Abstract
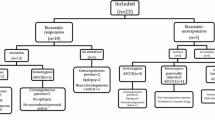
Persistent hypoglycaemia in newborns and infants is most commonly caused by congenital hyperinsulinism (CHI). Most CHI studies report outcomes in children from both consanguineous and non-consanguineous families which can affect the phenotype-genotype analysis. The aim of this study was to analyze characteristics of patients with CHI in 21 non-consanguineous families from Serbia. This retrospective cohort study included a total of 21 patients with CHI treated in the Mother and Child Healthcare Institute of Serbia during the past 20 years. The prevalence of macrosomia at birth was very low in our cohort (4.8%). Median age at presentation was 6 days, with seizures as the presenting symptom in 76% of patients. Only four patients (19%) were diazoxide unresponsive, and eventually underwent pancreatectomy. Genetic testing was performed in 15 patients and genetic diagnosis was confirmed in 60%, with all patients being heterozygous for detected mutations. The ABCC8 gene mutations were detected in 55.6%, GLUD1 in three patients (33.3%) with HIHA syndrome and one patient had HNF4A gene mutation and unusual prolonged hyperglycaemia lasting 6 days after diazoxide cessation. Neurodevelopmental deficits persisted in 33% of patients.
Conclusion: This is the first study regarding CHI patients in Serbia. It suggests that in countries with low consanguinity rate, majority of CHI patients are diazoxide responsive. The most common mutations were heterozygous ABCC8, followed by GLUD1 and HNF4A mutations, suggesting the potential benefit of population-tailored genetic analysis approach, targeting the mutations causing CHI via dominant inheritance model in regions with low consanguinity rates.
What is Known: • Persistent hypoglycaemia during infancy and early childhood is most commonly caused by congenital hyperinsulinism (CHI). • Consanguinity is a very important factor regarding the genetics and phenotype of CHI, increasing the risk of autosomal recessive genetic disorders, including the severe, diazoxide-unresponsive forms caused by recessive inactivating mutations in ABCC8 and KCNJ11. | |
What is New: • Results of the present study which included CHI patients from 21 non-consanguineous families suggest that in countries with low consanguinity rates, majority of CHI patients can be diazoxide responsive, with most common mutations being heterozygous ABCC8, followed by GLUD1 and HNF4A mutations. • Unusually prolonged hyperglycaemic reaction to diazoxide treatment in a patient with HNF4A mutation was also described in the present study. |
Similar content being viewed by others
Data availability
Anonymized data can be provided by the authors upon request.
Code availability
N/A.
Abbreviations
- 18F-DOPA-PET:
-
18F-fluoro-dihydroxyphenylalanine positron emission tomography
- ABCC8:
-
ATP-binding cassette subfamily C member 8
- CHI:
-
Congenital hyperinsulinism
- GLUD1:
-
Glutamate dehydrogenase 1
- HNF4A:
-
Hepatocyte nuclear factor 4 alpha
- HIHA:
-
Hyperinsulinism-hyperammonemia syndrome
- KCNJ11:
-
Potassium inwardly rectifying channel subfamily J member 11
References
Rahman SA, Nessa A, Hussain K (2015) Molecular mechanisms of congenital hyperinsulinism. J Mol Endocrinol 54:119–129. https://doi.org/10.1530/JME-15-0016
Shah R, Harding J, Brown J, McKinlay C (2019) Neonatal glycaemia and neurodevelopmental outcomes: a systematic review and meta-analysis. Neonatology. 115:116–126
Aynsley-Green A, Hussain K, Hall J, Saudubray JM, NihoulFékété C, de Lonlay-Debeney P et al (2000) Practical management of hyperinsulinism in infancy. Arch Dis Child Fetal Neonatal Ed 82(2):F98–F107
Yorifuji T, Horikawa R, Hasegawa T, Adachi M, Soneda S, Minagawa M, Ida S, Yonekura T, Kinoshita Y, Kanamori Y, Kitagawa H, Shinkai M, Sasaki H, Nio M, (on behalf of The Japanese Society for Pediatric Endocrinology and The Japanese Society of Pediatric Surgeons) (2017) Clinical practice guidelines for congenital hyperinsulinism. Clin Pediatr Endocrinol 26(3):127–152
Senniappan S, Arya VB, Hussain K (2013) The molecular mechanisms, diagnosis and management of congenital hyperinsulinism. Indian J Endocrinol Metab 17(1):19–30
Mathew PM, Young JM, Abu-Osba YK, Mulhern BD, Hammoudi S, Hamdan JA, Sa'di AR (1988) Persistent neonatal hyperinsulinism. Clin Pediatr (Phila) 27:148–151
Stevenson AC, Johnston HA, Stewart M, Golding DR (1966) Congenital malformations: a report of a study of series of consecutive births in 24 centres. Bull World Health Organ 34(Suppl):1–127
Snider KE, Becker S, Boyajian L, Shyng SL, MacMullen C, Hughes N, Ganapathy K, Bhatti T, Stanley CA, Ganguly A (2013) Genotype and phenotype correlations in 417 children with congenital hyperinsulinism. J Clin Endocrinol Metab 98(2):E355–E363
Alaei M, Akbaroghli D, Keramatipour M, Alaei A (2016) A case series: congenital hyperinsulinism. Int J Endocrinol Metab 14:e37311
James C, Kapoor RR, Ismail D, Hussain K (2009) The genetic basis of congenital hyperinsulinism. J Med Genet 46(5):289–299
Kapoor RR, Flanagan SE, Arya VB, Shield JP, Ellard S, Hussain K (2013) Clinical and molecular characterisation of 300 patients with congenital hyperinsulinism. Eur J Endocrinol 168:557–564
Cabezas OR, Flanagan SE, Stanescu H, García-Martínez E, Caswell R, Lango-Allen H, Antón-Gamero M, Argente J, Bussell AM, Brandli A, Cheshire C, Crowne E, Dumitriu S, Drynda R, Hamilton-Shield JP, Hayes W, Hofherr A, Iancu D, Issler N, Jefferies C, Jones P, Johnson M, Kesselheim A, Klootwijk E, Koettgen M, Lewis W, Martos JM, Mozere M, Norman J, Patel V, Parrish A, Pérez-Cerdá C, Pozo J, Rahman SA, Sebire N, Tekman M, Turnpenny PD, Hoff W’, Viering DHHM, Weedon MN, Wilson P, Guay-Woodford L, Kleta R, Hussain K, Ellard S, Bockenhauer D (2017) Polycystic kidney disease with hyperinsulinemic hypoglycemia caused by a promoter mutation in phosphomannomutase 2. J Am Soc Nephrol 28(8):2529–2539
Gregory LC, Ferreira CB, Young-Baird SK, Williams HJ, Harakalova M, van Haaften G, Rahman SA, Gaston-Massuet C, Kelberman D, GOSgene, Qasim W, Camper SA, Dever TE, Shah P, Robinson ICAF, Dattani MT (2019) Impaired EIF2S3 function associated with a novel phenotype of X-linked hypopituitarism with glucose dysregulation. EBioMedicine. 42:470–480
Rozenkova K, Guemes M, Shah P, Hussain K (2015) The diagnosis and management of hyperinsulinaemic hypoglycaemia. J Clin Res Pediatr Endocrinol 7:86–97
Pinney SE, Ganapathy K, Bradfield J, Stokes D, Sasson A, Mackiewicz K, Boodhansingh K, Hughes N, Becker S, Givler S, Macmullen C, Monos D, Ganguly A, Hakonarson H, Stanley CA (2013) Dominant form of congenital hyperinsulinism maps to HK1 region on 10q. Horm Res Paediatr 80:18–27
Tegtmeyer LC, Rust S, van Scherpenzeel M, Ng BG, Losfeld ME, Timal S, Raymond K, He P, Ichikawa M, Veltman J, Huijben K, Shin YS, Sharma V, Adamowicz M, Lammens M, Reunert J, Witten A, Schrapers E, Matthijs G, Jaeken J, Rymen D, Stojkovic T, Laforêt P, Petit F, Aumaître O, Czarnowska E, Piraud M, Podskarbi T, Stanley CA, Matalon R, Burda P, Seyyedi S, Debus V, Socha P, Sykut-Cegielska J, van Spronsen F, de Meirleir L, Vajro P, DeClue T, Ficicioglu C, Wada Y, Wevers RA, Vanderschaeghe D, Callewaert N, Fingerhut R, van Schaftingen E, Freeze HH, Morava E, Lefeber DJ, Marquardt T (2014) Multiple phenotypes in phosphoglucomutase 1 deficiency. N Engl J Med 370:533–542
Flanagan SE, Vairo F, Johnson MB, Caswell R, Laver TW, Lango Allen H, Hussain K, Ellard S (2017) A CACNA1D mutation in a patient with persistent hyperinsulinaemic hypoglycaemia, heart defects, and severe hypotonia. Pediatr Diabetes 18(4):320–323
Giri D, Vignola ML, Gualtieri A, Scagliotti V, McNamara P, Peak M, Didi M, Gaston-Massuet C, Senniappan S (2017) Novel FOXA2 mutation causes hyperinsulinism, hypopituitarism with craniofacial and endoderm-derived organ abnormalities. Hum Mol Genet 26:4315–4326
Arnoux JB, Verkarre V, Saint-Martin C, Montravers F, Brassier A, Valayannopoulos V, Brunelle F, Fournet JC, Robert JJ, Aigrain Y, Bellanné-Chantelot C, de Lonlay P (2011) Congenital hyperinsulinism: current trends in diagnosis and therapy. Orphanet J Rare Dis 6:63
Welters A, Lerch C, Kummer S, Marquard J, Salgin B, Mayatepek E, Meissner T (2015) Long-term medical treatment in congenital hyperinsulinism: a descriptive analysis in a large cohort of patients from different clinical centers. Orphanet J Rare Dis 10:150
Demirbilek H, Shah P, Arya VB, Hinchey L, Flanagan SE, Ellard S, Hussain K (2014) Long-term follow-up of children with congenital hyperinsulinism on octreotide therapy. J Clin Endocrinol Metab 99(10):3660–3667
Adzick NS et al (2018) Surgical treatment of congenital hyperinsulinism: results from 500 pancreatectomies in neonates and children. J Pediatr Surg 54:27–32
Demirbilek H, Arya VB, Ozbek MN, Akinci A, Dogan M, Demirel F, Houghton J, Kaba S, Guzel F, Baran RT, Unal S (2014) Clinical characteristics and phenotype-genotype analysis in Turkish patients with congenital hyperinsulinism; predominance of recessive KATP channel mutations. Eur J Endocrinol 170(6):885–892
Mohnike K, Wieland I, Barthlen W, Vogelgesang S, Empting S, Mohnike W, Meissner T, Zenker M (2014) Clinical and genetic evaluation of patients with KATP channel mutations from the German registry for congenital hyperinsulinism. Horm Res Paediatr 81:156–168
Al-Agha AE, Ahmad IA (2013) Characterization of the ABCC8 gene mutation and phenotype in patients with congenital hyperinsulinism in western Saudi Arabia. Saudi Med J 34:1002–1006
Martínez R, Fernández-Ramos C, Vela A, Velayos T, Aguayo A, Urrutia I, Rica I, Castaño L (2016) Clinical and genetic characterization of congenital hyperinsulinism in Spain. Eur J Endocrinol 174(6):717–726
Faletra F, Athanasakis E, Morgan A, Biarnés X, Fornasier F, Parini R, Furlan F, Boiani A, Maiorana A, Dionisi-Vici C, Giordano L (2013) Congenital hyperinsulinism: clinical and molecular analysis of a large Italian cohort. Gene. 521(1):160–165
Casertano A, De Matteis A, Mozzillo E, Rosanio FM, Buono P, Fattorusso V, Franzese A (2020) Diagnosis of congenital hyperinsulinism can occur not only in infancy but also in later age: a new flow chart from a single center experience. Ital J Pediatr 46(1):131
Thomas PM, Cote GJ, Wohllk N, Haddad B, Mathew PM, Rabl W, Aguilar-Bryan L, Gagel R, Bryan J (1995) Mutations in the sulfonylurea receptor gene in familial persistent hyperinsulinemic hypoglycemia of infancy. Science. 268(5209):426–429
Thomas P, Ye Y, Lightner E (1996) Mutation of the pancreatic islet inward rectifier Kir6.2 also leads to familial persistent hyperinsulinemic hypoglycemia of infancy. Hum Mol Genet 5(11):1809–1812
Wang WY, Sun Y, Zhao WT, Wu T, Wang L, Yuan TM, Yu HM (2017) Congenital hyperinsulinism in China: a review of Chinese literature over the past 15 years. J Clin Res Pediatr Endocrinol 9(3):194–201
El Tonbary K, Robinson P, Banerjee I, Shaikh MG (2020) Congenital hyperinsulinism: management and outcome, a single tertiary centre experience. Eur J Pediatr 179:947–952
Şiklar Z, Berberoğlu M (2016) Current status of childhood hyperinsulinemic hypoglycemia in Turkey. J Clin Res Pediatr Endocrinol 8(4):375–380
Sarajlija A, Milenkovic T, Djordjevic M, Mitrovic K, Todorovic S, Kecman B, Hussain K (2016) Early presentation of hyperinsulinism/hyperammonemia syndrome in three Serbian patients. J Clin Res Pediatr Endocrinol 8:228–231
Kapoor R, Heslegrave A, Hussain K (2010) Congenital hyperinsulinism due to mutations in HNF4A and HADH. Rev Endocr Metab Disord 11:185–191
Chandran S, Rajadurai VS, Hoi WH, Flanagan SE, Hussain K, Yap F (2020) A novel HNF4A mutation causing three phenotypic forms of glucose dysregulation in a family. Front Pediatr 8:320. https://doi.org/10.3389/fped.2020.00320
Acknowledgements
We would like to express our deepest thanks to Professor Dr. Sarah Flanagan and other members of the Exeter Molecular Genetics Laboratory team for providing genetic testing for CHI.
Author information
Authors and Affiliations
Contributions
MR and RV designed the research study. MR gathered the data, conducted statistical analyses and wrote the first draft of the manuscript. All authors contributed to the study design, revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Hospital Ethics Committee and conducted in accordance with the Declaration of Helsinki.
Consent to participate
Having in mind the retrospective design and data anonymization in the present study, the need for consent to participate was waived by the Hospital Ethics Committee.
Consent for publication
Having in mind the retrospective design and data anonymization in the present study, the need for consent to participate was waived by the Hospital Ethics Committee.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raicevic, M., Milenkovic, T., Hussain, K. et al. Clinical and genetic characteristics of patients with congenital hyperinsulinism in 21 non-consanguineous families from Serbia. Eur J Pediatr 180, 2815–2821 (2021). https://doi.org/10.1007/s00431-021-04051-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04051-w