Abstract
Purpose
Immune checkpoint inhibitors (ICIs) are ineffective against epidermal growth factor receptor (EGFR)-mutant non-small cell lung cancer (NSCLC). This study aimed to investigate the clinical characteristics of patients who were treated or not treated with ICIs, and of those who benefit from immunotherapy in EGFR-mutant NSCLC.
Methods
We analyzed patients with unresectable stage III/IV or recurrent NSCLC harboring EGFR mutations using a prospective umbrella-type lung cancer registry (CS-Lung-003).
Results
A total of 303 patients who met the eligibility criteria were analyzed. The median age was 69 years; 116 patients were male, 289 had adenocarcinoma, 273 had major mutations, and 67 were treated with ICIs. The duration of EGFR-TKI treatment was longer in the Non-ICI group than in the ICI group (17.1 vs. 12.7 months, p < 0.001). Patients who received ICIs for more than 6 months were categorized into the durable clinical benefit (DCB) group (24 patients), and those who received ICIs for less than 6 months into the Non-DCB group (43 patients). The overall survival in the DCB group exhibited longer than the Non-DCB group (69.3 vs. 47.1 months), and an equivalent compared to that in the Non-ICI group (69.3 vs. 68.9 months). Multivariate analysis for time to next treatment (TTNT) of ICIs showed that a poor PS was associated with a shorter TTNT [hazard ratio (HR) 3.309; p < 0.001]. Patients who were treated with ICIs and chemotherapy combination were associated with a longer TTNT (HR 0.389; p = 0.003). In addition, minor EGFR mutation was associated with a long TTNT (HR 0.450; p = 0.046).
Conclusion
ICIs were administered to only 22% of patients with EGFR-mutated lung cancer, and they had shorter TTNT of EGFR-TKI compared to other patients. ICI treatment should be avoided in EGFR mutated lung cancer with poor PS but can be considered for lung cancer with EGFR minor mutations. Pathological biomarker to predict long-term responders to ICI are needed.
Similar content being viewed by others
Introduction
Lung cancer is the leading cause of cancer-related deaths worldwide (Sung et al. 2021). Epidermal growth factor receptor (EGFR) mutations account for 50–60% of driver oncogenes of lung adenocarcinomas in individuals of the East Asian ethnicity or never smokers (Shigematsu H et al. 2005). EGFR tyrosine kinase inhibitors (EGFR-TKIs) provide a survival benefit in EGFR-mutant non-small-cell lung cancer (NSCLC) (Ohashi et al. 2013; Soria et al. 2018). However, the inhibitory effect of EGFR-TKIs is transient and disease progression is inevitable owing to the acquisition of resistance (Passaro et al. 2021).
Immune checkpoint inhibitors (ICIs) such as programmed cell death-1 and anti-programmed death-ligand 1 (PD-L1) inhibitors prolong the overall survival (OS) of patients with lung cancer (Ferrara et al. 2021; Zhou et al. 2020). However, they have a limited effect on EGFR-mutant NSCLCs (Lee et al. 2018). In contrast, ICIs occasionally exert sustained tumor inhibition in some EGFR-mutant lung cancers (Garassino et al. 2018; Watanabe et al. 2019). The characteristics of patients who may benefit from ICIs have not yet been fully established. Therefore, we aimed to compare the clinical characteristics of ICI-treated and non-treated patients with EGFR-mutant lung cancers and to investigate the characteristics of those who benefited from immunotherapy in a prospective registry cohort of NSCLC.
Materials and methods
Patients and study design
This observational study was registered at the prospective umbrella-type lung cancer registry (CS-Lung-003; UMIN000026696) (Nishii et al. 2021; Kudo et al. 2022) and included patients with lung cancer enrolled from 31 collaborating hospitals between July 2017 and September 2020. This study aimed to investigate clinical practice patterns and treatment efficacy in patients with EGFR-mutant lung cancer. Data for this study were collected in August 2021. This study was approved by the ethics committee of the participating hospital (no. 1703–055; Institutional Review Board of Okayama University Hospital) and all patients provided written informed consent.
Patient eligibility
This study included patients with unresectable stage III/IV lung cancer harboring EGFR mutations without indications for radical radiotherapy or with recurrent EGFR-mutant NSCLC. We excluded patients with an observation period of less than 6 months or unknown outcome. EGFR mutations were assessed using a test approved by the Pharmaceuticals and Medical Devices Agency of Japan. We defined the EGFR exon 19 deletion and EGFR L858R as major mutations, and the other types as minor mutations. We categorized patients treated with ICIs for more than 6 months in the “durable clinical benefit (DCB)” group, and those treated with ICIs for less than 6 months in the “Non-DCB” group (Rizvi NA et al. 2015). Patients treated with ICIs for more than 2 years were considered as “long-term responders” (von Pawel J et al. 2019).
Outcomes
The primary outcome was the OS, compared between the ICI and Non-ICI groups. Secondary outcomes were the frequency of ICI use in EGFR lung cancer, OS in the DCB and Non-DCB groups, and clinical factors correlated with time to next treatment (TTNT) for immunotherapy. TTNT was calculated from the date of initiation of EGFR-TKI or ICI therapy to the date of next treatment or death due to any cause (Kehl et al. 2021). OS was calculated from the date of initiation of first-line anti-cancer therapy to the date of death or the last follow-up.
Statistical analyses
Patient characteristics were assessed using Fisher’s exact test. The Kaplan–Meier method was used for analysis of TTNT and OS. TTNT for EGFR-TKI or ICI therapy and OS were assessed using the log-rank test. Univariate and multivariate analyses were performed using a Cox proportional hazards model to evaluate the factors associated with the duration of ICI treatment. A multivariate analysis was conducted using the stepwise method, with threshold p values for entering and removing variables (Eastern Cooperative Oncology Group performance status (PS), histology, type of EGFR mutation, treatment, sex, age, smoking history, and line of treatment) from the model as 0.05 and 0.20, respectively. All statistical analyses were performed using STATA software (version 17.0) (StataCorp, College Station, Texas, USA) and p values < 0.05 were considered statistically significant.
Results
Efficacy of EGFR-TKIs in EGFR-mutant lung cancer with/without immunotherapy
A total of 332 patients with stage III/IV disease harboring EGFR mutations without an indication for radical radiotherapy or surgery or with EGFR-mutant recurrent NSCLC were consecutively enrolled in this registry study from July 2017 to September 2020 (Fig. 1). Of these, 29 patients were excluded because of a short observation period (less than 6 months) (n = 19), lack of data (n = 7), or no therapy (n = 3). Of the remaining 303 patients, 67 (22%) were treated with ICIs, and 236 (78%) were not.
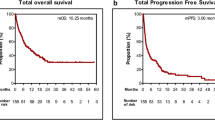
First, we analyzed the clinical characteristics of 303 patients (Table 1). The median patient age was 69 (range 26–98) years. Of the included patients, 38% were men, 59% were non-smokers, 95% had adenocarcinoma, and 84% had PS 0–1 at the initiation of systemic therapy. EGFR exon 19 deletion was observed in 55%, exon 21 L858R in 35%, and minor mutations in the remaining 10% patients. Initial use of EGFR-TKIs was as follows: the 1st generation (gefitinib and erlotinib) were used in 40% patients, 2nd generation (afatinib) in 33%, and 3rd generation (osimertinib) in 24%. 3% of all patients had never been treated with EGFR-TKIs. Then, we evaluated patient characteristics according to the provision of ICI treatment (Table 2). Compared with those in the ICI group, patients in the Non-ICI group were significantly more likely to be female and have brain metastases at diagnosis. There were no significant differences between age, the groups in stage, histology, PS, EGFR mutation type, liver metastasis, or smoking history. In addition, 4% in the ICI group and 2% in the non-ICI group never received EGFR-TKIs (p = 0.381). The duration of EGFR-TKI treatment was significantly shorter in the ICI group than in the Non-ICI group (median 12.7 vs. 17.1 months, p < 0.001) (Fig. 2a). Given that osimertinib showed superior effect than gefitinib or erlotinib (Soria et al. 2018), we excluded patients who were treated with osimertinib as initial EGFR-TKI (Supplementary Table 1), and assessed the TTNT of EGFR-TKI in patients treated with 1st or 2nd generation EGFR-TKIs as initial EGFR-TKI. The TTNT were still shorter in the ICI group than in the Non-ICI group (median 12.8 vs. 18.5 months, p < 0.001) (Supplementary Fig. 1a). In contrast, patients in the Non-ICI group tended to have a longer OS than those in the ICI group, in patients with or without osimertinib treatment, although the difference was not significant (median 68.9 vs. 61.9 months, p = 0.555) (Fig. 2b) (median 75.6 vs. 63.3 months, p = 0.364) (Supplementary Fig. 1b). Consequently, these results suggest that the duration of EGFR-TKI treatment is more important than the administration of ICI for a survival benefit in patients with EGFR mutated lung cancers.
Superior OS in the DCB than in the Non-DCB group in EGFR-mutant lung cancers
To examine the characteristics of patients who benefited from ICI treatment, we compared the DCB and Non-DCB groups. The DCB group included 36% (24/67) and the Non-DCB group included 64% (43/67) of patients treated with ICIs. The characteristics of each group are presented in Table 3. Comparing the DCB and Non-DCB groups, the DCB group had a better PS at ICI initiation, an earlier line of treatment (≤ third line), and a higher proportion of patients treated with chemotherapy and ICIs combination (ChemoIO). In contrast, there were no significant differences in age, sex, stage, histology, PS at the initiation of systemic therapy, type of EGFR mutation, smoking history, duration of EGFR-TKI treatment, or immune-related adverse events. The expression of PD-L1 was not examined in 71% of patients in the DCB group and 51% of those in the Non-DCB group. The types of minor EGFR mutations are as shown in Supplementary Table 2. For ChemoIO, the atezolizumab, bevacizumab, carboplatin and paclitaxel (ABCP) combination was the most commonly used (DCB group: 82%, Non-DCB group: 75%).
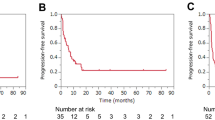
The TTNT for ICI monotherapy was 20.4 months in the DCB group and 2.4 months in the Non-DCB group (p < 0.001) (Fig. 3a). The TTNT for ChemoIO was 11.9 or 1.8 months in the DCB or Non-DCB group, respectively (p < 0.001) (Fig. 3b). The median OS was significantly longer in the DCB group than in the Non-DCB group (69.3 months vs. 47.1 months, p = 0.025) (Fig. 4) and was comparable to the Non-ICI group (Supplementary Fig. 2).
Kaplan–Meier curves for OS in the DCB and Non-DCB groups. TTNT time to next treatment, EGFR Epidermal growth factor receptor, TKI tyrosine kinase inhibitor, OS overall survival, ICI immune-checkpoint inhibitors, ChemoIO chemotherapy and ICIs combination, DCB durable clinical benefit, CI confidence interval, NE not evaluable
Impact of PS, ChemoIO, minor mutilations on TTNT for immunotherapy in EGFR-mutant lung cancers
Univariate and multivariate analyses were performed in 67 patients to assess the clinical factors associated with TTNT for immunotherapy in EGFR-mutant lung cancer (Table 4). In the univariate analyses, histology, EGFR mutation type, sex, age, and smoking history were not associated with TTNT for ICIs. PS 0–1 at ICI initiation, ChemoIO, and treatment line (≤ third line) were positively correlated with the TTNT for immunotherapy. Multivariate analyses revealed that PS 0–1 at ICI initiation, minor EGFR mutations, and ChemoIO had a positive correlation with TTNT.
Next, we examined the impact of these clinical factors on the OS of patients with EGFR-mutant lung cancer. Patients with PS 0–1 exhibited a superior OS than those with PS 2–4 (median 69.3 vs. 61.9 months, p = 0.005) (Supplementary Fig. 3a). Patients with the use of ChemoIO did not show a significant prolongation of OS compared to patients with ICI monotherapy (median: 63.3 vs. 49.0 months, p = 0.230) (Supplementary Fig. 3b). Patients with lung cancers harboring minor EGFR mutations showed a tendency of longer TTNT for ICIs (median 7.6 vs. 3.8 months, p = 0.133) than patients with major EGFR mutations. In contrast, the OS tended to be shorter in patients with minor EGFR mutations, but without statistical significance (median: 62.7 vs. 35.1 months, p = 0.636) (Supplementary Fig. 3c), again suggesting that the importance of EGFR-TKI duration for survival benefit in EGFR-mutated lung cancer (Supplementary Fig. 3d).
In our study, a long-term response (TTNT > 2 years) was observed in 4 patients (Table 5). All patients had a good PS (0–1). However, 3 of these 4 patients had a major EGFR mutation, and 3 of them were treated with ICI monotherapy. Additionally, ICI monotherapy was administered after 4th line therapy in 2 of the 3 patients. These results suggest the limitation of clinical characteristics to predict of long-term response induced by ICI in EGFR-mutant lung cancer.
Discussion
Few prospective observational studies have assessed the clinical characteristics of patients treated (ICI group) and not treated (Non-ICI group) with ICIs in EGFR-mutant lung cancer. This prospective observational study demonstrated that ICIs were administered to only 22% of patients, and they benefited less from initial use of EGFR-TKI regardless of 1st, 2nd or, 3rd generation, than those who were not treated with ICIs. It was thought that ICI might not yet be used because of the long duration of response to EGFR-TKI. In addition, the Non-ICI group did not show a significant prolongation of OS compared to the ICI group, but tended to have a superior OS. Previous studies revealed that a short duration of response to EGFR-TKIs correlated with benefit of ICI treatment in patients with EGFR-mutant lung cancers (Yoshida et al. 2018; Liu et al. 2021). However, our study revealed that the effect of ICI treatment does not neutralize the short duration of response to EGFR-TKIs, suggesting the importance of long-term response to EGFR-TKIs in terms of survival benefits in patients with EGFR-mutant lung cancer.
While the expected benefit of immunotherapy is limited in EGFR-mutant lung cancers, our study revealed that PS (0–1) was correlated with DCB of ICI therapies in EGFR-mutated lung cancers. PS is a well-known prognostic factor (Kawaguchi et al. 2010; Simmons et al. 2015). Therefore, it is challenging to evaluate the impact of PS on the efficacy of immunotherapy. Currently, multiple studies have reported the poor effect of ICI in patients with PS (Facchinetti et al. 2020; Miura et al. 2023). Given that these reports and the four cases of long-term response to immunotherapy (> 2 years) had good PS in our study, if treatment with ICIs is planned for EGFR-mutant lung cancer, it should be considered at least in patients who have maintained a good PS (0–1).
In this study, multivariate analysis showed that ChemoIO was a favorable factor for the prolongation of TTNT. Currently, several studies have failed to show the benefit of ChemoIO in EGFR-mutant lung cancers (Mok et al. 2022; Yang et al. 2023). In addition, ChemoIO with anti-angiogenic agents showed inconsistent and incompatible results in the same populations (Nogami et al. 2022; Zhou et al. 2023; Park et al. 2023). A subset analysis of the Impower150 trial indicated that ABCP may have a benefit on OS compared with bevacizumab plus carboplatin and paclitaxel chemotherapy in EGFR-mutant lung cancer (Nogami et al. 2022). This previous study may have prompted the administration of ABCP in patients with PS 0–1 in our cohort. However IMPOWER151 trial and ATTLAS trial failed to reproduce the benefit (Zhou et al. 2023; Park et al. 2023). Consistent with previous studies, our study also failed to show the significant prolongation of OS in the patients treated with ChemoIO compared with those without ChemoIO; thus, ChemoIO (including ABCP) is still not a standard treatment for EGFR-mutant lung cancer.
Consistent with previous reports (Yoshida et al. 2018), the TTNT of ICIs was superior in lung cancer with EGFR minor mutation than that with EGFR major mutation; however, the benefit in OS was inverse. This may be explained by the duration of administration of EGFR-TKIs because of the relatively worse effect of EGFR-TKIs in patients with EGFR minor mutation than in those with EGFR major mutation (Castellanos et al. 2017).
Patients with long-term response to immunotherapy (> 2 years) did not possess the clinical factors extracted by multivariate analysis in this study, suggesting a limitation in predicting the long-term response to immunotherapy using only clinical factors. A previous preclinical study revealed that oncogenic EGFR mutations play an important role in creating a non-inflamed tumor microenvironment (TME) (Nishii et al. 2022; Sugiyama et al. 2020) and that the expression of PD-L1 in cancer cells do not reproducibly predict the efficacy of ICI in EGFR-mutant lung cancer (Qiao et al. 2021). A previous report showed that cytotoxic T cells and the chemokines that recruit them are associated with the efficacy of ICIs in EGFR-mutant lung cancer (Hayashi et al. 2022), suggesting that some EGFR-lung cancers have an inflamed TME. Patients with lung cancer in the DCB group or long-term responders in our study may have such biological features. There is a strong need to establish biomarkers to identify effective populations for immunotherapy.
Our study has some limitations. First, eliminating registration and selection biases was difficult. Second, the number of factors for the multivariate analysis was limited because of the limited sample size. Third, data pertaining to PD-L1 expression, resistance mechanism to EGFR-TKI, or blood test results prior to ICI treatment were limited. In addition, the impact of co-occurring gene mutations such as TP53 mutations, which were reported to positively correlate with the effect with ICI (Dong et al. 2017; Sun et al. 2020), was not investigated in this study. Fourth, TTNT was used instead of PFS, which had a stronger correlation with OS, because it was difficult to obtain PFS for all the patients in this registry study. Therefore, we must carefully interpret our data for application in clinical practice. However, our study provides valuable real-world data regarding EGFR-mutant lung cancer.
In conclusion, our study demonstrates that patients treated with ICIs benefited less from EGFR-TKI treatment than those who were not treated with ICIs. In EGFR-lung cancer, it is difficult to predict the responder to ICI with OS prolongation based on clinical factors. Further studies to establish a biomarker based on the biological characteristics of EGFR-mutant lung cancers are warranted.
Data availability
The datasets generated and/or analyzed during the current study are potentially available from the corresponding author on reasonable request.
References
Castellanos E, Feld E, Horn L (2017) Driven by mutations: the predictive value of mutation subtype in EGFR- mutated non-small cell lung cancer. J Thorac Oncol 12(4):612–623. https://doi.org/10.1016/j.jtho.2016.12.014
Dong ZY, Zhong WZ, Zhang XC et al (2017) Potential predictive value of TP53 and KRAS mutation status for response to PD-1 blockade immunotherapy in lung adenocarcinoma. Clin Cancer Res 23(12):3012–3024. https://doi.org/10.1158/1078-0432.CCR-16-2554
Facchinetti F, Mazzaschi G, Barbieri F et al (2020) First-line pembrolizumab in advanced non-small cell lung cancer patients with poor performance status. Eur J Cancer 130:155–167. https://doi.org/10.1016/j.ejca.2020.02.023
Ferrara R, Imbimbo M, Malouf R et al (2021) Single or combined immune checkpoint inhibitors compared to first-line platinum-based chemotherapy with or without bevacizumab for people with advanced non-small cell lung cancer. Cochrane Database Syst Rev 4(4):CD013257. https://doi.org/10.1002/14651858.CD013257.pub3
Garassino MC, Cho BC, Kim JH et al (2018) Durvalumab as third-line or later treatment for advanced non-small-cell lung cancer (ATLANTIC): an open-label, single-arm, phase 2 study. Lancet Oncol 19(4):521–536. https://doi.org/10.1016/S1470-2045(18)30144-X
Hayashi H, Sugawara S, Fukuda Y et al (2022) A Randomized phase II study comparing nivolumab with carboplatin-pemetrexed for EGFR-mutated NSCLC with Resistance to EGFR tyrosine kinase inhibitors (WJOG8515L). Clin Cancer Res 28(5):893–902. https://doi.org/10.1158/1078-0432.CCR-21-3194
Kawaguchi T, Takada M, Kubo A et al (2010) Performance status and smoking status are independent favorable prognostic factors for survival in non-small cell lung cancer: a comprehensive analysis of 26,957 patients with NSCLC. J Thorac Oncol 5(5):620–630. https://doi.org/10.1097/JTO.0b013e3181d2dcd9
Kehl KL, Riely GJ, Lepisto EM et al (2021) Correlation between surrogate end points and overall survival in a multi-institutional clinicogenomic cohort of patients with non-small cell lung or colorectal cancer. JAMA Netw Open 4(7):e2117547. https://doi.org/10.1001/jamanetworkopen.2021.17547
Kudo K, Nishii K, Makimoto G et al (2022) First and repeat rebiopsy for detecting EGFR T790M mutation in non-small-cell lung cancer: CS-Lung-003 prospective observational registry study. J Cancer Res Clin Oncol 148(8):1869–1877. https://doi.org/10.1007/s00432-021-03893-z
Lee CK, Man J, Lord S et al (2018) Clinical and molecular characteristics associated with survival among patients treated with checkpoint inhibitors for advanced non-small cell lung carcinoma: a systematic review and meta-analysis. JAMA Oncol 4(2):210–6. https://doi.org/10.1001/jamaoncol.2017.4427
Liu S, Wu F, Li X et al (2021) Patients with short PFS to EGFR-TKIs predicted better response to subsequent anti-PD-1/PD-L1 based immunotherapy in EGFR common mutation NSCLC. Front Oncol 11:639947. https://doi.org/10.3389/fonc.2021.639947
Miura S, Nishio M, Akamatsu H et al (2023) Effectiveness and safety of atezolizumab monotherapy in previously treated Japanese patients with unresectable advanced or recurrent NSCLC: a multicenter, prospective, observational study (J-TAIL). JTO Clin Res Rep 4(3):100484. https://doi.org/10.1016/j.jtocrr.2023.100484
Mok TSK, Nakagawa K, Park K et al (2022) Nivolumab (NIVO) + chemotherapy (chemo) vs chemo in patients (pts) with EGFR-mutated metastatic non-small cell lung cancer (mNSCLC) with disease progression after EGFR tyrosine kinase inhibitors (TKIs) in CheckMate 722. Ann Oncol 33(Supplement 9):S1561–S1562. https://doi.org/10.1016/j.annonc.2022.10.350
Nishii K, Inoue M, Obata H et al (2021) Novel prospective umbrella-type lung cancer registry study for clarifying clinical practice patterns: CS-Lung-003 study protocol. Thorac Cancer 12(5):725–731. https://doi.org/10.1111/1759-7714.13789
Nishii K, Ohashi K, Tomida S et al (2022) CD8+ T-cell responses are boosted by dual PD-1/VEGFR2 blockade after EGFR inhibition in Egfr-mutant lung cancer. Cancer Immunol Res 10(9):1111–1126. https://doi.org/10.1158/2326-6066.CIR-21-0751
Nogami N, Barlesi F, Socinski MA et al (2022) Impower150 final exploratory analyses for atezolizumab plus bevacizumab and chemotherapy in key NSCLC patient subgroups with EGFR mutations or metastases in the liver or brain. J Thorac Oncol 17(2):309–323. https://doi.org/10.1016/j.jtho.2021.09.014
Ohashi K, Maruvka YE, Michor F, Pao W (2013) Epidermal growth factor receptor tyrosine kinase inhibitor-resistant disease. J Clin Oncol 31(8):1070–1080. https://doi.org/10.1200/JCO.2012.43.3912
Park S, Kim TM, Han JY et al (2023) A Phase 3, Randomized study of atezolizumab plus bevacizumab and chemotherapy in patients with EGFR or ALK mutated in non-small cell lung cancer (ATTLAS, KCSG-LU19-04). J Clin Oncol. https://doi.org/10.1200/JCO.23.01891
Passaro A, Jänne PA, Mok T, Peters S (2021) Overcoming therapy resistance in EGFR-mutant lung cancer. Nat Cancer 2(4):377–391. https://doi.org/10.1038/s43018-021-00195-8
Qiao M, Jiang T, Liu X et al (2021) Immune checkpoint inhibitors in EGFR-mutated NSCLC: dusk or dawn? J Thorac Oncol 16(8):1267–1288. https://doi.org/10.1016/j.jtho.2021.04.003
Rizvi NA, Hellmann MD, Snyder A et al (2015) Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348(6230):124–8. https://doi.org/10.1126/science.aaa1348
Shigematsu H, Lin L, Takahashi T et al (2005) Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst 97(5):339–346. https://doi.org/10.1093/jnci/dji055
Simmons CP, Koinis F, Fallon MT et al (2015) Prognosis in advanced lung cancer–a prospective study examining key clinicopathological factors. Lung Cancer 88(3):304–309. https://doi.org/10.1016/j.lungcan.2015.03.020
Soria JC, Ohe Y, Vansteenkisite J et al (2018) Osinertinib in untreated EGFR-mutated advanced non-small-cell lung cncer. N Engl J Med 378(2):113–125. https://doi.org/10.1056/NEJMoa1713137
Sugiyama E, Togashi Y, Takeuchi Y et al (2020) Blockade of EGFR improves responsiveness to PD-1 blockade in EGFR-mutated non-small cell lung cancer. Sci Immunol 5(43):eaav3937. https://doi.org/10.1126/sciimmunol.aav3937
Sun H, Liu SY, Zhou JY et al (2020) Specific TP53 subtype as biomarker for immune checkpoint inhibitors in lung adenocarcinoma. EbioMedicine 60:102990. https://doi.org/10.1016/j.ebiom.2020.102990
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
von Pawel J, Bordoni R, Satouchi M et al (2019) Long-term survival in patients with advanced non-small-cell lung cancer treated with atezolizumab versus docetaxel: results from the randomized phase III OAK study. Eur J Cancer 107:124–132. https://doi.org/10.1016/j.ejca.2018.11.020
Watanabe H, Ohashi K, Nishii K et al (2019) A long-term response to nivolumab in a case of PD-L1-negative lung adenocarcinoma with an EGFR mutation and surrounding PD-L1-positive tumor associated macrophages. Intern Med 58(20):3033–3037. https://doi.org/10.2169/internalmedicine.2875-19
Yang JCH, Lee DH, Lee JS et al (2023) Pemetrexed and platinum with or without pembrolizumab for tyrosine kinase inhibitor (TKI)-resistant, EGFR-mutant, metastatic nonsquamous NSCLC: phase 3 KEYNOTE-789 study. J Clin Oncol 41(17 suppl):LBA9000. https://doi.org/10.1200/JCO.2023.41.17_suppl.LBA9000
Yoshida H, Kim YH, Ozasa H et al (2018) Nivolumab in non-small-cell lung cancer with EGFR mutation. Ann Oncol 29(3):777–778. https://doi.org/10.1093/annonc/mdx745
Zhou T, Zhang Z, Luo F et al (2020) Comparison of first-line treatments for patients with extensive-stage small cell lung cancer: a systematic review and network meta-analysis. JAMA Netw Open 3(10):e2015748. https://doi.org/10.1001/jamanetworkopen.2020.15748
Zhou C, Dong X, Chen G, et al. IMpower151: Phase III study of atezolizumab + bevacizumab + chemotherapy in first-line metastatic nonsquamous NSCLC. Presented at: 2023 IASLC World Conference on Lung Cancer; September 9–12, 2023; Singapore, Republic of Singapore. Abstract OA09.06.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
Open Access funding provided by Okayama University. This research received a research grant in 2016 for medicine from Chugoku Occupational Health Association (non-profit organization).
Author information
Authors and Affiliations
Contributions
TaK, KO, KaN and KH contributed to the study design and manuscript writing. TaK, KO and KiN conducted data analysis. All authors provided relevant data for the analysis. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ohashi has received honoraria from Eli Lilly Japan K.K., Novartis Pharma K.K., Chugai Pharmaceutical Co. Ltd., AstraZeneca K.K., Kyowa Kirin Co., Ltd., and Novartis Pharma K.K; grants from Nippon Boehringer Ingelheim Co., Ltd., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Daiichi Sankyo Co. Ltd., Amgen K.K., and Novartis Pharma K.K; and receipt of research reagents from Genentech, Inc. and Novartis Pharma K.K. outside the submitted work. Dr. Ninomiya has received honoraria from AstraZeneca K.K., Nippon Boehringer-Ingelheim Co., Ltd., Kyowa Kirin Co., Ltd., Eli Lilly Japan K.K., Chugai Pharmaceutical Co. Ltd., Nippon Kayaku Co., Ltd., TAIHO PHARMACEUTICAL CO., LTD., MSD K.K., Ono Pharmaceutical CO., LTD., Takeda Pharmaceutical CO., LTD., Pfizer Japan Inc., Bristol Myers Squibb K.K., Elekta K.K., Janssen Pharmaceutical K.K., and Daiichi Sankyo Co. Ltd. outside the submitted work. Dr. Tsubata has received honoraria from Daiichi Sankyo Co. Ltd., AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Kyowa Kirin Co., Ltd, TAIHO PHARMACEUTICAL CO., LTD., and Bristol Myers Squibb K.K.; and subsidies or donations from Pfizer Health Research Foundation outside the submitted work. Dr. Ishikawa has received honoraria from AstraZeneca K.K. and Nippon Boehringer-Ingelheim Co., Ltd. outside the submitted work. Dr. Kodani has received AstraZeneca K.K., Nippon Boehringer Ingelheim Co., Ltd., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Ono Pharmaceutical CO., LTD., Pfizer Japan Inc., TAIHO PHARMACEUTICAL CO., LTD., and Takeda Pharmaceutical CO., LTD. outside the submitted work. Dr. Kuyama has received honoraria from Chugai Pharmaceutical Co. Ltd., Bristol Myers Squibb K.K., Nippon Boehringer Ingelheim Co., Ltd., AstraZeneca K.K., Pfizer Japan Inc., Eli Lilly Japan K.K., MSD K.K., TAIHO PHARMACEUTICAL CO., LTD., Sanofi K.K., Kyowa Kirin Co., Ltd., Hisamitsu Pharmaceutical Co., Inc., Daiichi Sankyo Co., Ltd., Nippon Kayaku Co., Ltd., and Novartis Pharma K.K. outside the submitted work. Dr. Takigawa has received grants and personal fees from Eli Lilly Japan K.K., Chugai Pharmaceutical Co. Ltd., TAIHO PHARMACEUTICAL CO., LTD., Nippon Boehringer-Ingelheim Co., Ltd., and; grants from Kyowa Hakko Kirin Co., Ltd., Nippon Kayaku Co. Ltd., and Takeda Pharmaceutical Co. Ltd.; and personal fees from AstraZeneca K.K., Pfizer Japan Inc., Merck Japan, MSD K.K., Ono Pharmaceutical Co. Ltd. and Bristol Myers Squibb K.K. outside the submitted work. Dr. Fujimoto received honoraria from Ono Pharmaceutical Co. Ltd., AstraZeneca K.K., Nippon Boehringer-Ingelheim Co., Ltd., and Nippon Kayaku Co., Ltd. outside the submitted work. Dr. Fujiwara has received honoraria from MSD K.K., AstraZeneca K.K., Ono Pharmaceutical Co. Ltd., Sanofi K.K., and Eli Lilly Japan K.K. outside the submitted work. Dr. Kiura has received honoraria from AstraZeneca K.K., Nippon Boehringer-Ingelheim Co., Ltd., Merk Biopharma, TAIHO PHARMACEUTICAL CO., LTD., Chugai Pharmaceutical Co. Ltd., Takeda Pharmaceutical CO., LTD., Eli Lilly Japan K.K., Pfizer Japan Inc. Bristol Myers Squibb K.K., NipponKayaku Co., Ltd., Ono Pharmaceutical Co. Ltd., and MSD K.K.; research fund from Nippon Boehringer-Ingelheim Co., Ltd., Ono Pharmaceutical Co. Ltd., Novartis Pharma K.K., Takeda Pharmaceutical CO., LTD., Teijin pharma Ltd., Kyorin Pharmaceutical Co., Ltd., Shionogi Pharma Co., Ltd., Nippon Kayaku Co., Ltd., TAIHO PHARMACEUTICAL CO., LTD., and Chugai Pharmaceutical; and consulting fees from Nippon Kayaku Co., Ltd., and Nipro Corp. outside the submitted work. Dr. Hotta has received honoraria from Pfizer Japan Inc., AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Takeda Pharmaceutical CO., LTD., MSD K.K., Bristol Myers Squibb K.K., Ono Pharmaceutical Co. Ltd., Nippon Boehringer-Ingelheim Co., Ltd., and NipponKayaku Co., Ltd.; and research fund from MSD K.K., AstraZeneca K.K., Chugai Pharmaceutical Co. Ltd., Eli Lilly Japan K.K., Bristol Myers Squibb K.K., and Abbvie Inc. outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kuribayashi, T., Ohashi, K., Nishii, K. et al. Clinical characteristics of patients treated with immune checkpoint inhibitors in EGFR-mutant non-small cell lung cancer: CS-Lung-003 prospective observational registry study. J Cancer Res Clin Oncol 150, 89 (2024). https://doi.org/10.1007/s00432-024-05618-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05618-4