Abstract
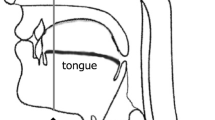
Muscle strength and function are generally positively correlated with muscle quantity and negatively correlated with muscle quality; however, the tongue shows a unique tendency, different from limb muscles. The relationship between the characteristics of each part of the tongue, muscle strength and function, and systemic factors has been unclear. The aim of the study was to investigate the relationship between cross-sectional area (CSA) and echo intensity (EI) of the middle and base of the tongue and swallowing, articulation function, and body composition. Eighty-nine healthy individuals were included in this cross-sectional study. Swallowing was assessed using tongue pressure (TP) and jaw opening force (JOF) as they indicate swallowing-related muscle strength. Articulation function was evaluated through oral diadochokinesis (ODK). Bioelectrical impedance analysis was performed for body composition. CSAs and EIs of the middle and base of the tongue were measured using ultrasound. Multiple regression analysis was used to examine the relationship between the characteristics of the tongue, swallowing-related muscle strength, and ODK. In multiple regression analysis with TP as the dependent variable, age (β = − 0.22, P < 0.01) and CSA of the middle part (β = 0.02, P < 0.01) were significant explanatory variables. In multiple regression analysis with JOF as the dependent variable, sex (β = − 2.76, P < 0.01) and CSA of the base (β = − 0.004, P < 0.05) were significant explanatory variables. Multiple regression analysis with articulation function as the dependent variable did not yield significant results. The CSA of the tongue is a better indicator of swallowing-related muscle strength than EI. Ultrasonography may be used for assessing swallowing-related muscle strength.


Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30:80–7. https://doi.org/10.1007/s00455-014-9577-y.
Rong P, Green JR. Predicting speech intelligibility based on spatial tongue-jaw coupling in persons with amyotrophic lateral sclerosis: the impact of tongue weakness and jaw adaptation. J Speech Lang Hear Res. 2019;62:3085–103. https://doi.org/10.1044/2018_JSLHR-S-CSMC7-18-0116.
van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C. Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J Dent Res. 2011;90:1398–404. https://doi.org/10.1177/0022034511422909.
Maresca G, Pranio F, Naro A, De Luca R, Maggio MG, Scarcella I, et al. Augmentative and alternative communication improves quality of life in the early stages of amyotrophic lateral sclerosis. Funct Neurol. 2019;34:35–43.
Kim AM, Keenan BT, Jackson N, Chan EL, Staley B, Poptani H, et al. Tongue fat and its relationship to obstructive sleep apnea. Sleep. 2014;37:1639–48. https://doi.org/10.5665/sleep.4072.
Bradley TD, Floras JS. Obstructive sleep apnea and its cardiovascular consequences. Lancet. 2009;373:82–93. https://doi.org/10.1016/S0140-6736(08)61622-0.
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–41. https://doi.org/10.1056/NEJMoa043104.
Yamaguchi K, Hara K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, et al. Ultrasonography shows age-related changes and related factors in the tongue and suprahyoid muscles. J Am Med Dir Assoc. 2021;22:766–72. https://doi.org/10.1016/j.jamda.2020.10.012.
Nashi N, Kang S, Barkdull GC, Lucas J, Davidson TM. Lingual fat at autopsy. Laryngoscope. 2007;117:1467–73. https://doi.org/10.1097/MLG.0b013e318068b566.
Ogawa N, Mori T, Fujishima I, Wakabayashi H, Itoda M, Kunieda K, et al. Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc. 2018;19:516–22. https://doi.org/10.1016/j.jamda.2017.11.007.
Biltz NK, Collins KH, Shen KC, Schwartz K, Harris CA, Meyer GA. Infiltration of intramuscular adipose tissue impairs skeletal muscle contraction. J Physiol. 2020;598:2669–83. https://doi.org/10.1113/JP279595.
Sanders I, Mu L, Amirali A, Su H, Sobotka S. The human tongue slows down to speak: muscle fibers of the human tongue. Anat Rec (Hoboken). 2013;296:1615–27. https://doi.org/10.1002/ar.22755.
Nakao Y, Yamashita T, Honda K, Katsuura T, Hama Y, Nakamura Y, et al. Association among age-related tongue muscle abnormality, tongue pressure, and presbyphagia: a 3D MRI study. Dysphagia. 2021;36:483–91. https://doi.org/10.1007/s00455-020-10165-4.
International Phonetic Association. Handbook of the international phonetic association: a guide to the use of the international phonetic alphabet. Cambridge: Cambridge University Press; 1999.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707. https://doi.org/10.1016/j.pmr.2008.06.001.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), the Extended Group for EWGSOP2, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. https://doi.org/10.1093/ageing/afy169.
Young HJ, Jenkins NT, Zhao Q, Mccully KK. Measurement of intramuscular fat by muscle echo intensity. Muscle Nerve. 2015;52:963–71. https://doi.org/10.1002/mus.24656.
Chantaramanee A, Tohara H, Nakagawa K, Hara K, Nakane A, Yamaguchi K, et al. Association between echo intensity of the tongue and its thickness and function in elderly subjects. J Oral Rehabil. 2019;46:634–9. https://doi.org/10.1111/joor.12788.
Mori T, Wakabayashi H, Ogawa N, Fujishima I, Oshima F, Itoda M, et al. The mass of geniohyoid muscle is associated with maximum tongue pressure and tongue area in patients with sarcopenic dysphagia. J Nutr Health Aging. 2021;25:356–60. https://doi.org/10.1007/s12603-020-1528-8.
Namiki C, Hara K, Tohara H, Kobayashi K, Chantaramanee A, Nakagawa K, et al. Tongue-pressure resistance training improves tongue and suprahyoid muscle functions simultaneously. Clin Interv Aging. 2019;14:601–8. https://doi.org/10.2147/CIA.S194808.
Kletzien H, Russell JA, Leverson GE, Connor NP. Differential effects of targeted tongue exercise and treadmill running on aging tongue muscle structure and contractile properties. J Appl Physiol (1985). 2013;114:472–81. https://doi.org/10.1152/japplphysiol.01370.2012.
Nagano A, Maeda K, Koike M, Murotani K, Ueshima J, Shimizu A, et al. Effects of physical rehabilitation and nutritional intake management on improvement in tongue strength in sarcopenic patients. Nutrients. 2020;12:3104. https://doi.org/10.3390/nu12103104.
Yamaguchi K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, et al. Tohara H. Age-related changes in swallowing muscle intramuscular adipose tissue deposition and related factors. Exp Gerontol. 2021;153:111505. https://doi.org/10.1016/j.exger.2021.111505.
Yoshimi K, Hara K, Tohara H, Nakane A, Nakagawa K, Yamaguchi K, et al. Relationship between swallowing muscles and trunk muscle mass in healthy elderly individuals: a cross-sectional study. Arch Gerontol Geriatr. 2018;79:21–6. https://doi.org/10.1016/j.archger.2018.07.018.
Low S, Ng TP, Lim CL, Moh A, Ang SF, Wang J, et al. Association between lower extremity skeletal muscle mass and impaired cognitive function in type 2 diabetes. Sci Rep. 2020;10:2956. https://doi.org/10.1038/s41598-020-59914-3.
Hara K, Tohara H, Wada S, Iida T, Ueda K, Ansai T. Jaw-opening force test to screen for Dysphagia: preliminary results. Arch Phys Med Rehabil. 2014;95:867–74. https://doi.org/10.1016/j.apmr.2013.09.005.
Sarukawa S, Noguchi T, Miyazaki K, Itoh H, Nishino H, Kusama M. Development of a tool for speech intelligibility evaluation after glossectomy: the TKR speech test. Jpn J Head Neck Cancer. 2013;39:374–8.
Utanohara Y, Hayashi R, Yoshikawa M, Yoshida M, Tsuga K, Akagawa Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia. 2008;23:286–90. https://doi.org/10.1007/s00455-007-9142-z.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. https://doi.org/10.1037//0033-2909.86.2.420.
Nakamori M, Imamura E, Fukuta M, Tachiyama K, Kamimura T, Hayashi Y, et al. Tongue thickness measured by ultrasonography is associated with tongue pressure in the Japanese elderly. PLoS ONE. 2020;15: e0230224. https://doi.org/10.1371/journal.pone.0230224.
Kajisa E, Tohara H, Nakane A, Wakasugi Y, Hara K, Yamaguchi K, et al. The relationship between jaw-opening force and the cross-sectional area of the suprahyoid muscles in healthy elderly. J Oral Rehabil. 2018;45:222–7. https://doi.org/10.1111/joor.12596.
Baril AA, Carrier J, Lafrenière A, Warby S, Poirier J, Osorio RS, Canadian Sleep and Circadian Network, et al. Biomarkers of dementia in obstructive sleep apnea. Sleep Med Rev. 2018;42:139–48. https://doi.org/10.1016/j.smrv.2018.08.001.
Cadore EL, Izquierdo M, Conceição M, Radaelli R, Pinto RS, Baroni BM, et al. Echo intensity is associated with skeletal muscle power and cardiovascular performance in elderly men. Exp Gerontol. 2012;47:473–8. https://doi.org/10.1016/j.exger.2012.04.002.
Sanders I, Mu L. A three-dimensional atlas of human tongue muscles. Anat Rec (Hoboken). 2013;296:1102–14. https://doi.org/10.1002/ar.22711.
Mizuno T, Matsui Y, Tomida M, Suzuki Y, Nishita Y, Tange C, et al. Differences in the mass and quality of the quadriceps with age and sex and their relationships with knee extension strength. J Cachexia Sarcopenia Muscle. 2021;12:900–12. https://doi.org/10.1002/jcsm.12715.
Lopez P, Pinto MD, Pinto RS. Does rest time before ultrasonography imaging affect quadriceps femoris muscle thickness, cross-sectional area and echo intensity measurements? Ultrasound Med Biol. 2019;45:612–6. https://doi.org/10.1016/j.ultrasmedbio.2018.10.010.
Acknowledgements
The authors would like to thank Editage for editing and proofreading this manuscript for English language and all staff members and participants of the study.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
KY involved in conceptualization, methodology, formal analysis, writing-original draft, review, and editing. KN participated in validation, data curation, writing-review, and editing. KY and CA took part in investigation, data curation, and resources. AN and TO did formal analysis and resources. HT contributed in supervision, project administration, writing-review, and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This study was approved by the Tokyo Medical and Dental University Ethics Committee (Ref: D2014-047).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamaguchi, K., Nakagawa, K., Yoshimi, K. et al. The Cross-Sectional Area of the Middle and Base of the Tongue is Associated with Swallowing-Related Muscle Strength. Dysphagia 37, 1723–1731 (2022). https://doi.org/10.1007/s00455-022-10431-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10431-7