Abstract
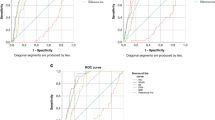
This study aimed to estimate the prevalence of metabolically healthy obesity (MHO) according to two different consensus-based criteria and to investigate simple, measurable predictive markers for the diagnosis of MHO. Five hundred and ninety-three obese children and adolescents aged 6–18 years were included in the study. The frequency of MHO was calculated. ROC analysis was used to estimate the predictive value of AST/ALT ratio, waist/hip ratio, MPV, TSH, and Ft4 cut-off value for the diagnosis of MHO. The prevalence of MHO was 21.9% and 10.2% according to 2018 and 2023 consensus-based MHO criteria, respectively. AST/ALT ratio cut-off value for the diagnosis of MHO was calculated as ≥ 1 with 77% sensitivity and 52% specificity using Damanhoury et al.’s criteria (AUC = 0.61, p = 0.02), and 90% sensitivity and 51% specificity using Abiri et al.’s criteria (AUC = 0.70, p = 0.01). Additionally, using binomial regression analysis, only the AST/ALT ratio is independently and significantly associated with the diagnosis of MHO (p = 0.03 for 2018 criteria and p = 0.04 for 2023 criteria).
Conclusion: The ALT/AST ratio may be a useful indicator of MHO in children and adolescents.
What is Known: • Metabolically healthy obesity refers to people who are obese but do not have any of the standard cardio-metabolic risk factors. • Metabolically healthy obesity is not entirely harmless; the metabolic characteristics of individuals with this phenotype are less favorable than those of healthy lean groups. Moreover, it is not a constant state, and there may be a transition to metabolically unhealthy phenotypes over time. | |
What is New: • The prevalence of MHO is 21.9% and 10.2% according to 2018 and 2023 consensus-based metabolically healthy obesity criteria, respectively. • The ALT/AST ratio may be a useful indicator of metabolically healthy obesity in children and adolescents. |


Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Code availability
NA.
Abbreviations
- AGA:
-
Appropriate for gestational age
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- DBP:
-
Diastolic blood pressure
- GW:
-
Gestational week
- HC:
-
Hip circumference
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostasis model of insulin resistance
- LDL:
-
Low-density lipoprotein
- LGA:
-
Large for gestational age
- MCV:
-
Mean corpuscular volume
- MHO:
-
Metabolically healthy obesity
- MPV:
-
Mean platelet volume
- MUO:
-
Metabolically unhealthy obesity
- ROC:
-
Receiver operating characteristic
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SDS:
-
Standard deviation score
- SGA:
-
Small for gestational age
- SHT:
-
Subclinical hypothyroidism
- SPSS:
-
Statistical Package for Social Sciences
- TSH:
-
Thyroid stimulating hormone
- WBC:
-
White blood cells
- WC:
-
Waist circumference
- WHO:
-
World Health Organization
References
Lister NB, Baur LA, Felix JF, Hill AJ, Marcus C, Reinehr T, Summerbell C, Wabitsch M (2023) Child and adolescent obesity. Nat Rev Dis Primers 9(1):24. https://doi.org/10.1038/s41572-023-00435-4
Alper Z, Ercan İ, Uncu Y (2018) A meta-analysis and an evaluation of trends in obesity prevalence among children and adolescents in Turkey: 1990 through 2015. JCRPE J Clin Res Pediatr Endocrinol 10:59–67. https://doi.org/10.4274/jcrpe.5043
Jacobs DR, Woo JG, Sinaiko AR et al (2022) Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med 386:1877–1888. https://doi.org/10.1056/NEJMoa2109191
Bonora E, Kiechl S, Willeit J et al (1998) Prevalence of insulin resistance in metabolic disorders: the Bruneck Study. Diabetes 47:1643–1649. https://doi.org/10.2337/diabetes.47.10.1643
Semlitsch T, Stigler FL, Jeitler K et al (2019) Management of overweight and obesity in primary care—a systematic overview of international evidence-based guidelines. Obes Rev 20:1218–1230. https://doi.org/10.1111/obr.12889
Lahav Y, Kfir A, Gepner Y (2023) The paradox of obesity with normal weight; a cross-sectional study. Front Nutr 10:1173488. https://doi.org/10.3389/fnut.2023.1173488
Abiri B, Valizadeh M, Amini S et al (2023) Risk factors, cutoff points, and definition of metabolically healthy/unhealthy obesity in children and adolescents: a scoping review of the literature. Obes Rev 24:e13548. https://doi.org/10.1111/obr.13548
Damanhoury S, Newton AS, Rashid M et al (2018) Defining metabolically healthy obesity in children: a scoping review: MHO definition in children. Obes Rev 19:1476–1491. https://doi.org/10.1111/obr.12721
Dundar I, Akinci A (2023) Prevalence and predictive clinical characteristics of metabolically healthy obesity in obese children and adolescents. Cureus 15(3):e35935. https://doi.org/10.7759/cureus.35935
Keskin M, Kurtoglu S, Kendirci M et al (2005) Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 115:e500-503. https://doi.org/10.1542/peds.2004-1921
Valerio G, Licenziati MR, Iannuzzi A et al (2006) Insulin resistance and impaired glucose tolerance in obese children and adolescents from Southern Italy. Nutr Metab Cardiovasc Dis NMCD 16:279–284. https://doi.org/10.1016/j.numecd.2005.12.007
Biondi B, Cooper DS (2008) The clinical significance of subclinical thyroid dysfunction. Endocr Rev 29:76–131. https://doi.org/10.1210/er.2006-0043
Zamrazilova H, Weiss R, Hainer V, Aldhoon-Hainerová I (2016) Cardiometabolic health in obese adolescents is related to length of obesity exposure: a pilot study. J Clin Endocrinol Metab 101:3088–3095. https://doi.org/10.1210/jc.2016-1706
Li S, Chen W, Srinivasan SR et al (2012) Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol 176(Suppl 7):S142-149. https://doi.org/10.1093/aje/kws236
Dalla Valle M, Laatikainen T, Kalliokoski T et al (2015) Childhood obesity in specialist care—searching for a healthy obese child. Ann Med 47:639–654. https://doi.org/10.3109/07853890.2015.1083118
Remor JM, Lopes WA, Locateli JC et al (2019) Prevalence of metabolically healthy obese phenotype and associated factors in South American overweight adolescents: a cross-sectional study. Nutrition 60:19–24. https://doi.org/10.1016/j.nut.2018.08.017
Alvehus M, Burén J, Sjöström M et al (2010) The human visceral fat depot has a unique inflammatory profile. Obes Silver Spring Md 18:879–883. https://doi.org/10.1038/oby.2010.22
Elmaogullari S, Demirel F, Hatipoglu N (2017) Risk factors that affect metabolic health status in obese children. J Pediatr Endocrinol Metab 30(1):49–55. https://doi.org/10.1515/jpem-2016-0128
Marra NF, Bechere Fernandes MT, de Melo ME et al (1992) (2019) Fasting insulin resistance affects the prevalence of metabolically healthy obesity in Brazilian adolescents. Acta Paediatr Oslo Nor 108:1295–1302. https://doi.org/10.1111/apa.14684
Heinzle S, Ball GDC, Kuk JL (2016) Variations in the prevalence and predictors of prevalent metabolically healthy obesity in adolescents. Pediatr Obes 11:425–433. https://doi.org/10.1111/ijpo.12083
Fu J, Li Y, Esangbedo IC et al (2018) Circulating osteonectin and adipokine profiles in relation to metabolically healthy obesity in Chinese children: findings from BCAMS. J Am Heart Assoc 7:e009169. https://doi.org/10.1161/JAHA.118.009169
Pacifico L, Poggiogalle E, Costantino F et al (2009) Acylated and nonacylated ghrelin levels and their associations with insulin resistance in obese and normal weight children with metabolic syndrome. Eur J Endocrinol 161:861–870. https://doi.org/10.1530/EJE-09-0375
Rocha EPAA, Vogel M, Stanik J et al (2018) Serum uric acid levels as an indicator for metabolically unhealthy obesity in children and adolescents. Horm Res Paediatr 90:19–27. https://doi.org/10.1159/000490113
Engelmann G, Hoffmann GF, Grulich-Henn J, Teufel U (2014) Alanine aminotransferase elevation in obese infants and children: a marker of early onset non alcoholic Fatty liver disease. Hepat Mon 14:e14112. https://doi.org/10.5812/hepatmon.14112
Elizondo-Montemayor L, Ugalde-Casas PA, Lam-Franco L et al (2014) Association of ALT and the metabolic syndrome among Mexican children. Obes Res Clin Pract 8:e79-87. https://doi.org/10.1016/j.orcp.2012.08.191
Ooi DSQ, Ong SG, Lee OMH et al (2022) Prevalence and predictors of metabolically healthy obesity in severely obese Asian children. Pediatr Res 92:1374–1380. https://doi.org/10.1038/s41390-022-01941-z
Jeong S, Jang H-B, Kim H-J, Lee H-J (2023) Identification of biomarkers related to metabolically unhealthy obesity in Korean obese adolescents: a cross-sectional study. Children 10:322. https://doi.org/10.3390/children10020322
Akduman F, Şıklar Z, Özsu E et al (2022) Fibroblast growth factor 21 levels and bone mineral density in metabolically healthy and metabolically unhealthy obese children. J Clin Res Pediatr Endocrinol 14:433–443. https://doi.org/10.4274/jcrpe.galenos.2022.2022-1-15
Vos MB, Abrams SH, Barlow SE et al (2017) NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr 64:319. https://doi.org/10.1097/MPG.0000000000001482
Titmuss AT, Srinivasan S (2016) Metabolic syndrome in children and adolescents: old concepts in a young population. J Paediatr Child Health 52:928–934. https://doi.org/10.1111/jpc.13190
Beysel P, Çeli̇k N (2022) Obez çocuk ve ergenlerde metabolik sendrom sıklığı ve subklinik hipotiroidinin araştırılması: retrospektif tek merkezli gözlemsel bir çalışma: Investigation of metabolic syndrome frequency and subclinical hypothyroidism in obese children and adolescents: a retrospective single center observational study. Turk Klin J Pediatr 31:9–18. https://doi.org/10.5336/pediatr.2021-83667
Çelik N (2019) The prevalence of subclinical hypothyroidism in obese children and adolescents and its effects on metabolic parameters. Cumhur Med J. https://doi.org/10.7197/cmj.vi.551051
Januszek-Trzciąkowska A, Małecka-Tendera E (2013) Subclinical hypothyroidism in obese children. Postepy Hig Med Doswiadczalnej Online 67:770–774. https://doi.org/10.5604/17322693.1061415
Abiri B, Ahmadi AR, Mahdavi M et al (2023) Association between thyroid function and obesity phenotypes in healthy euthyroid individuals: an investigation based on Tehran Thyroid Study. Eur J Med Res 28:179. https://doi.org/10.1186/s40001-023-01135-1
Nkambule BB, Mxinwa V, Nyambuya TM, Dludla PV (2022) The mean platelet volume and atherosclerotic cardiovascular-risk factors in adults with obesity: a systematic review and meta-analysis of observational studies. BMC Nutr 8:47. https://doi.org/10.1186/s40795-022-00541-8
Kalyoncu D (2023) Platelet indices in overweight and obese children. Eur J Pediatr. https://doi.org/10.1007/s00431-023-05082-1
Zhao M, López-Bermejo A, Caserta CA et al (2019) Metabolically healthy obesity and high carotid intima-media thickness in children and adolescents: International Childhood Vascular Structure Evaluation Consortium. Diabetes Care 42:119–125. https://doi.org/10.2337/dc18-1536
Serbis A, Giapros V, Paschou SA, Siomou E (2021) Children with metabolically healthy obesity have a worse metabolic profile compared to normal-weight peers: a cross-sectional study. Endocrine 73:580–587. https://doi.org/10.1007/s12020-021-02762-6
Phillips CM (2017) Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Ann N Y Acad Sci 1391:85–100. https://doi.org/10.1111/nyas.13230
Author information
Authors and Affiliations
Contributions
NÇ: conception and design of the study, acquisition of the data, contribution to analysis, interpretation of data, revising it critically for important intellectual content. GÜ: conception and design of the study, acquisition of the data, contribution to analysis, interpretation of data. HT: conception and design of the study, acquisition of the data, revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval
The institutional ethics committee approved the study protocol (2023-06/17).
Consent to participate
Written informed assent and consent were obtained from all participants and their parents before any procedures.
Consent for publication
All authors consent to the publication of the manuscript in EJPE.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Çelik, N., Ünsal, G. & Taştanoğlu, H. Predictive markers of metabolically healthy obesity in children and adolescents: can AST/ALT ratio serve as a simple and reliable diagnostic indicator?. Eur J Pediatr 183, 243–251 (2024). https://doi.org/10.1007/s00431-023-05296-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05296-3