Abstract
Purpose
A randomized controlled trial was conducted to determine whether pathologic necrosis in response to preoperative treatment with uracil–tegafur(UFT) could be used to identify patients with colorectal cancer most likely to benefit from postoperative adjuvant therapy with the drug.
Patients and methods
The 152 patients with colorectal cancer who received preoperative UFT at a dose of 600 mg/day for at least 10 days were classified into two groups according to the pathologic necrosis in resected tumor specimens: 90% or more necrosis (sensitive) versus less than 90% necrosis (insensitive). After excluding 13 ineligible patients, the remaining 139 were then randomly assigned to receive postoperative adjuvant UFT (400 mg/day) for 12 months or no treatment.
Results
Preoperative and postoperative UFT produced no serious toxicity in any of the patients. Among the 22 patients with sensitive tumors, overall survival was significantly better in the UFT group (n = 12) than in the control (n = 10) (100 vs. 70.0%; P = 0.023). Among the 117 patients with insensitive tumors, there was no significant difference between the two groups (n = 60, 68.1% vs. n = 57, 76.6%; P = 0.373).
Conclusion
Our method involving neoadjuvant UFT can identify patients most likely to benefit from postoperative UFT, as well as those unlikely to benefit from such treatment.
Similar content being viewed by others
Introduction
Despite the recent development of drugs such as irinotecan, oxaliplatin, bevacitumab and cetuximab, 5-fluorouracil (5-FU) continues to have an important role in the management of advanced colorectal cancer (Douillard et al. 2000; Bleiberg 1998; Punt 1998). Uracil–tegafur (UFT) is a preparation combining uracil and tegafur in a fixed molar ratio of 4:1 (Fujii et al. 1979). Uracil competitively blocks the metabolism of 5-FU, leading to increased 5-FU concentrations in plasma and tumor (Ikenaka et al. 1979). UFT can be administered orally on an outpatient basis. However, the clinical response of individual tumors to UFT is often unpredictable. Previous studies have shown that “pathologic necrosis” induced by neoadjuvant therapy is the most reliable determinant of survival in patients with malignant bone tumors and soft tissue sarcomas (Picci et al. 1997; Eilber et al. 2001).
We conducted a randomized controlled trial to determine whether pathologic necrosis in response to preoperative treatment with UFT could be used to identify patients with colorectal cancer most likely to benefit from postoperative adjuvant therapy with the drug.
Patients and methods
Eligibility criteria
To be eligible for the study, patients had to have histologically proven adenocarcinoma of the colon or rectum, clinically curative resectable, an age of 75 years or younger, previously received no other cancer treatment, adequate organ function (a leukocyte count of at least the lower limit of 3,000/mm3, a platelet count of at least 100,000/mm3, a total bilirubin level of no more than 1.5 mg/dl, aspartate aminotaransferase and alanine aminotransferase levels of no more than 2.5× the upper limit of normal, and a serum creatinine level of no more than the upper limit of normal), and written informed consent.
Preoperative treatment
By outpatient treatment, UFT was given in an oral dose of 600 mg/day (200 mg, every 8 h) for 10 days just before the day of surgery.
Histopathologic assessment
Resected tumors were stained with hematoxylin and eosin. Two pathologists independently assessed pathologic necrosis. To rule out spontaneous necrosis, we defined UFT-induced pathologic necrosis as necrosis of at least 90% of a cross-section of the tumor center. This cutoff value was assigned from our previous study. In that study, 126 patients with colorectal cancer were also preoperatively treated by UFT. By histopathologic assessment, no necrosis, less than 50% tumor necrosis, 50% or over and less than 90% tumor necrosis, and 90% or over tumor necrosis were seen in 18% (23/126), 39% (49/126), 20% (25/126), and 28% (28/126) of patients, respectively (Fig. 1a–d). On the other hand, in the assessment of 48 of the non-UFT treated patients, no spontaneous necrosis, less than 50% spontaneous necrosis, 50% or over and less than 90% necrosis, and 90% or over necrosis were seen in 48% (23/48), 31% (15/48), 21% (10/48) and 0% (0/48) patients, respectively (Table 1). By these results, we employed 90% or over tumor necrosis as an appropriate cutoff value to avoid spontaneous necrosis of colorectal cancer.
Histopathologic assessment: resected tumors were stained with hematoxylin and eosin. a In this case, there was no UFT-induced pathologic necrosis at a cross-section of the tumor center. b In this case, tumor necrosis was seen, but this necrosis was less than 50% of the tumor at a cross-section of the tumor center. c In this case, tumor necrosis was seen in 90% or over of the tumor at a cross-section of the tumor center. d In this case, there was no viable cancer cell at a cross-section of the tumor center. In our previous study, 3 of 126 cases (2.4%) showed pathologically complete response by preoperative treatment of UFT
Study design
The patients were divided into two groups according to the rate of tumor necrosis in response to preoperative UFT: those with 90% or greater pathologic necrosis (sensitive) and those with less than 90% pathologic necrosis (insensitive). The patients were then randomly assigned according to a permuted-block scheme to receive UFT (400 mg/day, for 12 months) or no treatment (control) after surgery.
The primary endpoint was overall survival, and the secondary endpoint was relapse-free survival.
Statistical methods
The sample size was based on comparisons of 5-year survival rates. For the sensitive group, 40 patients were needed to detect a 35% difference in 5-year survival rates (from 60 to 95%) at 5% type I error and 80% power. Because our previous study (Fujii et al. 2000) showed that colorectal tumors were sensitive to preoperative UFT in about 28 of 126 patients (22.2%), the planned sample size was 160 patients. Data were analyzed according to intention to treat. Both survival curves were generated by the Kaplan–Meier method and compared by the log-rank test. For the patient’s characteristics, Chi-square test was used excepting age for which Wilcoxon test was used.
Results
Between 1992 and 1995, we enrolled 152 patients: 78 had colonic cancer and 74 had rectal cancer. Preoperatively, the median administered dose of UFT was 7.2 g (range 1.8–24.6 g). The 13 patients were found to be ineligible because of histological evidence of non-curative resection (eight patients), not primary tumor (two), and previous chemotherapy (three).
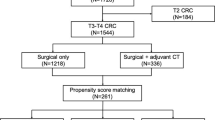
By histopathologic assessment for the 139 eligible patients, 22 patients (15.8%) were classified as having sensitive tumors (postoperative UFT 12, no adjuvant therapy 10) and 117 (84.2%) as having insensitive tumors (postoperative UFT 60, no adjuvant therapy 57) (Fig. 2).
Trial profile: 152 patients were enrolled in the trial, and 13 patients were found to be ineligible. On histopathologic assessment, 22 patients were classified as having sensitive tumors (postoperative UFT 12, no adjuvant therapy 10) and 117 (84.2%) as having insensitive tumors (postoperative UFT 60, no adjuvant therapy 57)
In patient’s characteristics of the sensitive group, the depth of invasion of the tumor in the UFT group was significantly better than the no adjuvant therapy group (P = 0.035). There was no significant difference in any other baseline characteristic between the sensitive group and the insensitive group (Table 2). Preoperative UFT was associated with no serious toxicity or operative complications. No grade 3 or 4 toxicity (World Health Organization criteria) occurred during postoperative treatment with UFT.
No patient was lost to follow-up. The median length of follow-up after surgery was 5.5 years (0.6–9.9). Among the patients with sensitive tumors, overall survival was significantly better in the UFT group (5-year survival rate 100%) than in the control group (70.0%, 95% CI 41.6–98.4%) (P = 0.023) (Fig. 3). Among those with insensitive tumors, survival was similar in the UFT group (5-year survival rate 68.1%, 95% CI 56.2–79.9) and the control group (76.6%, 65.5–87.8%) (P = 0.373). The rate of relapse-free survival at 5 years was significantly higher in the UFT group than in the control group among patients with sensitive tumors (100 vs. 60.0%, 95% CI 29.6–90.4%) (P = 0.009), but was similar among those with insensitive tumors (61.4%, 95% CI 49.1–73.8% vs. 66.4%, 95% CI 54.1–78.7%) (P = 0.632) (Fig. 4).
Overall survival: among the 22 patients with sensitive tumors, 5-year survival rate was significantly better in the UFT group (100%) than in the control group (70.0%) (P = 0.023). Among 117 patients with insensitive tumors, 5-year survival rate was similar in the UFT group (68.1%) and the control group (76.6%) (P = 0.373)
Relapse free survival: among the 22 patients with sensitive tumors, 5-year relapse free survival rate was significantly better in the UFT group (100%) than in the control group (60.0%) (P = 0.009). Among 117 patients with insensitive tumors, 5-year relapse free survival rate was similar in the UFT group (61.4%) and control group (66.4%) (P = 0.632)
Among patients who received UFT postoperatively, the relative risk for death was 0.0002 (95% CI 0.0001–0.691, P = 0.010) in the sensitive group, as compared with 1.173 in the insensitive group (95% CI 0.828–1.689, P = 0.371).
Discussion
Our randomized controlled study showed that assessment of pathologic necrosis in response to preoperative treatment with UFT can identify patients with colorectal cancer most likely to benefit from postoperative treatment with UFT, as well as those unlikely to benefit from such treatment.
UFT is commercially available since 1983 in Japan for gastric, colorectal, pancreas, breast, and lung carcinomas. A response rate of UFT for colorectal carcinoma is around 20% (Ota et al. 1988). UFT is commonly used for an adjuvant setting for curatively resected colorectal carcinoma without any evidence, by large randomized controlled studies in Japan when we started conducting this trial in 1992. Recently, the final results of randomized trials by the Japanese National Surgical Adjuvant Study of Colorectal Cancer (NSAS-CC) for adjuvant chemotherapy with UFT comparing surgery alone for stage III colorectal cancer was reported (Hamaguchi 2007). As the results show, there is significantly better relapse-free survival (RFS) in rectal cancer [5-year RFS UFT 68.9%, surgery alone 56.3%, hazard ratio = 0.66 (0.45–0.97), P = 0.0325]; however, there is no significantly better RFS in colon cancer [5-year RFS UFT 71.3%, surgery alone 69.6%, hazard ratio = 0.89 (0.60–1.32), P = 0.5586]. Then, there is still no evidence of the benefit of adjuvant UFT for colon cancer in Japan. We suppose that the reason for this negative impact is mainly the low power of the anti-tumor effect of UFT on colon cancer, showing that the cancer was not chemosensitive to UFT.
In our study, 5-year survival and relapse-free survival rates of the control group in sensitive tumors (70, 60%) seemed to be poorer than those in insensitive tumors (76.6, 66.4%). We speculate that these results were because, tumors with higher activity of cell division were sensitive to chemotherapy, but tumor progression of these tumors was faster than those with lower activity.
Because we employed a high cutoff value for pathologic necrosis to eliminate spontaneous necrosis, 18% of the patients who received preoperative oral UFT were predicted to have UFT-sensitive tumors. This value is similar to the rate of tumor sensitivity to UFT in the phase II study of this drug (Ota et al. 1988) and also the conventional treatment with 5-FU (loading or weekly bolus) in patients with metastatic colorectal cancer (Thirion et al. 2004).
UFT is now usually combined with leucovorin (LV) for the treatment of colorectal cancer (Pazdur 1997). A response rate of UFT/LV for advanced colorectal cancer is 42.2%. In our preliminary results for the preoperative use of UFT/LV, 90% or over necrosis was found in 14 cases in 34 preoperatively UFT/LV treated colorectal patients (sensitive rate of UFT/LV is 37.8%). The recent National Surgical Adjuvant Breast and Bowel Project (NSABP) adjuvant colon clinical trial (CO-6), comparing UFT/LV versus weekly regimen of intravenous 5-fluorouracil plus LV in the postoperative adjuvant therapy of Dukes’ B and C colon cancer patients, reported that there is no significant difference of both treatments (Lembersky et al. 2006). We believe that we can use the same method, used for UFT/LV adjuvant setting for colorectal cancer patients, for other agents including Capecitabine, FOLFOX, and FOLFIRI (Goldberg et al. 2004; Tournigand et al. 2004).
We conclude that pathologic tumor necrosis in response to preoperative UFT can be used to predict the response of colorectal tumors to postoperative adjuvant therapy with UFT. Patients whose tumors are insensitive to preoperative UFT should be given irinotecan or oxaliplatin as first-line chemotherapy in the event of recurrence. Our method is practical (requiring only routine pathologic examination), inexpensive, and highly predictable.
References
Bleiberg H (1998) Oxaliplatin (L-OHP): a new reality in colorectal cancer. Br J Cancer 77(Suppl 4):1–3
Douillard JY, Cunningham D, Roth AD, Navarro M, James RD, Karasek P et al (2000) Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet 355:1041–1047. doi:10.1016/S0140-6736(00)02034-1
Eilber FC, Rosen G, Eckaradt J, Forscher C, Nelson SD, Selch M et al (2001) Treatment-induced pathologic necrosis: a predictor of local recurrence and survival in patients receiving neoadjuvant therapy for high-grade extremity soft tissue sarcomas. J Clin Oncol 19:3203–3209
Fujii M, Kochi M, Kasakura Y (2000) Randomized trial of adjuvant chemotherapy by the results of histopathologic evaluation of patients with operable colorectal cancer following preoperative chemotherapy using UFT. J Clin Oncol 19:abstract 257a
Fujii S, Kitano S, Ikenaka K, Shirasaka T (1979) Effect of coadministration of uracil or cytosine on the anti-tumor activity of clinical doses of 1-(2-tetrahydrofulyl)-5-fluorouracil and level of 5-fluorouracil in rodents. Gann 70:209–214
Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK et al (2004) A randomized controlled trial of fluorouracil plus leucovorin, irinotecan and oxaliplatin combination in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 22:23–30. doi:10.1200/JCO.2004.09.046
Hamaguchi T (2007) Adjuvant chemotherapy with uracil–tegafur (UFT) for stage III colorectal cancer: final results of randomized trials by the National Surgical Adjuvant Study of Colorectal Cancer (NSAS-CC) ASCO 2007, abstract #4049
Ikenaka K, Shirasaka T, Kitano S, Fujii S (1979) Effect of uracil on metabolism of 5-fluorouracil in vitro. Gann 70:353–359
Lembersky BC, Wieand HS, Petrelli NJ, O’Connell MJ, Colangelo LH, Smith RE et al (2006) Oral uracil and tegafur plus leucovorin compared with intravenous fluorouracil and leucovorin in stage II and III carcinoma of the colon: results from National Surgical Adjuvant Breast and Bowel Project Protocol C-06. J Clin Oncol 24:2059–2064. doi:10.1200/JCO.2005.04.7498
Ota K, Taguchi T, Kimura K (1988) Report on nationwide pooled data and cohort investigation in UFT phase II study. Cancer Chemother Pharmacol 22:333–338. doi:10.1007/BF00254241
Pazdur R (1997) Phase II study of UFT plus leucovorin in colorectal cancer. Oncology 54(Suppl 1):19–23
Picci P, Bohling T, Bacci G, Ferrari S, Sangiorgi L, Mercuri M et al (1997) Chemotherapy-induced tumor necrosis as a prognostic factor in localized Ewing’s sarcoma of extremities. J Clin Oncol 15:1553–1559
Punt CJ (1998) New drugs in the treatment of colorectal carcinoma. Cancer 83:679–689. doi:10.1002/(SICI)1097-0142(19980815)83:4<679::AID-CNCR8>3.0.CO;2-F
Thirion P, Michiels S, Pignon JP, Buyse M, Braud AC, Carlson RW et al (2004) Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: an updated meta-analysis. J Clin Oncol 22:3766–3775. doi:10.1200/JCO.2004.03.104
Tournigand C, Andre T, Achille E, Liedo G, Flesh M, Mery-Mignard D et al (2004) FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GEOCOR study. J Clin Oncol 22:229–237. doi:10.1200/JCO.2004.05.113
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Fujii, M., Takayama, T. & Kochi, M. Clinical identification of colorectal cancer patients benefiting from adjuvant uracil–tegafur (UFT): a randomized controlled trial. J Cancer Res Clin Oncol 134, 1319–1323 (2008). https://doi.org/10.1007/s00432-008-0417-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-008-0417-z