Baba M, Fujii W, Palmer JB. Chewing and food consistency: effects on bolus transport and swallow initiation. Dysphagia. 2007. https://doi.org/10.1007/s00455-006-9060-5.
Stachler R, et al. Swallowing of bolus types by postsurgical head and neck cancer patients. Head Neck. 1994;16(5):413–9. https://doi.org/10.1002/hed.2880160504.
Ayala K, Logemann J. Effects of altered sensory bolus characteristics and repeated swallows in Healthy young and elderly subjects. J Med Speech Lang Pathol Orig. 2010;18(3):34–58.
Bhattacharyya N, Kotz T, Fau-Shapiro J, Shapiro J. The effect of bolus consistency on dysphagia in unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 2003. https://doi.org/10.1016/s0194-5998(03)00633-8.
Bisch EM, Logemann J, Fau-Rademaker AW, Rademaker A, Fau-Kahrilas PJ, Fau-Lazarus CL, Lazarus CL. Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Speech Hear Res. 1994. https://doi.org/10.1044/jshr.3705.1041.
Butler S, Stuart A, Case L, Rees C, Vitolins M, Kritchevsky S. Effects of liquid type, delivery method, and bolus volume on penetration-aspiration scores in healthy older adults during flexible endoscopic evaluation of swallowing. Ann Otol Rhinol Laryngol. 2011;120(5):288–95. https://doi.org/10.1177/000348941112000502.
Butler S, Stuart A, Castell D, Russell G, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume on pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52(1):240–53. https://doi.org/10.1044/1092-4388(2008/07-0092).
Chi-Fishman G, Sonies B. Effects of systematic bolus viscosity and volume changes on hyoid movement kinematics. Dysphagia. 2002;17(4):278–87. https://doi.org/10.1007/s00455-002-0070-7.
Dantas RO, et al. “Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing,” (in eng). Am J Physiol. 1990;258(0002–9513):G675–81. https://doi.org/10.1152/ajpgi.1990.258.5.G675.
Diniz P, Vanin G, Xavier R, Parente M. Reduced incidence of aspiration with spoon-thick consistency in stroke patients. Nutrition. 2009;24(3):414–8. https://doi.org/10.1177/0884533608329440.
Gingrich L, Stierwalt J, Hageman C, LaPointe L. Lingual propulsive pressures across consistencies generated by the anteromedian and posteromedian tongue by healthy young adults. J Speech Lang Hear Res. 2012;55(3):960–72. https://doi.org/10.1044/1092-4388(2011/10-0357).
Hamlet S, et al. “Normal adult swallowing of liquid and viscous material: scintigraphic data on bolus transit and oropharyngeal residues,” (in eng). Dysphagia. 1996;11(1):41–7. https://doi.org/10.1007/BF00385799.
Hiss SG, Strauss M, Treole K, Stuart A, Boutilier S. Effects of age, gender, bolus volume, bolus viscosity, and gustation on swallowing apnea onset relative to lingual bolus propulsion onset in normal adults. J Speech Lang Hear Res. 2004;47(3):572–83. https://doi.org/10.1044/1092-4388(2004/044).
Iguchi T, Ohkubo M, Sugiyama T, Hori K, Ono T, Ishida R. Effects of water viscosity and tongue ingestion site on tongue pressure during food bolus propulsion. J Oral Rehabil. 2018;45(5):371–7. https://doi.org/10.1111/joor.12623.
Humbert IA, et al. “Swallowing kinematic differences across frozen, mixed, and ultrathin liquid boluses in healthy adults: age, sex, and normal variability,” (in eng). J Speech Lang Hear Res. 2018;61(1558–9102):1544–59. https://doi.org/10.1044/2018_JSLHR-S-17-0417.
Inamoto Y, et al. "The effect of bolus viscosity on laryngeal closure in swallowing: kinematic analysis using 320-row area detector CT. Dysphagia. 2013;28(1):33–42. https://doi.org/10.1007/s00455-012-9410-4.
Larsson V, Torisson G, Bulow M, Londos E. Effects of carbonated liquid on swallowing dysfunction in dementia with Lewy bodies and Parkinson’s disease dementia (in English). Clin Interv Aging. 2017;12:1215–22. https://doi.org/10.2147/cia.s140389.
Kuhlemeier KV, Palmer J, Fau-Rosenberg D, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia. 2001. https://doi.org/10.1007/s004550011003.
Leder S, Judson B, Sliwinski E, Madson L. Promoting safe swallowing when puree is swallowed without aspiration but thin liquid is aspirated: nectar is enough. Dysphagia. 2013;28(1):58–62. https://doi.org/10.1007/s00455-012-9412-2.
Lee S, Yoo J, Kim M, Ryu J. Changes of timing variables in swallowing of boluses with different viscosities in patients with dysphagia. Arch Phys Med Rehabil. 2013;94(1):120–6. https://doi.org/10.1016/j.apmr.2012.07.016.
Leonard R, White C, McKenzie S, Belafsky P. Effects of bolus rheology on aspiration in patients with Dysphagia. J Acad Nutr Diet. 2014;114(4):590–4. https://doi.org/10.1016/j.jand.2013.07.037.
Miller JL, Watkin KL. The influence of bolus volume and viscosity on anterior lingual force during the oral stage of swallowing. Dysphagia. 1996;11(2):117–24. https://doi.org/10.1007/BF00417901.
Nagy A, Molfenter SM, Péladeau-Pigeon M, Stokely S, Steele CM. The effect of bolus consistency on hyoid velocity in healthy swallowing. Dysphagia. 2015;30(4):445–51. https://doi.org/10.1007/s00455-015-9621-6.
Okuno K, Tachimura T, Sakai T. Influences of swallowing volume and viscosity on regulation of levator veli palatini muscle activity during swallowing. J Oral Rehabil. 2013;40(9):657–63. https://doi.org/10.1111/joor.12071.
Omari TI, Dejaeger E, Fau-Tack J, Fau-Van Beckevoort D, Fau-Rommel N, Rommel N. “Effect of bolus volume and viscosity on pharyngeal automated impedance manometry variables derived for broad Dysphagia patients,” (in eng). Dysphagia. 2012;28(1432–0460):146–52. https://doi.org/10.1007/s00455-012-9423-z.
Reimers-Neils L, Logemann J, Larson C. “Viscosity effects on EMG activity in normal swallow,” (in eng). Dysphagia. 1994;9(2):101–6. https://doi.org/10.1007/BF00714596.
Rofes L, Arreola V, Martin A, Clavé P. Natural capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut. 2013;62(9):1280–7. https://doi.org/10.1136/gutjnl-2011-300753.
Steele C, Bailey G, Molfenter S. “Tongue pressure modulation during swallowing: water versus nectar-thick liquids,” (in eng). J Speech Lang Hear Res. 2010;53(2):273–83. https://doi.org/10.1044/1092-4388(2009/09-0076).
Steele CM, Molfenter SM, Peladeau-Pigeon M, Polacco RC, Yee C. Variations in tongue-palate swallowing pressures when swallowing xanthan gum-thickened liquids. Dysphagia. 2014;29(6):678–84. https://doi.org/10.1007/s00455-014-9561-6.
Steele C, et al. “Reference values for healthy swallowing across the range from thin to extremely thick liquids,” (in eng). J Speech Lang Hear Res. 2019;62(5):1338–63. https://doi.org/10.1044/2019_jslhr-s-18-0448.
Steele C, et al. “Modulation of tongue pressure according to liquid flow properties in healthy swallowing,” (in eng). J Speech Lang Hear Res. 2019;62(1):22–33. https://doi.org/10.1044/2018_jslhr-s-18-0229.
Steele C, Van Lieshout P. Influence of bolus consistency on lingual behaviors in sequential swallowing. Dysphagia. 2004;19(3):192–206. https://doi.org/10.1007/s00455-004-0006-5.
Vilardell N, Rofes L, Arreola V, Speyer R, Clave P. A comparative study between modified starch and xanthan gum thickeners in post-stroke oropharyngeal Dysphagia. Dysphagia. 2016;31(2):169–79. https://doi.org/10.1007/s00455-015-9672-8.
Tsuzuki H, et al. “Effects of bolus consistency and reclining position on kinematic swallowing events in analysis using 320-row area detector computed tomography,” (in eng). J Oral Sci. 2020;62(1880–4926):18–22. https://doi.org/10.2334/josnusd.18-0377.
Wu S, et al. “Effect of changes in bolus viscosity on swallowing muscles in patients with dysphagia after stroke,” (in eng). Chin Med J (Engl). 2018;131(23):2868–70. https://doi.org/10.4103/0366-6999.246071.
Bogaardt H, Burger J, Fokkens W, Bennink R. Viscosity is not a parameter of postdeglutitive pharyngeal residue: quantification and analysis with scintigraphy. Dysphagia. 2007;22(2):145–9. https://doi.org/10.1007/s00455-006-9069-9.
Butler S, Postma G, Fischer E. Effects of viscosity, taste, and bolus volume on swallowing apnea duration of normal adults. Otolaryngol Head Neck Surg. 2004;131(6):860–3. https://doi.org/10.1016/j.otohns.2004.06.706.
Kim C, Hsu J, O’Connor M, Weaver A, Brown M, Zinsmeister A. Effect of viscosity on oropharyngeal and esophageal emptying in man. Dig Dis Sci. 1994;39(1):189–92. https://doi.org/10.1007/bf02090081.
Lazarus C, et al. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Archiv Phys Med Rehabil. 1993;74(10):1066–70. https://doi.org/10.1016/0003-9993(93)90063-G.
Ferris L, et al. Modulation of pharyngeal swallowing by bolus volume and viscosity. Am J Physiol Gastroint Liver Physiol. 2020;320(1):G43–53. https://doi.org/10.1152/ajpgi.00270.2020.
Gozzer M, Cola P, Onofri S, Merola B, Silva R. Fiberoptic endoscopic findings of oropharyngeal swallowing of different food consistencies in amyotrophic lateral sclerosis. CoDAS. 2020. https://doi.org/10.1590/2317-1782/20192018216.
Ito Y, et al. The effect of bolus consistency on pharyngeal volume during swallowing: kinematic analysis in three dimensions using dynamic Area Detector CT. J Oral Rehabil. 2020;47(10):1287–96. https://doi.org/10.1111/joor.13062.
Ortega O, et al. “Therapeutic effect, rheological properties and α-amylase resistance of a new mixed starch and xanthan gum thickener on four different phenotypes of patients with oropharyngeal dysphagia,” (in eng). Nutrients. 2020;12(6):1873. https://doi.org/10.3390/nu12061873.
Castell JA, Dalton C, Fau-Castell DO, Castell DO. Effects of body position and bolus consistency on the manometric parameters and coordination of the upper esophageal sphincter and pharynx. Dysphagia. 1990. https://doi.org/10.1007/BF02412685.
Mendell D, Logemann J. Temporal sequence of swallow events during the oropharyngeal swallow. J Speech Lang Hear Res. 2007;50(5):1256–71. https://doi.org/10.1044/1092-4388(2007/088).
Mozzanica F, et al. Effect of age, sex, bolus volume, and bolus consistency on whiteout duration in healthy subjects during FEES. Dysphagia. 2019;34(2):192–200. https://doi.org/10.1007/s00455-018-9961-0.
Dantas RO, Dodds WJ. Effect of bolus volume and consistency on swallow-induced submental and infrahyoid electromyographic activity. Braz J Med Biol Res. 1990;23(1):37–44.
Miura Y, Morita Y, Koizumi H, Shingai T. Effects of taste solutions, carbonation, and cold stimulus on the power frequency content of swallowing submental surface electromyography. Chem Senses. 2009;34(4):325–31. https://doi.org/10.1093/chemse/bjp005.
Leow LP, Huckabee ML, Sharma S, Tooley TP. The influence of taste on swallowing apnea, oral preparation time, and duration and amplitude of submental muscle contraction. Chem Senses. 2007;32(2):119–28. https://doi.org/10.1093/chemse/bjl037.
Pelletier CA, Dhanaraj GE. “The effect of taste and palatability on lingual swallowing pressure,” (in eng). Dysphagia. 2006;21:121–8. https://doi.org/10.1007/s00455-006-9020-0.
Nagy A, Steele CM, Pelletier CA. Differences in swallowing between high and low concentration taste stimuli. Biomed Res Int. 2014;2014:813084–813084. https://doi.org/10.1155/2014/813084.
Regan J. “Impact of sensory stimulation on pharyngo-esophageal swallowing biomechanics in adults with dysphagia: a high-resolution manometry study,” (in eng). Dysphagia. 2020;35(1432–0460):825–33. https://doi.org/10.1007/s00455-019-10088-9.
Gatto AR, et al. Sour taste and cold temperature in the oral phase of swallowing in patients after stroke. CoDAS. 2013;25(2):163–8. https://doi.org/10.1590/s2317-17822013000200012.
Gatto AR, Cola PC, Da Silva RG, Ribeiro PW, Spadotto AA, et al. Influence of thermal and gustatory stimulus in the initiation of the pharyngeal swallow and bolus location instroke. J Stroke Cerebrovasc Dis. 2021;30(4):105349.
Oh E, Jee S, Kim B, Lee J, Cho K, Ahn S. A new swallowing supplement for dysphagia in patients with Parkinson’s disease. Neurol Sci. 2021;42(5):1949–58. https://doi.org/10.1007/s10072-020-04730-w.
Wahab NA, Jones RD, Huckabee M-L. Effects of olfactory and gustatory stimuli on the biomechanics of swallowing. Physiol Behav. 2011;102(5):485–90. https://doi.org/10.1016/j.physbeh.2010.11.030.
Morishita M, Mori S, Yamagami S, Mizutani M. Effect of carbonated beverages on pharyngeal swallowing in young individuals and elderly inpatients. Dysphagia. 2014;29(2):213–22. https://doi.org/10.1007/s00455-013-9493-6.
Moritaka H, et al. Effect of carbon dioxide in carbonated drinks on linguapalatal swallowing pressure. Chem Senses. 2014;39(2):133–42. https://doi.org/10.1093/chemse/bjt062.
Sonja S-K, et al. Effect of capsaicinoids on neurophysiological, biochemical, and mechanical parameters of swallowing function. Neurotherapeutics. 2021;18(2):1360–70. https://doi.org/10.1007/s13311-020-00996-2.
Pelletier CA, Steele CM. Influence of the perceived taste intensity of chemesthetic stimuli on swallowing parameters given age and genetic taste differences in healthy adult women. J Speech Lang Hear Res. 2014;57(1):46–56. https://doi.org/10.1044/1092-4388(2013/13-0005).
Krival K, Bates C. Effects of club soda and ginger brew on linguapalatal pressures in healthy swallowing. Dysphagia. 2012;27(2):228–39. https://doi.org/10.1007/s00455-011-9358-9.
Pelletier CA, Lawless HT, Pelletier CA, Lawless HT. Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Dysphagia. 2003;18(4):231–41. https://doi.org/10.1007/s00455-003-0013-y.
Logemann J, Pauloski B, Colangelo L, Lazarus C, Fujiu M, Kahrilas P. “Effects of a sour bolus on oropharyngeal swallowing measures in patients with neurogenic dysphagia,” (in eng). J Speech Hear Res. 1995;38(3):556–63. https://doi.org/10.1044/jshr.3803.556.
Dietsch AM, Westemeyer RM, Pearson WG, Schultz DH. Genetic taster status as a mediator of neural activity and swallowing mechanics in healthy adults. Front Neurosci Original Res 2019;13
Sdravou K, Walshe M, Dagdilelis L. Effects of carbonated liquids on oropharyngeal swallowing measures in people with neurogenic dysphagia. Dysphagia. 2012;27(2):240–50. https://doi.org/10.1007/s00455-011-9359-8.
Yael S-G, et al. Effects of carbonation of liquids on penetration–aspiration and residue management. Eur Arch Oto-Rhino-Laryngol. 2021;278(12):4871–81. https://doi.org/10.1007/s00405-021-06987-z.
Perlman A, Schultz J, VanDaele D. Effects of age, gender, bolus volume, and bolus viscosity on oropharyngeal pressure during swallowing. J Appl Physiol. 1993;75(1):33–7. https://doi.org/10.1152/jappl.1993.75.1.33.
Alves L, Secaf M, Dantas R. Effect of a bitter bolus on oral, pharyngeal and esophageal transit of healthy subjects. Arq Gastroenterol. 2013. https://doi.org/10.1590/s0004-28032013000100007.
Alves L, Secaf M, Dantas R. Oral, pharyngeal, and esophageal transit of an acidic bolus in healthy subjects. Esophagus. 2013;10(4):217–22. https://doi.org/10.1007/s10388-013-0389-1.
Alves L, Fabio S, Dantas R. Efeito do Sabor no Trânsito Oral e Faríngeo de Pacientes com Acidente Vascular Cerebral. Revista Neurociências. 2014;22(1):17–21.
Miyaoka Y, Haishima K, Takagi M, Haishima H, Asari J, Yamada Y. Influences of thermal and gustatory characteristics on sensory and motor aspects of swallowing. Dysphagia. 2006;21(1):38–48. https://doi.org/10.1007/s00455-005-9003-6.
Lee K, et al. The influence of sour taste on Dysphagia in brain injury: blind study. Ann Rehabil Med. 2012;36(3):365–70. https://doi.org/10.5535/arm.2012.36.3.365.
Dietsch A, Dorris H, Pearson WJ, Dietrich-Burns K, Solomon N. Taste manipulation and swallowing mechanics in trauma-related sensory-based Dysphagia. J Speech Lang Hear Res. 2019;62(8):2703–12. https://doi.org/10.1044/2019_jslhr-s-18-0381.
Turkington L, Ward EC, Farrell A, Porter L, Wall LR. Impact of carbonation on neurogenic dysphagia and an exploration of the clinical predictors of a response to carbonation. Int J Lang Commun Disord. 2019;54(3):499–513. https://doi.org/10.1111/1460-6984.12458.
Park H, Kim D, Lee S, Park K. “The effect of aging on mastication and swallowing parameters according to the hardness change of solid food,” (in eng). J Texture Stud. 2017;48(5):362–9. https://doi.org/10.1111/jtxs.12249.
Dantas R, et al. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258(5 Pt 1):G675–81. https://doi.org/10.1152/ajpgi.1990.258.5.G675.
Pauloski BR, et al. “Effects of enhanced bolus flavors on oropharyngeal swallow in patients treated for head and neck cancer,” (in eng). Head Neck. 2013;35(8):1124–31. https://doi.org/10.1002/hed.23086.
Yokoyama S, et al. Tongue pressure modulation for initial gel consistency in a different oral strategy. PLoS ONE. 2014. https://doi.org/10.1371/journal.pone.0091920.
Sugita K, Inoue M, Taniguchi H, Ootaki S, Igarashi A, Yamada Y. Effects of food consistency on tongue pressure during swallowing. J Oral Biosci. 2006;48(4):278–85. https://doi.org/10.1016/S1349-0079(06)80010-1.
Iida Y, Katsumata A, Fujishita M. “Videofluorographic evaluation of mastication and swallowing of Japanese udon noodles and white rice,” (in eng). Dysphagia. 2011;26(3):246–9. https://doi.org/10.1007/s00455-010-9295-z.
Palmer P, McCulloch T, Jaffe D, Neel A. “Effects of a sour bolus on the intramuscular electromyographic (EMG) activity of muscles in the submental region,” (in eng). Dysphagia. 2005;20(3):210–7. https://doi.org/10.1007/s00455-005-0017-x.
Igarashi A, et al. “Sensory and motor responses of normal young adults during swallowing of foods with different properties and volumes,” (in eng). Dysphagia. 2010;25(3):198–206. https://doi.org/10.1007/s00455-009-9243-y.
Kendall KA, Leonard RJ, Fau-McKenzie SW, McKenzie SW. “Accommodation to changes in bolus viscosity in normal deglutition: a videofluoroscopic study,” (in eng). Ann Otol Rhinol Laryngol. 2001;110(0003–4894):1059–65. https://doi.org/10.1177/000348940111001113.
Moritaka H, Nakazawa F. The rheological and swallowing properties of rice starch. Food Sci Technol Res. 2009;15(2):133–40. https://doi.org/10.3136/fstr.15.133.
Cola P, et al. “Taste and temperature in swallowing transit time after stroke,” (in eng). Cerebrovasc Dis Extra. 2012;2(1):45–51. https://doi.org/10.1159/000339888.
Cola PC, Gatto AR, Silva RG, Spadotto AA, Schelp AO, Henry MA. “The influence of sour taste and cold temperature in pharyngeal transit duration in patients with stroke,” (in eng). Arq Gastroenterol. 2010;47(1):18–21. https://doi.org/10.1590/S0004-28032010000100004.
Friedman L, DeMets D, Reboussin D, Granger C. Fundamentals of clinical trials. 5th ed. Switzerland: Springer; 2015.
Martino R, McCulloch T. Therapeutic intervention in oropharyngeal dysphagia. Nat Rev Gastroenterol Hepatol Rev. 2016;13(11):665–79. https://doi.org/10.1038/nrgastro.2016.127.
Sterne JAC, Elbers RG. Reeves BC and the development group for ROBINS-I, Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I): detailed guidance. 12 October 2016.
Baijens L, et al. “European Society for Swallowing Disorders European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome,” (in English). Clin Interv Aging Rev. 2016;11:1403–28.
Chen DF. Dysphagia in the hospitalized patient. Hosp Med Clin. 2017;6(1):38–52. https://doi.org/10.1016/j.ehmc.2016.07.004.
Clave P, et al. “Pathophysiology, relevance and natural history of oropharyngeal dysphagia among older people,” (in eng). Nestle Nutr Inst Workshop Ser. 2012;72:57–66. https://doi.org/10.1159/000339986.
Krekeler BN, Broadfoot CK, Johnson S, Connor NP, Rogus-Pulia N. Patient adherence to dysphagia recommendations: a systematic review. Dysphagia. 2018;33(2):173–84. https://doi.org/10.1007/s00455-017-9852-9.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7. https://doi.org/10.1016/S0140-6736(07)61602-X.
Collaborative S. STARTED (Standards for Rigor and Transparency in Dysphagia Research). https://dysphagia-standards.netlify.app/app/. Accessed 2 Oct 2022.
Cho H-M, Yoo W, Yoo B. “Effect of NaCl addition on rheological behaviors of commercial gum-based food thickener used for dysphagia diets,” (in eng). Prev Nutr Food Sci. 2015;20(2):137–42. https://doi.org/10.3746/pnf.2015.20.2.137.
Vickers Z, et al. “Relationships among rheological, sensory texture, and swallowing pressure measurements of hydrocolloid-thickened fluids,” (in eng). Dysphagia. 2015;30(6):702–13. https://doi.org/10.1007/s00455-015-9647-9.
Steffe J. Rheological methods in food process engineering. 2nd ed. East Lansing: Freeman Press; 1996.
Sugino S, Tsukada T, Ootaki S, Yuka K, Yamada Y, Inoue M. Effects of food consistency and subject’s posture on the electromyographic activity in the genioglossus muscle in humans. Jpn Soc Stomatognath Funct. 2007;14:13–23.
Sanpei R, et al. “Video-endoscopic comparison of swallowing waxy rice mochi and waxy wheat mochi: improvement of a traditional Japanese food that presents a choking hazard,” (in eng). Biosci Biotechnol Biochem. 2014;78(1347–6947):472–7. https://doi.org/10.1080/09168451.2014.877817.
Yamada T, Matsuo K, Izawa M, Yamada S, Masuda Y, Ogasawara T. “Effects of age and viscosity on food transport and breathing-swallowing coordination during eating of two-phase food in nursing home residents,” (in eng). Geriatr Gerontol Int. 2017;17(11):2171–7. https://doi.org/10.1111/ggi.13056.
Kuhlemeier KV, Palmer JB, Rosenberg D. “Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients,” (in eng). Dysphagia. 2001;16(2):119–22. https://doi.org/10.1007/s004550011003.Dysphagia.
Steele C, van Lieshout P, Pelletier C. The influence of stimulus taste and chemesthesis on tongue movement timing in swallowing. J Speech Lang Hear Res. 2012;55(1):262–75. https://doi.org/10.1044/1092-4388(2011/11-0012).
Dafiah P, Swapna N. Variations in the amplitude and duration of hyolaryngeal elevation during swallow: effect of sour and carbonated liquid bolus. Physiol Behav. 2020;224:113028. https://doi.org/10.1016/j.physbeh.2020.113028.
Funding
Funding was provided by Beca Igualdad de Oportunidades Fulbright-ANID (BECAS/DOCTORADO EXTRANJERO/56150014) and National Institutes of Health (1K76AG068590).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peña-Chávez, R.E., Schaen-Heacock, N.E., Hitchcock, M.E. et al. Effects of Food and Liquid Properties on Swallowing Physiology and Function in Adults. Dysphagia 38, 785–817 (2023). https://doi.org/10.1007/s00455-022-10525-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10525-2