Abstract
Purpose
The transcription factors YY1 and CP2 have been associated with tumor promotion and suppression in various cancers. Recently, simultaneous expression of both markers was correlated with negative prognosis in cancer. The aim of this study was to explore the expression of YY1 and CP2 in head and neck squamous cell carcinoma (HNSCC) patients and their association with survival.
Methods
First, we analyzed mRNA expression and copy number variations (CNVs) of YY1 and CP2 using “The Cancer Genome Atlas” (TCGA) with 510 HNSCC patients. Secondly, protein expression was investigated via immunohistochemistry in 102 patients, who were treated in the Vienna General Hospital, utilizing a tissue microarray.
Results
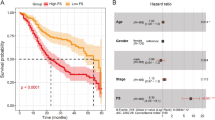
The median follow-up was 2.9 years (1.8–4.6) for the TCGA cohort and 10.3 years (6.5–12.8) for the inhouse tissue micro-array (TMA) cohort. The median overall survival of the TCGA cohort was decreased for patients with a high YY1 mRNA expression (4.0 vs. 5.7 years, p = 0.030, corr. p = 0.180) and high YY1-CNV (3.53 vs. 5.4 years, p = 0.0355, corr. p = 0.213). Furthermore, patients with a combined high expression of YY1 and CP2 mRNA showed a worse survival (3.5 vs. 5.4 years, p = 0.003, corr. p = 0.018). The mortality rate of patients with co-expression of YY1 and CP2 mRNA was twice as high compared to patients with low expression of one or both (HR 1.99, 95% CI 1.11–3.58, p = 0.021). Protein expression of nuclear YY1 and CP2 showed no association with disease outcome in our inhouse cohort.
Conclusion
Our data indicate that simultaneous expression of YY1 and CP2 mRNA is associated with shorter overall survival. Thus, combined high mRNA expression might be a suitable prognostic marker for risk stratification in HNSCC patients. However, since we could not validate this finding at genomic or protein level, we hypothesize that unknown underlying mechanisms which regulate mRNA transcription of YY1 and CP2 are the actual culprits leading to a worse survival.
Similar content being viewed by others
Introduction
Head and neck squamous cell carcinoma (HNSCC) is the sixth most frequent cancer worldwide and about 650,000 new cases are diagnosed each year (Cognetti et al. 2008). The reported 5-year survival rates range between 25 and 59% and strongly depend on the anatomic site and stage at presentation (Gatta et al. 2015). Treatment options include surgical resection, radio- and chemotherapy. Although therapy has evolved and survival rates have improved, about one-third of patients die within 5-years of diagnosis (Pulte and Brenner 2010). To date, known risk factors for poor survival are smoking, poor socioeconomic status and a negative human papilloma virus (HPV) status in oropharyngeal SCC patients (Gatta et al. 2015). While treatment de-escalation is currently under clinical investigation in HPV-positive oropharyngeal SCC patients, biomarkers for better therapeutic decision guidance in HNSCC are still lacking (Mirghani and Blanchard 2018).
The transcription factors Ying Yang 1 (YY1) and CP2 have been shown to act as tumor suppressors and promoters. YY1 is an ubiquitous transcription activator and repressor and is involved in the transcriptional regulation of approximately 10% of the human exome (Gordon et al. 2006; Khachigian 2018). Among many different functions, it is involved in the regulation of cell proliferation, apoptosis, DNA repair, chromatin modelling and epigenetic modification (Sarvagalla et al. 2019). While YY1 acts as a tumor suppressor in pancreatic cancer (Zhang et al. 2016), it exhibits a tumor promoting function in colon cancer (Yokoyama et al. 2010) and prostate cancer (Camacho-Moctezuma et al. 2018).
The transcription factor CP2, also known as Late SV40 Factor (LSF) and LBP-1c, is ubiquitously expressed as well. It is involved in hematopoiesis, regulation of the cell cycle and expression of immune-related genes. CP2 is overexpressed in many cancers, such as hepatocellular carcinoma (Yoo et al. 2010), pancreatic cancer (Yuedi et al. 2017) and colorectal cancer (Jiang et al. 2014), and mostly serves as a pro-oncogene (Kotarba et al. 2018). However, in melanoma cells, overexpression of CP2 leads to growth inhibition (Goto et al. 2016).
One possible explanation for the controversial effects in tumors of both transcription factors is the interaction with other proteins. In hepatocellular carcinoma, the co-expression of the transcription factors YY1 and CP2 was associated with a significantly worse prognosis (Kim et al. 2017). This was the first report that proposed the joint expression of both genes as prognostic markers in a tumor. In fact, data on the interaction of YY1 and CP2 are sparse. Structural and interaction analysis showed that YY1 is able to bind to CP2 (Coull et al. 2000; Kang et al. 2005) and together they are involved in spermatogenesis (Kim et al. 2016) and HIV replication (Romerio et al. 1997; Coull et al. 2000).
Hence, in this study, we investigated the mRNA expression and copy number variation (CNV) of YY1 and CP2 and their individual and combined prognostic relevance in HNSCC. Furthermore, we analyzed their expression at the protein level in an independent patient cohort.
Patients and methods
The Cancer Genome Atlas dataset
Data from “The Cancer Genome Atlas” (TCGA), namely “TCGA, Firehose Legacy” including 530 samples were extracted from cBioportal.org. Missing data were extracted from “TCGA PanCancer Atlas” including 523 samples (Liu et al. 2018), and “TCGA, Nature 2015” including 279 samples (Lawrence et al. 2015). Patients with incomplete survival data or missing mRNA data were excluded as well as patients with an overall survival (OS) of less than 2 months due to the possibility of perioperative complications (n = 11). HPV status was assessed via RNA sequencing as described by Liu et al. (2018, Suppl. Information). Most patients received surgical resection with curative intent and postoperative radiotherapy (Liu et al. 2018, Suppl. Information). However, treatment options also included neoadjuvant radiotherapy or pharmaceutical therapy. Only few patients received primary radiotherapy and/or chemotherapy (see Table 1). mRNA expression z scores (RNA Seq V2 RSEM) were extracted for YY1 and TFCP2 via cBioportal.org. Thus, after merging these datasets we were able to include 510 patients in total. mRNA expression was divided into low and high expression with a cutoff at a z score of > 0 for high mRNA expression. CNV data were retrieved from UCSC Xena for YY1 and TFCP2 (Goldman et al. 2020). CNV calculation was performed as described by the copy number variation analysis pipeline of the National Cancer Institute GDC Documentation (Copy Number Variation Analysis Pipeline). The cohort was divided by the median copy number.
Tissue microarray patient dataset
In this cohort, we included 102 HNSCC patients from a single center, retrospective study at the Vienna General Hospital. Patients received surgery, postoperative radiotherapy and additional chemotherapy in case of extranodal spread between 2002 and 2012. Patients were excluded when they had a second primary carcinoma, received external treatment, showed distant metastasis, had prior irradiation or were under immunosuppression. Data were collected by medical chart review. HPV status was assessed using in situ hybridization. Collected data included date of birth, time of initial diagnosis, recurrence, tumor grading, histology and date of death or date of last follow-up. This study was approved by the ethics committee of the Medical University of Vienna (EK1262/2019).
Tissue microarray
Tissue samples were taken from preselected formalin-fixed, paraffin-embedded (FFPE) HNSCC tissue acquired through surgical resection. The tissue microarray (TMA) was constructed using a Galileo TMA CK Series-HTS Tissue computer assisted TMA Microarray Platform (Integrated Systems Engineering Srl, Milan, Italy). Histology was confirmed by hematoxylin–eosin (H&E) staining. Subsequently, 4 µm sections were prepared for immunohistochemical analysis.
Immunohistochemistry
Immunohistochemical staining was performed using a Lab Vision Ultra Kit (Thermo Scientific) according to the manufacturer’s protocol. In short, the appropriate retrieval buffer and antibody dilution were assessed prior to analysis using colon and stomach tissue as positive control. After dewaxing and dehydrating the TMA, antigen retrieval was performed using EDTA in a microwave oven at 600 W for 10 min. Endogenous peroxidase activity was blocked in 3% H2O2 and Ultra V Block was applied. Subsequently, the tissue was incubated for 1 h with the primary antibodies against YY1 1:100 (sc-7341, Santa Cruz Biotechnology) and CP2 1:200 (610818, BD Biosciences) at room temperature. Then, the primary antibody enhancer and horseradish peroxidase enhancer were applied for 10 and 15 min, respectively. UltraVision Plus Detection System DAB Plus Substrate System (Thermo Scientific) was used to visualize staining. Tissues were counterstained with hematoxylin Gill II (Merck). The tissues were scanned using an NIKON Eclipse Ti microscope (NIKON) and analyzed using a modified ImageJ plugin of “IHC Profiler” (Varghese et al. 2014). Since the original plugin uses threshold adjustment and selection in the deconvoluted DAB image to select nuclei or tissue, all nuclei or tissue with negative staining were not considered. Therefore, the script was changed to adjust the threshold in the binarized original image before deconvolution to include either all nuclei or the whole tissue area. The threshold was then used for selection to analyze nuclear YY1 or overall CP2 DAB intensity in the deconvoluted image. Expression levels were categorized by the IHC Profiler under visual control of the researcher (J.S.) in negative, low positive, positive, and high positive expression levels. Negative and low positive expression levels were further grouped into low expression, and positive and high positive expression were considered as high expression.
Statistical analysis
To further analyze the combined expression of YY1 and CP2, the YY1CP2 score was formed. The YY1CP2 score was considered positive when mRNA, CNV or protein levels of both YY1 and CP2 were high (high YY1/high CP2). When both levels were low, or only one was high, the YY1CP2 score was considered negative (low YY1/low CP2, low YY1/high CP2, high YY1/low CP2). Categorical data were reported as absolute frequencies (%) and continuous data as median as well as 25th and 75th percentiles. OS or disease-free survival (DFS) were calculated from the date of diagnosis to the date of death or tumor recurrence, respectively. Kaplan–Meier curves were calculated to visualize OS and DFS rates and analyzed for statistical significance using log-rank test. Uni- and multivariable regression analysis was calculated using the Cox proportional hazard model. The multivariable model was corrected for staging, HPV, and smoker status. A pairwise-interaction analysis between YY1 and CP2 mRNA expression was performed to further analyze the impact of combined high expression on OS. The median follow-up was calculated using the method published by Schemper and Smith (1996). Statistical analysis was performed using Prism GraphPad software (GraphPad Software, Inc, La Jolla, CA) and Stata (Stata Corp, Houston, TX).
Results
Analysis at baseline
Five hundred and ten (510) patients were included in the TCGA dataset. Patient characteristics are shown in Table 1. The median observation period was 2.9 years (1.8–4.6). The median age at diagnosis was 60.5 years (53–68). The 5-year OS was 41% and the 5-year DFS was 45%. Treatment options included surgery, radiotherapy and pharmaceutical therapy as specified in Table 1; however, it is unspecified in up to 50%.
Analysis of expression of YY1 and CP2 mRNA and clinicopathological data
mRNA levels were split into high or low levels with a cutoff at a z score of 0. YY1 mRNA levels were high in 54% (275) and CP2 mRNA levels were high in 50% (253) of the samples. Since mRNA levels of YY1 and CP2 showed a low positive correlation (Fisher’s exact p = 0.027, correlation coeff. r = 0.221) we formed the YY1CP2 score. Twenty-nine percent (149) showed a positive YY1CP2 score (high expression of YY1 and CP2).
The expression of YY1, CP2 and the YY1CP2 score was analyzed for its association with various clinicopathological features (Suppl. Table 1). Low mRNA expression of CP2 was more commonly found in patients with a higher T stage (T3–T4; p = 0.005, corr. p = 0.030) and HPV-negative patients (p = 0.002, corr. p = 0.012). Furthermore, male patients more commonly showed high YY1 mRNA expression (p = 0.008, corr. p = 0.048). After Bonferroni correction, there was no further significant correlation. The YY1CP2 score showed no association with clinicopathological data.
Analysis of expression of YY1 and CP2 copy number variation and clinicopathological data
CNVs were divided into high or low using the median as cutoff. YY1-CNVs were high in 50% (254) and CP2-CNVs were high in 28% (143) of the samples. The YY1CP2- score was high in 28% (143). While the categorical evaluation of YY1- and CP2-CNVs showed a correlation, the continuous CNVs showed only a very weak correlation (Fisher’s exact p = 0.002, correlation coeff. r = − 0.076).
The correlation of CNV to clinicopathological data revealed an association of YY1-CNV with HPV (p < 0.001, corr. p < 0.006) and smoker status (p = 0.006, corr. p = 0.036). There was no further significant correlation of YY1-, CP2-CNV or the CNV-YY1CP2 score after Bonferroni correction.
We then analyzed whether there was a correlation of mRNA and CNV values. YY1 mRNA showed a strong correlation with CNV values (Fisher’s exact p < 0.001; correlation coeff. r = 0.618). CP2 mRNA expression revealed a moderate correlation with CNV (Fisher’s exact p < 0.001; correlation coeff. r = 0.441).
Analysis of overall survival and disease-free survival
To determine whether levels of YY1 or CP2 mRNA expression or CNV might be associated with disease outcome in HNSCC patients, we examined OS and DFS in the TCGA. As shown in Fig. 1, survival was decreased for patients with high expression of YY1 (4.0 vs. 5.7 years, p = 0.030, corr. p = 0.180). Furthermore, the median OS was decreased in case of a positive YY1CP2 score (3.5 vs. 5.4 years, p = 0.003, corr. p = 0.018). When CNV data were analyzed, only patients with a high YY1-CNV showed a worse survival (3.5 vs. 5.4 years, p = 0.0355, corr. p = 0.213). There was no further association of mRNA levels, CNV or (CNV-)YY1CP2 score with OS or DFS. Kaplan–Meier curves for DFS were calculated as shown in Suppl. Figure 1.
Univariable analysis showed a worse OS for patients with high YY1 mRNA levels (HR 1.35, 95% CI 1.03–1.78, p = 0.030, corr. p = 0.180). This result did not prevail in multivariable analysis after correction for stage, smoker status and HPV status (Table 2). Further analysis of the risk per increase of z score unit did not reach statistical significance. Univariable analysis of CP2 expression or z score did not show a significant association with outcome. However, after correction for multiple confounders, patients showed an increased risk for death of 14% per increase in z score (HR 1.14, 95% CI 1.00–1.29, p = 0.049, corr. p = 0.294). Patients with a positive YY1CP2 score showed a significantly increased risk for death in uni- (HR 1.55, 95% CI 1.16–2.05, p = 0.003, corr. p = 0.018) and multivariable analysis (HR 1.60, 95% CI 1.19–2.16, p = 0.002, corr. p = 0.012). To determine whether those two mRNA markers significantly interact, we added pairwise-interaction terms to the cox regression model. This revealed no individual increase in risk for high mRNA expression of only one (YY1 or CP2). However, when both mRNA expression levels were high, uni- and multivariable pairwise-interaction analysis revealed a significant association with a worse OS (univariable: HR 1.96, 95% CI 1.12–3.43, p = 0.018; multivariable: HR 1.99, 95% CI 1.11–3.58, p = 0.021).
Analysis of CNV data revealed a higher risk for death in case of high YY1-CNV in univariable analysis (HR 1.33, 95% CI 1.02–1.75, p = 0.036, corr. p = 0.216). However, this result did not prevail in multivariable analysis, and uni- and multivariable analysis of continuous CNV values. Furthermore, analysis of CP2-CNV or the calculated CNV-YY1CP2 score did not show an association with outcome.
To better compare the two datasets, we analyzed only TCGA patients who received postoperative radio(chemo)therapy. YY1 and CP2 mRNA were not associated with OS. However, patients with a combined high expression of YY1 and CP2 showed a significantly shorter OS (3.9 vs. 5.7 years, log-rank p = 0.038, corr. p = 0.114). Further analysis of the YY1CP2 score revealed an increased risk for death (HR 1.69, 95% CI 1.02–2.79, p = 0.040, corr. p = 0.120) independent of multiple confounders (HR 1.73, 95% CI 1.04–2.87, p = 0.034, corr. p = 0.102). Interaction analysis further confirmed the association with OS (univariable: HR 3.67, 95% CI 1.27–10.60, p = 0.016; multivariable: HR 3.49, 95% CI 1.19–10.19, p = 0.023).
Tissue microarray dataset
To further explore the association of YY1 and CP2 with disease outcome, we examined expression at the protein level using immunohistochemistry (Fig. 2). In total, 102 patients with HNSCC were included in our secondary dataset. Patient characteristics are presented in Table 1. The median observation period was 10.3 years (6.5–12.8). The median age at diagnosis was 59 (53–63). The 5-year OS was 56% and the 5-year DFS was 67%. All patients received postoperative radiotherapy with a median dose of 60 Gy. Sixteen percent (16) received additional chemotherapy due to extracapsular spread or R1 resection.
Immunohistochemical staining showed high expression of nuclear YY1 in 19% (19) and high expression of CP2 in 44% (45). High expression of YY1 showed a moderate positive correlation with high expression of CP2 (Fisher’s exact p < 0.001, correlation coeff. r = 0.491). After combining the expressions of YY1 and CP2 to form the YY1CP2 score (as described earlier), 17% (17) showed a positive score.
Next, we tested for associations of marker expression with clinicopathological characteristics. Low YY1 protein expression (p = 0.014, corr. p = 0.042) and a negative YY1CP2 score (p = 0.011, corr. p = 0.033) were associated with a negative HPV status (Suppl. Table 2). There was no further association of protein expression or YY1CP2 score with other clinicopathological features.
Finally, we analyzed marker expression at the protein level and its association with disease outcome. No significant association of protein expression or the YY1CP2 score with OS or DFS was observed (Table 2, Suppl. Table 3). Kaplan–Meier curves for OS and DFS were calculated as shown in Fig. 1 and Suppl. Figure 1, respectively.
Statistical comparison of the two cohorts
As seen in Table 1, the two cohorts show differences in the locations of the primary. The TCGA dataset generally contains more locally advanced stages (p < 0.001) with a lower N stage (p < 0.001). Resulting in more early-staged cancers (I–II, p < 0.001). Interestingly, the TCGA cohort shows a generally worse OS (4.7 vs 7.1 years, p = 0.003) and DFS (4.7 vs. 13 years, p < 0.001). Observation time differs between the cohorts (2.9 vs. 10.3 years, p < 0.001). The TCGA cohort contains fewer active smokers (p < 0.001) and more patients with an HPV negative status (p = 0.019), probably due to less patients with oropharyngeal carcinoma. Patients within the TCGA cohort are older (61 vs. 58 years, t test p = 0.028, chi2 p = 0.344). Furthermore, the application of radiotherapy (p < 0.001) and chemotherapy (p < 0.001) differs greatly; however, for up to 50% of the patient’s therapy is not further specified in the TCGA cohort. For better comparison to the TMA cohort, we analyzed the TCGA subgroup who received postoperative radio(chemo)therapy. However, this subgroup still shows significant differences in the location of the primary, T stage, N stage, smoker status and the application of pharmaceutical therapy (data not shown, all p < 0.001).
Discussion
HNSCC is among the ten most frequently diagnosed malignancies worldwide. Survival has improved over the last 2 decades, still about one-third of HNSCC patients die within 5 years of diagnosis (Pulte and Brenner 2010). If these high-risk patients could be identified early in the course of their disease, intensified treatment could potentially be beneficial. Hence, it is necessary to find prognostic markers to stratify high-risk patients.
The transcription factors YY1 and CP2 act as tumor suppressors and promoters. A combined high protein expression of these factors was recently linked to a worse prognosis in hepatocellular carcinoma (Kim et al. 2017). To date, there is only little data on the role of these transcription factors in HNSCC. Noteworthy, YY1 protein expression is associated with enhanced proliferation and migration in oral cancer cells (Behera et al. 2019). Furthermore, high expression of YY1 mRNA and protein was associated with pro-neoplastic effects in laryngeal cancer (Qu et al. 2017). For CP2 protein expression, a report in oral carcinoma showed an upregulation and association with higher tumor and TNM stage (Chen et al. 2017). The purpose of this study was to investigate the individual role of YY1 and CP2 in HNSCC as well as a statistical add on effect of their co-expression.
First, we evaluated the mRNA expression levels of YY1 and CP2 in a cohort of HNSCC patients, which we extracted from “The Cancer Genome Atlas, Firehose Legacy”. Although Kaplan–Meier curves revealed a trend for worse survival of patients with a high YY1 or CP2 mRNA expression, further statistical analysis was controversial. High YY1 mRNA expression was associated with a shorter median survival in univariable analysis but did not prevail after correcting for multiple confounders. High expression of CP2 mRNA was not associated with survival. Further analysis of the association of survival with continuous z scores revealed no significant influence of the YY1 z score. Interestingly, a higher CP2 z score showed an increased risk for death after multivariable correction. In literature, YY1 mRNA expression was not associated with survival in cancers of the central nervous system, the breast, the colon, and the lungs (Bonavida and Kaufhold 2015). In contrast, high expression of YY1 mRNA was associated with a worse outcome in diffuse large B-cell lymphoma (DLBCL) (Sakhinia et al. 2007) but showed a better outcome in pancreatic cancer (Zhang et al. 2014). In hepatocellular carcinoma, high expression of CP2 mRNA was associated with a worse DFS but not with OS (Kim et al. 2017).
We subsequently formed a YY1CP2 score to compare patients with simultaneous high levels of YY1 and CP2 mRNA (positive YY1CP2 score) to the group with a negative YY1CP2 score. Patients with a positive YY1CP2 score showed a shorter median survival and this turned out to be an independent prognostic marker for worse OS in multivariable analysis. We then performed an interaction analysis and found that the combined high YY1 and CP2 status proved to be an independent prognostic marker for worse OS. In contrast, no association with prognosis was found for individual high expression of either YY1 or CP2 in this interaction model. Interestingly, analysis of DFS showed no association with YY1, CP2 or the YY1CP2 score. Moreover, there was no association of the YY1CP2 score with clinicopathological features, suggesting its independence from potential confounders. In accordance with our findings, in hepatocellular carcinoma, survival was decreased in case of combined high protein expression of CP2 and YY1 (Kim et al. 2017).
Next, we analyzed CNVs of YY1 and CP2. In accordance with our findings at mRNA level, patients with a high YY1-CNV showed a shorter OS. However, this result did not prevail after correction for multiple confounders. Likewise, there was no other association of YY1- or CP2-CNV with DFS or OS. Although mRNA and CNV values showed a moderate-to-strong positive correlation, the analysis of the formed CNV-YY1CP2 score showed no association with OS or DFS. In contrast to our findings, CP2-CNV was associated with DFS in hepatocellular carcinoma (Kim et al. 2017).
To verify our findings at the protein level, we investigated the expression of CP2 and nuclear YY1 in a secondary dataset using immunohistochemistry. In concordance with our findings on mRNA level, expression of CP2 and nuclear YY1 showed a positive correlation. However, we could not find a significant association with OS or DFS. Likewise, Kim et al. found no significant association of CP2 or YY1 expression with OS in hepatocellular carcinoma; however, CP2 expression was associated with a worse DFS (Kim et al. 2017). In contrast, Jiang et al. found that high CP2 protein expression was associated with a worse prognosis in hepatocellular carcinoma (Jiang et al. 2014). For YY1, high expression was associated with a worse outcome in hepatoblastoma (Shin et al. 2011), DLBCL and follicular lymphoma (Sakhinia et al. 2007). Interestingly, high expression of YY1 was also associated with a longer DFS in prostate cancer (Seligson et al. 2005) and a better outcome in pancreatic cancer (Zhang et al. 2014), colon cancer (Chinnappan et al. 2009) and follicular lymphoma (Naidoo et al. 2011).
Altogether, the question remains whether the transcription factors YY1 and CP2 influence survival via joint activation or suppression of other genes (our data suggest otherwise), or unknown underlying mechanisms which regulate mRNA transcription of YY1 and CP2 are the actual culprits leading to a worse outcome. In the literature, YY1 and CP2 mRNA expression generally correlated with protein expression (Jiang et al. 2014; Zhang et al. 2014). A possible explanation for our divergent results of mRNA and protein expression is the influence of posttranscriptional processes to protein abundance (Liu et al. 2016). Furthermore, there might be some selection bias since our secondary dataset only included tissue from patients who received surgical therapy and postoperative radio(chemo)therapy. Thus, we performed a short analysis of the TCGA subgroup who received postoperative radio(chemo)therapy. The association of combined high mRNA expression of YY1 and CP2 with OS did not change significantly; however, the subgroup still showed differences in patient characteristics. All in all, there was no relevant correlation of mRNA or protein expression with clinicopathological data, which would explain the different results of the two cohorts. This study design, however, is not suitable to evaluate the relationship between mRNA and protein levels of YY1 and CP2 since they were investigated in different patient cohorts.
Limitations of this study are the comparison of mRNA expression with protein expression in different cohorts. Although protein levels largely depend on mRNA levels, this is a complicated relationship and can easily vary through post-transcriptional processes, protein half-lives and the error or noise of the experiments (Liu et al. 2016). Both datasets are limited due to their retrospective designs. Furthermore, the secondary dataset shows a considerably smaller number of patients. Protein expression was investigated in FFPE tissue; thus, some protein might be lost compared with fresh tissue. Furthermore, staining intensity was evaluated using a modification of the ImageJ plugin of “IHC Profiler” (Varghese et al. 2014) under visual control of one fully blinded researcher (J.S.). All in all, external validation of our findings at the mRNA, CNV and protein level are necessary.
In conclusion, we showed for the first time that high co-expression of YY1 and CP2 mRNA is an independent prognostic marker for a worse OS in HNSCC. However, we were not able to validate these findings at the protein level in an independent cohort. Nonetheless, we hypothesize that our data show a prognostic relevance of combined high expression of YY1 and CP2 mRNA in HNSCC and this warrants further investigation.
Availability of data, materials and code
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CNV:
-
Copy number variation
- DFS:
-
Disease-free survival
- DLBCL:
-
Diffuse large B cell lymphoma
- FFPE:
-
Formalin-fixed, paraffin-embedded
- HNSCC:
-
Head and neck squamous cell carcinoma
- LSF:
-
Late SV40 Factor
- OS:
-
Overall survival
- SCC:
-
Squamous cell carcinoma
- TCGA:
-
The Cancer Genome Atlas
- TMA:
-
Tissue microarray
- YY1:
-
Ying Yang 1
References
Behera AK, Kumar M, Shanmugam MK et al (2019) Functional interplay between YY1 and CARM1 promotes oral carcinogenesis. Oncotarget 10:3709–3724
Bonavida B, Kaufhold S (2015) Prognostic significance of YY1 protein expression and mRNA levels by bioinformatics analysis in human cancers: a therapeutic target. Pharmacol Ther 150:149–168
Camacho-Moctezuma B, Quevedo-Castillo M, Melendez-Zajgla J, Aquino-Jarquin G, Martinez-Ruiz GU (2019) YY1 negatively regulates the XAF1 gene expression in prostate cancer. Biochem Biophys Res Commun 508:973–979
Chen CH, Tsai HT, Chuang HC et al (2017) Metformin disrupts malignant behavior of oral squamous cell carcinoma via a novel signaling involving Late SV40 factor/Aurora-A. Sci Rep 7:1–15
Chinnappan D, Xiao D, Ratnasari A, Andry C, King TC, Weber HC (2009) Transcription factor YY1 expression in human gastrointestinal cancer cells. Int J Oncol 35:547–557
Cognetti DM, Weber RS, Lai SY (2008) Head and neck cancer an evolving treatment paradigm. Cancer 113:1911–1932
Copy number variation analysis pipeline. https://docs.gdc.cancer.gov/Data/Bioinformatics_Pipelines/CNV_Pipeline/
Coull JJ, Romerio F, Sun J-M et al (2000) The human factors YY1 and LSF repress the human immunodeficiency virus type 1 long terminal repeat via recruitment of histone deacetylase 1. J Virol 74:6790–6799
Gatta G, Botta L, Sánchez MJ et al (2015) Prognoses and improvement for head and neck cancers diagnosed in Europe in early 2000s: The EUROCARE-5 population-based study. Eur J Cancer 51:2130–2143
Goldman MJ, Craft B, Hastie M et al (2020) Visualizing and interpreting cancer genomics data via the Xena platform. Nat Biotechnol 38:675–678
Gordon S, Akopyan G, Garban H, Bonavida B (2006) Transcription factor YY1: structure, function, and therapeutic implications in cancer biology. Oncogene 25:1125–1142
Goto Y, Yajima I, Kumasaka M et al (2016) Transcription factor LSF (TFCP2) inhibits melanoma growth. Oncotarget 7:2379–2390
Jiang H, Du J, Jin J, Qi X, Pu Y, Fei B (2014) LSF expression and its prognostic implication in colorectal cancer. Int J Clin Exp Pathol 7:6024–6031
Kang HC, Chung BM, Chae JH, Il YS, Kim CG, Kim CG (2005) Identification and characterization of four novel peptide motifs that recognize distinct regions of the transcription factor CP2. FEBS J 272:1265–1277
Khachigian LM (2018) The Yin and Yang of YY1 in tumor growth and suppression. Int J Cancer 143:460–465
Kim JS, Chae JH, Cheon Y-P, Kim CG (2016) Reciprocal localization of transcription factors YY1 and CP2c in spermatogonial stem cells and their putative roles during spermatogenesis. Acta Histochem 118:685–692
Kim JS, Son SH, Kim MY et al (2017) Diagnostic and prognostic relevance of CP2c and YY1 expression in hepatocellular carcinoma. Oncotarget 8:24389–24400
Kotarba G, Krzywinska E, Grabowska AI, Taracha A, Wilanowski T (2018) TFCP2/TFCP2L1/UBP1 transcription factors in cancer. Cancer Lett 420:72–79
Lawrence MS, Sougnez C, Lichtenstein L et al (2015) Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature 517:576–582
Liu Y, Beyer A, Aebersold R (2016) On the dependency of cellular protein levels on mRNA abundance. Cell 165:535–550
Liu J, Lichtenberg T, Hoadley KA et al (2018) An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell 173:400–416
Mirghani H, Blanchard P (2018) Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol 8:4–11
Naidoo K, Clay V, Hoyland JA et al (2011) YY1 expression predicts favourable outcome in follicular lymphoma. J Clin Pathol 64:125–129
Pulte D, Brenner H (2010) Changes in survival in head and neck cancers in the late 20th and early 21st century: a period analysis. Oncologist 15:994–1001
Qu S, Sun Y, Li Y, Xu Z, Fu W (2017) YY1 directly suppresses MYCT1 leading to laryngeal tumorigenesis and progress. Cancer Med 6:1389–1398
Romerio F, Gabriel MN, Margolis DM (1997) Repression of human immunodeficiency virus type 1 through the novel cooperation of human factors YY1 and LSF. J Virol 71:9375–9382
Sakhinia E, Glennie C, Hoyland JA et al (2007) Clinical quantitation of diagnostic and predictive gene expression levels in follicular and diffuse large B-cell lymphoma by RT-PCR gene expression profiling. Blood 109:3922–3928
Sarvagalla S, Kolapalli SP, Vallabhapurapu S (2019) The two sides of YY1 in cancer: a friend and a foe. Front Oncol 9:10–13
Schemper M, Smith TL (1996) A note on quantifying follow-up in studies of failure time. Control Clin Trials 17:343–346
Seligson D, Horvath S, Huerta-Yepez S et al (2005) Expression of transcription factor Yin Yang 1 in prostate cancer. Int J Oncol 27:131–141
Shin E, Lee K-B, Park S-Y et al (2011) Gene expression profiling of human hepatoblastoma using archived formalin-fixed and paraffin-embedded tissues. Virchows Arch 458:453–465
Varghese F, Bukhari AB, Malhotra R, De A (2014) IHC Profiler: an open source plugin for the quantitative evaluation and automated scoring of immunohistochemistry images of human tissue samples (SA Aziz, Ed.). PLoS ONE 9:e96801
Yokoyama NN, Pate KT, Sprowl S, Waterman ML (2010) A role for YY1 in repression of dominant negative LEF-1 expression in colon cancer. Nucleic Acids Res 38:6375–6388
Yoo BK, Emdad L, Gredler R et al (2010) Transcription factor Late SV40 Factor (LSF) functions as an oncogene in hepatocellular carcinoma. Proc Natl Acad Sci USA 107:8357–8362
Yuedi D, Yuankun C, Jiaying Z et al (2017) TFCP2 activates beta-catenin/TCF signaling in the progression of pancreatic cancer. Oncotarget 8:70538–70549
Zhang JJ, Zhu Y, Xie KL et al (2014) Yin Yang-1 suppresses invasion and metastasis of pancreatic ductal adenocarcinoma by downregulating MMP10 in a MUC4/ErbB2/p38/MEF2C-dependent mechanism. Mol Cancer 13:130
Zhang JJ, Zhu Y, Yang C et al (2016) Yin Yang-1 increases apoptosis through bax activation in pancreatic cancer cells. Oncotarget 7:28498–28509
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Contributions
JS, BJJ and SS: contributed to the study design, data collection, statistical analysis, and manuscript writing; LKW, SS, CPS, LK and GH: contributed to the study design, data collection and manuscript revision. All authors critically reviewed and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the ethics committee of the Medical University of Vienna (EK1262/2019).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schnoell, J., Jank, B.J., Kadletz-Wanke, L. et al. Transcription factors CP2 and YY1 as prognostic markers in head and neck squamous cell carcinoma: analysis of The Cancer Genome Atlas and a second independent cohort. J Cancer Res Clin Oncol 147, 755–765 (2021). https://doi.org/10.1007/s00432-020-03482-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03482-6