Abstract
Hypertensive disorders of pregnancy are complications that can lead to maternal and infant mortality and morbidity. Hypertensive disorders of pregnancy are generally defined as hypertension and may be accompanied by other end organ damages including proteinuria, maternal organ disturbances including renal insufficiency, neurological complications, thrombocytopenia, impaired liver function, or uteroplacental dysfunction such as fetal growth restriction and stillbirth. Although the causes of these hypertensive disorders of pregnancy are multifactorial and elusive, they seem to share some common vascular-related mechanisms, including diseased spiral arteries, placental ischemia, and endothelial dysfunction. Recently, preeclampsia is being considered as a vascular disorder. Unfortunately, due to the complex etiology of preeclampsia and safety concerns on drug usage during pregnancy, there is still no effective pharmacological treatments available for preeclampsia yet. An emerging area of interest in this research field is the potential beneficial effects of dietary intervention on reducing the risk of preeclampsia. Recent studies have been focused on the association between deficiencies or excesses of some nutrients and complications during pregnancy, fetal growth and development, and later risk of cardiovascular and metabolic diseases in the offspring. In this review, we discuss the involvement of placental vascular dysfunction in preeclampsia. We summarize the current understanding of the association between abnormal placentation and preeclampsia in a vascular perspective. Finally, we evaluate several studied dietary supplementations to prevent and reduce the risk of preeclampsia, targeting placental vascular development and function, leading to improved pregnancy and postnatal outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization (WHO), the worldwide maternal mortality is unacceptably high [1]. In 2017, approximately 810 women died each day from pregnancy-related complications [1]. Maternal mortality is the result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy while some complications may exist before pregnancy and are worsened during pregnancy. The major complications that lead to most maternal deaths include severe bleeding during childbirth, infections, unsafe abortion, high blood pressure during pregnancy, and other causes associated with chronic diseases like diabetes [2]. Indeed, most of these complications are largely preventable and can be improved with better hygiene condition and healthcare facilities. However, among these complications, hypertensive disorders of pregnancy, including gestational hypertension, pre-eclampsia, and eclampsia, can only be minimized via pharmacological and dietary interventions. Also, pregnancy-associated hypertensive disorders occur in approximately 10% of all pregnancies and account for approximately 14% of maternal mortality [3, 4]. Hypertensive disorders of pregnancy are generally defined as hypertension (≥ 140 mmHg systolic and/or ≥ 90 mmHg diastolic blood pressure) occurring after 20 weeks of gestation while preeclampsia is defined as gestational hypertension accompanied by proteinuria (excretion of ≥ 300 mg protein every 24 h) [5]. Apart from maternal mortality, these hypertensive disorders of pregnancy can lead to an increased risk for future metabolic and cardiovascular disease for both mother and offspring [6, 7]. Therefore, the identification of better preventive strategies and treatment modalities is imperative to minimize these inter-generational pathological consequences of pregnancy-related complications. Despite the fact that the causes of these hypertensive disorders of pregnancy are multifactorial and elusive, they seem to share some common vascular-related mechanisms, including diseased spiral arteries, placental ischemia, and endothelial dysfunction [8,9,10]. Various studies have shown that dietary patterns and supplements can influence adverse pregnancy and birth outcomes [11,12,13]. This review aims to summarize the current understanding of the beneficial effects of different dietary supplementations in hypertensive disorders of pregnancy, focusing on vascular function.
Hypertensive disorders of pregnancy and vascular function
The exact mechanisms underlying the development of hypertensive disorders of pregnancy are unclear. Currently, most of the literature has specifically focused on the pathogenesis underlying preeclampsia, while few of them have discussed on gestational hypertension, although gestational hypertension is also associated with adverse maternal and perinatal outcomes, and similar renal histopathology [14,15,16]. Traditionally, significant proteinuria has been the second criterion required to distinguish between gestational hypertension and preeclampsia. Indeed, various maternal and fetal consequences now appear in international guidelines for the diagnosis of preeclampsia, including hypertension and end-organ dysfunction, while proteinuria is no longer mandatory [17,18,19]. Therefore, the review will primarily focus on the pathogenesis of preeclampsia.
Preeclampsia is a complex and multifactorial disease defined as a rise in systolic blood pressure above 140 mmHg and/or rise in diastolic blood pressure above 90 mmHg occurring after 20 weeks of gestation in a pregnant woman without prior hypertension [5, 20], accompanied by the occurrence of at least one of the following complications at or after 20 weeks of gestation: proteinuria, maternal organ disturbances including renal insufficiency, neurological complications, thrombocytopenia, impaired liver function, or uteroplacental dysfunction such as fetal growth restriction and stillbirth [17,18,19]. Superimposed preeclampsia is defined as the development of any of the above-mentioned maternal organ dysfunctions in a mother with pre-existing chronic hypertension [21]. If untreated, preeclampsia can lead to eclampsia. Eclampsia is the development of seizures in pre-existing preeclampsia and is a life-threatening emergency condition that can also occur in the postpartum period [22] (Fig. 1). Although eclampsia is one of the leading causes of maternal mortality, it is not known how hypertension in pregnancy affects the cerebral circulation and causes eclampsia due to the lack of animal models [23]. The primary explanation for the pathogenesis of eclampsia is thought to be hypertensive encephalopathy [24]. In addition, preeclampsia may persist during antepartum and postpartum. Late postpartum preeclampsia is defined as the presence of preeclampsia symptoms up to 6 weeks postpartum [25]. Although the detailed pathophysiology is relatively unknown, the persistently high levels of anti-angiogenic factors after delivery may play a role in the development of postpartum preeclampsia [26]. Postpartum preeclampsia may cause endothelial damage associated with substantial maternal mortality and increased risk of chronic hypertension [25, 27].
Diagram showing different hypertensive disorders of pregnancy. Gestation hypertension is the increase in blood pressure during pregnancy. Preeclampsia patients have gestation hypertension and accompanied by the occurrence of at least one of the following complications at or after 20 weeks of gestation: proteinuria, maternal organ disturbances including renal insufficiency, neurological complications, thrombocytopenia, impaired liver function, or uteroplacental dysfunction such as fetal growth restriction and stillbirth. Women with chronic hypertension who develop symptoms of preeclampsia are diagnosed with superimposed preeclampsia. Eclampsia is the development of seizures in pre-existing preeclampsia and is a life-threatening emergency condition. Postpartum preeclampsia may also occur when the symptoms of preeclampsia persist in postpartum, which may increase the risk of chronic cardiovascular diseases.
Women with history of preeclampsia have approximately 2-fold increased risk of developing cardiovascular diseases and around 10-fold increased risk of chronic kidney diseases [28]. Also, a few epidemiologic studies have linked 15–20% of all fetal growth restriction and small for gestational age infants to preeclampsia, while 20% of all preterm births are also associated with preeclampsia [29]. Apart from obstetric and neonatal consequences, preeclampsia has also been shown to exert long-term risk of metabolic and cardiovascular complications [30]. Therefore, hypertensive disorders of pregnancy can leave long-term metabolic and cardiovascular risks to both mother and child.
Placenta plays an important role in the development and severity of preeclampsia. It has been suggested that the placenta itself, but not the fetus, is necessary for the development of preeclampsia, while preeclampsia can also occur in patients with hydatidiform moles and the removal of placenta can resolve the syndrome [31, 32]. Accumulating studies have evidenced the involvement of multifactorial mechanisms including early disturbances in placentation followed by the imbalance in angiogenic factors, aberrant inflammatory response, increased placental oxidative stress, and placental aging in the pathogenesis of preeclampsia [33, 34]. Indeed, preeclampsia can be considered as a vascular disorder. A functional and adequately vascularized placenta is crucial for healthy pregnancy and birth outcome [35]. It is proposed that the initiating step in the pathogenesis of preeclampsia is the abnormal placentation that characterized by defective trophoblast cell invasion and uterine vasculature remodeling [36]. During normal pregnancy, maternal uterine spiral arteries are remodeled into low-resistance vessels as a result of fetal trophoblast invasion and replacing the endothelial and smooth muscle cells in the vessel wall [37]. The interaction between the trophoblast and uterine natural killer cells initials the spiral artery remodeling [38]. In preeclampsia, overreaction of the maternal immunity can limit the placental development [39], while the incomplete trophoblastic invasion and spiral arteries remodeling lead to decreased placental perfusion and poor placentation [40,41,42], which result in the activation of pathways leading to maternal vasoconstriction and endothelial dysfunction [42]. Currently, the exact pathological mechanisms of incomplete trophoblastic invasion are not completely known while some studies have suggested, apart from immune maladaptation, the contribution of imbalanced angiogenic growth factors and placental endothelial dysfunction [40, 43].
Reduction of placental angiogenic factors plays an important role in the pathogenesis of preeclampsia. The releases of angiogenic cytokines including, vascular endothelial growth factor (VEGF), placental growth factor (PlGF), and angiopoietin 2, are required for normal placentation [40, 43, 44]. In the first trimester of pregnancy, low serum level of PlGF is detected in suspected preeclampsia [45]. Inflammation and tissue hypoxia in the spiral arteries lead to the production of the transcription factor hypoxia-inducible factor-1 (HIF-1), which in turn downregulates PlGF [46]. Also, soluble fms-like tyrosine kinase 1 (sFlt1), an antiangiogenic protein that inactivates VEGF and PlGF is upregulated in preeclampsia [47]. Therefore, placental abnormality results in decreased levels of angiogenic VEGF and PlGF and increased levels of deleterious placental factors including sFIt-1 in the maternal circulation. Moreover, the imbalance of pro- and anti-inflammatory and pro- and anti-angiogenic factors significantly contribute to generalized endothelial dysfunction, intravascular inflammation, and activation of the hemostatic system that result in the maternal syndrome [48, 49].
Throughout the whole body, the endothelium is believed to be the primary target of mediators generated from the placenta, causing endothelial dysfunction and end-organ damages [50]. Hypertension and proteinuria are common manifestation of endothelial dysfunction-mediated end-organ damages, while some severe cases of preeclampsia have microangiopathic hemolytic anemia and organ hypoperfusion [51]. Indeed, endothelial dysfunction can occur in both maternal and placental circulations in hypertension disorders of pregnancy [40,41,42]. In clinical studies, vascular responsiveness can be assessed by in vivo [52,53,54,55] and in vitro [56, 57] methods to examine the vascular function in normal pregnancy and preeclampsia. A clinical study has demonstrated that vascular reactivity to endothelium-dependent vasodilators (such as acetylcholine) was impaired in preeclampsia as evidenced by the reduced forearm blood flow measured by venous occlusion plethysmography in vivo [52]. Flow-mediated dilatation was reduced in preeclampsia patients compared to normal pregnant women as measured by myography in vitro [56]. In addition, a reduction of flow-mediated dilation was observed in the uterine artery or preeclampsia patients by doppler ultrasonography in vivo [54]. Also, preeclampsia is associated with a failure of shear stress-induced vasodilatation and an enhanced myogenic response in vitro, which increased the vascular resistance in the uterine circulation [57]. Serum levels of endothelial activation markers including thrombomodulin, von Willebrand factor, fibronectin, and cell adhesion molecules including intercellular adhesion molecule 1 (ICAM-1), and vascular adhesion molecule (VCAM-1) have been shown upregulated in preeclamptic patients [58,59,60]. Coherent with the clinical studies, treatment of recombinant sFlt-1 in human umbilical vascular endothelial cells (HUVEC) significantly increases these endothelial activation markers in vitro [61], suggesting the pathological role of sFlt-1 in endothelial activation, which in turn, contributes to the adverse responsiveness of the vasculature. During preeclampsia, patients have increased serum levels of vasoconstrictors such as endothelin 1 (ET-1) and thromboxane [62,63,64], while the responsiveness to vasodilators including nitric oxide (NO) and prostacyclin is significantly reduced in vivo [65,66,67]. Endothelium-dependent hyperpolarization factors (EDHF)-mediated relaxation is also reduced in arteries of women with preeclampsia [68]. Vessels isolated from preeclamptic patients have increased responsiveness to vasoconstrictors including potassium chloride (KCl) and arginine vasopressin (AVP) and have limited vasodilatation in response to acetylcholine in vitro [69]. Studies using animal models of preeclampsia have reported comparable findings [70]. Moreover, vascular dysfunction in preeclampsia can be manifested as augmented arterial stiffness and remodeling [71].
Although there may be multiple factors that contribute to endothelial dysfunction in preeclampsia, poor placentation and ischemic placenta, associated with acute atherosis or thrombosis, are considered critically contribute to endothelial dysfunction [72]. Recent reports have suggested that maternal factors including obesity, hyperlipidemia, insulin resistance, and inflammation-associated coagulation factors alteration are correlated to impaired placentation [43, 73, 74]. These conditions further augment oxidative stress and disrupt both maternal and perinatal endothelial functions that lead to organ hypoperfusion [43]. Strikingly, incubation of resistance vessels from normotensive pregnant women with plasma from either preeclampsia patients or pregnant women who would later develop preeclampsia also results in a reduction of endothelium-dependent relaxation ex vivo, which highlights the contribution of the imbalanced circulating factors in the development of endothelial dysfunction during preeclampsia [75, 76]. These mechanisms lead to endothelial dysfunction that eventually results in hypertension and increased cardiac output, stroke volume, and systemic vascular resistance during preeclampsia, as well as in postpartum, and increase the risk for cardiovascular disease later in life [77, 78]. In addition, growing evidence has linked these placental vascular pathologies with poor fetal growth and adverse birth outcomes [79,80,81].
In addition to endothelial dysfunction, premature aging of the placenta has recently been associated with hypertensive disorders of pregnancy and intrauterine growth restriction (IUGR) [82]. Patients with preeclampsia have augmented placental senescence compared to normal pregnant women as evidenced by telomere shortening in trophoblasts [82], while other studies have shown the upregulation of protein and gene expression of senescence-associated secretory phenotype (SASP) components including p16, p21, p53, IL-6, IL-8, plasminogen activator inhibitor-1 (PAI-1), and monocyte chemotactic protein-1 (MCP-1) in the placenta from preeclamptic patients compared to normotensive controls [83,84,85,86]. One study has demonstrated that senescence of mesenchymal stem cells, multipotent cells with pro-angiogenic activities, is one of the mechanisms by which angiogenesis is inhibited by systemic inflammation in preeclampsia [87]. The same group has recently revealed the aging phenotype in the adipose tissue and kidney during preeclampsia, suggesting that cellular senescence can be one of the important mechanisms of the pathophysiology of preeclampsia [88]. In addition, immunohistological staining of the preeclamptic placentas revealed the presence of 8-hydroxy-2′-deoxy-guanosine (8-OHdG) [83], suggesting that oxidative stress may cause DNA damage, resulting in the activation of tumor suppressor genes such as p53. In fact, chronic low-grade inflammation can increase placental oxidative stress and endoplasmic reticulum stress in the placenta [89]. Poor placentation is also associated with increased placental oxidative stress and endoplasmic reticulum stress, which can facilitate the pathways of senescence [89]. These lead to apoptosis and cell senescence which result in the loss of proliferative capacity in the placenta (Fig. 2).
Placental dysfunction in hypertensive disorders of pregnancy. The current understanding of the pathogenesis of placental dysfunction in hypertensive disorders of pregnancy. Placenta plays an important role in the development and severity of preeclampsia. It is proposed that the initiating step in the pathogenesis of preeclampsia is the abnormal placentation that characterized by defective trophoblast cell invasion and uterine vasculature remodeling. Placental dysfunction leads to further imbalance in angiogenic factors, increased placental oxidative stress, placental aging and increased endothelial activation markers in the pathogenesis of preeclampsia. These multiple factors can cause adverse effects in both mother and offspring. Endothelial dysfunction leads to end-organ damages in the mother and causes symptoms of preeclampsia. Placental insufficiency can lead to growth restriction and adverse birth outcomes in the offspring. Preeclampsia can also increase the risk of metabolic and cardiovascular diseases in the mother as well as in the later life of the offspring.
Fetal programming and reprogramming
The sensitivity and susceptibility of the epigenome are high during pregnancy and lactation periods and decrease during life [90]. It is suggested that some adult metabolic and cardiovascular diseases have a fetal origin, which is also referred as fetal programming [91, 92]. Apart from maternal end-organ damages, preeclampsia can leave short-term and long-term adverse effects on the offspring. Indeed, the risk of preeclampsia is increased with family history while a maternal history of preeclampsia increases the risk in her daughter, as well as her son’s female partner [93]. Various reports have suggested the hypothesis that nutrition condition during intrauterine life and perinatal period may have long-lasting effects on the future risk of metabolic and cardiovascular disease through persistence of metabolic and physiological adaptations, which is referred as fetal reprogramming [94,95,96,97]. Epigenetic modifications can be induced by diet and drug treatments during pregnancy and lactation periods, even with compounds that are not direct inhibitors or activators of the epigenetic machinery enzymes [98, 99]. These suggest that maternal drug treatment and/or dietary supplementation may be very likely to affect the birth outcome and modulate the future risk of metabolic and cardiovascular diseases in the later life of the offspring by epigenetic mechanisms.
Endothelial nitric oxide synthase, nitric oxide, and preeclampsia
Endothelial nitric oxide synthase (eNOS) is an important regulator of vascular tone and contributes to the reduction of the uteroplacental resistance during normal pregnancy [100, 101]. eNOS exerts its functions mainly via the production of NO by reduction of L-arginine to L-citrulline [101]. It is suggested that, among different mediators that involved in endothelial dysfunction in preeclampsia, the role of eNOS appears most significant in the development of preeclampsia [102]. NO synthesis can be stimulated by intraluminal flow, shear stress, and vasodilators such as acetylcholine and bradykinin [56, 57]. It has been shown that NO production from the endothelium is increased during normal pregnancy and decreases in preeclampsia [103]. Also, various clinical studies have revealed the association between certain eNOS gene variants (for example G894T, 4b/a, c.894G > T (p.(Glu298Asp)), g.-786 T > C, g.2051G > A, and g.1861G > A) and low serum level of NO in preeclamptic patients [104, 105], while the presence of AGT 704C allele is associated with a reduced risk of developing preeclampsia [105]. Reduced eNOS activity or NO production exacerbates sFlt-1-associated preeclampsia-like phenotype in mice, which is partly through activation of the endothelin system [106].
Indeed, preeclampsia occurs during pregnancy exclusively in humans and certain apes, therefore, researches have been limited since there is currently no animal model which exactly mimics human preeclampsia [107]. Rodents are the most commonly used models for investigating preeclampsia, due to the similarity of cardiovascular adaptations to pregnancy in humans. In general, these rodent models of preeclampsia exhibit an increase in blood pressure (approximately 20–30 mmHg rise in systolic blood pressure), accompanied by reduced renal function [107,108,109]. NOS inhibition by its nonselective inhibitor L-NG-Nitro arginine methyl ester (L-NAME) has been commonly used in rodent models to mimic preeclampsia-like phenotype [110]. Chronic L-NAME treatment in pregnant rat results in hypertension, reduced kidney function and increased placental sFLT-1 expression, while proteinuria is not observed and vascular function is not altered ex vivo [111]. Also, fetal malformations could be a side-effect of L-NAME treatment [112]. sFLT1-infusion in rats is another animal model with preeclampsia-like symptoms and is the only animal model reported to have glomerular endotheliosis [113]. However, the relevance of this animal model requires more detailed studies. The main concern of these treatment-induced model is that the symptoms would be unlikely to subside after delivery of the placenta and is not due to a pregnancy-derived phenotype. On the other hand, Dahl salt-sensitive rats (DSSR) is a genetic model of salt-induced hypertension and has been recently reported to display preeclamptic phenotype (including blood pressure, proteinuria, placental hypoxia and reduced uteroplacental blood flow and fetal growth restriction) even when fed a normal chow diet [114,115,116,117,118]. There are a few helpful reviews that provide detailed discussion on animal models of preeclampsia [107,108,109, 119].
During normal pregnancy, the production of reactive oxygen species (ROS), such as NO, hydrogen peroxide (H2O2), hydroxyl radical·OH, superoxide anion O2−, and peroxynitrite ONOO− is increased [120]. These physiological ROS are important for the development of placenta and promotion of mitochondrial activity in trophoblasts [121]. In addition, uterine contractions and interventions including diet and exercise may induce mild placental ROS production that is also needed for maintenance of pregnancy and embryo development [120]. It is suggested that eNOS/NO signaling plays an important role in maintaining a healthy pregnancy. However, when ROS production is augmented, eNOS becomes uncoupled [122]. It is also suggested that the uncoupling of eNOS in the hypoxic placenta may further trigger high oxidative stress during preeclampsia [100]. Oxidative stress in the placenta can stimulate the release of apoptotic and necrotic trophoblastic placental debris, anti-angiogenic factors, and proinflammatory cytokines into maternal circulation [123].
On the other hand, sFlt-1 secreted from the placenta can antagonize VEGF signaling, which leads to reduced eNOS activity [61]. Hypertensive disorders of pregnancy are associated with increased levels of factors that inhibit eNOS/NO pathway. Plasma level of asymmetric dimethyl arginine (ADMA), a competitive inhibitor of eNOS, is increased in preeclamptic patients [54], while the expression of a placenta-derived soluble transforming growth factor beta (TGF-β) coreceptor, endoglin, which impairs eNOS activation is also increased [124]. Recent report has also shown that microRNAs (miRs) are upregulated in the human placenta during preeclampsia [125]. These miRs are carried by exosomes and can suppress NO production and eNOS expression by targeting the 3’-untranslated region on eNOS [125].
NO donors have potent vasodilator effect and have been shown to improve blood flow in the fetoplacental circulation during mild preeclampsia [126]. The vasodilator effect of NO signaling is modulated by the interaction between NO and heme-containing proteins, most notably soluble guanylyl cyclase (sGC) [127]. In addition, NO is an endogenous signaling molecule that is involved in the regulation of various important cellular functions. NO can regulate gene expression by either direct interaction with transcription factors or by post-translational modifications of proteins [128]. Recent studies have also revealed the importance of eNOS/NO signaling in modulating the expression of angiogenic factors including PlGF, VEGF, angiopoietins and their receptor soluble angiopoietin-tunica interna endothelial cell kinase 2 (Tie-2), thrombospondin, and anti-angiogenic factors such as sFlt-1 [129, 130]. NO is involved in the transcriptional regulation of histone-modifying enzymes and modulates the activities and cellular localizations of transcription factors through the formation of S-nitrosothiols or iron nitrosyl complexes. [131]. In addition, NO may alter the cellular methylation, acetylation, phosphorylation, ubiquitylation, or sumoylation profiles of proteins and histones [132]. S-nitrosylation is a post-translational modification on the cysteine residue by NO [133]. S-nitrosylated proteins are reported to be involved in different pregnancy-related processes including trophoblast cell migration, immunomodulation, apoptosis, and oxygen delivery [134]. Growing evidence has revealed the association between abnormal placental S-nitrosylation and preeclampsia in both human [135] and rodent [136]. The nitroso-proteomes in the placentas from normotensive and preeclamptic patients are significantly different, while among these downregulated S-nitrosylated-proteins in preeclampsia, annexin A2 is responsible for the activation of angiogenesis [137]. Therefore, reduced eNOS/NO signaling in hypertensive disorders of pregnancy may alter the nitrosylation of proteins which lead to placental dysfunction.
Dietary supplement
Due to the complex etiology of preeclampsia and safety concerns on drug usage during pregnancy, there is still no effective pharmacological treatments available for preeclampsia yet [3]. An emerging area of interest in this research field is the potential beneficial effects of dietary intervention on reducing the risk of preeclampsia [138]. Recent studies have been focused on the association between deficiencies or excesses of some nutrients and complications during pregnancy, fetal growth and development, and later risk of cardiovascular and metabolic diseases in the offspring.
During pregnancy, nutrient intake during the periods of periconception and pregnancy has significant influences to both the health of mother and the development of the fetus [139]. Pregnancy greatly changes a woman’s metabolism and increases the demands for energy, proteins, vitamins, and minerals. The daily requirement of dietary intake in healthy pregnancy woman is higher than that of a healthy nonpregnant woman [140]. The growth and development of fetus depend completely on the mother; hence, adequate maternal dietary intake is essential for the health of the mother and the development of the fetus. In this sense, pregnancy represents a challenge from a nutritional perspective [141, 142]. Unbalanced diet is a well-known risk factor for cardiovascular diseases and diabetes; hence it may also play a role in the pathophysiology of hypertensive disorders of pregnancy [143]. In addition, imbalanced serum levels of nutrients have been associated with increased inflammation, oxidative stress, and dyslipidemia [144]. Nutrient status including increased serum triglyceride and fatty acids, and reduced levels of magnesium, zinc and vitamins, as well as low calcium intake have been associated with increased risk of pre-eclampsia [145, 146].
An ideal nutrient supplement and/or therapy for pregnancy-related complications should have protective effects in relieving the symptoms of preeclampsia in the mother, improving fetal growth and survival, as well as reducing the disease risk of the offspring at adult ages. Although, the exact effects and mechanisms of nutrition in the alleviating preeclampsia are still debatable, growing number of studies has provided supporting evidence for the potential use of supplements in alleviating preeclampsia. Currently, two main mechanisms have been proposed: (i) Nutritional supplementation shows pharmacological effects in women with dietary intake of nutrients above the recommended daily amount [147]; (ii) nutritional supplementation may achieve benefit via normalizing the deficiency in women with inadequate nutrition [148]. Here, we summarize some of the supplements and their documented beneficial effects in hypertensive disorders of pregnancy.
L-arginine
As mentioned above, NO is a potent endothelium-derived vasodilator and defective eNOS/NO signaling has been documented in preeclampsia. NO is produced by eNOS which uses L-arginine as substrate. Therefore, the bio-availability of L-arginine is important to maintain the endothelial adaptive regulatory mechanisms for vasodilatation in healthy pregnancy. Arginine is a semi-essential amino acid and the precursor of various biological pathways including the urea cycle and the production of NO and polyamines [149, 150]. Arginine may regulate many metabolic pathways that are crucial to reproduction, growth, and health [151], while the role and functions of NO have been discussed above. It is well documented that the administration of L-arginine improves vascular function in atherosclerosis and peripheral vascular diseases [152,153,154].
Recently, it has been shown in some animal and clinical studies that L-arginine have the potential to alleviate preeclampsia [155,156,157]. In a recent systematic review and meta-analysis of randomized controlled trials, L-arginine supplementation has been shown to increase plasma NO concentration in IUGR pregnancies and decrease the risk of preeclampsia [158]. In addition, L-arginine supplementation can improve birth weights of offspring in both hypertensive and IUGR pregnant women [158]. Moreover, it has been suggested that intravenous infusion of L-arginine, but not oral administration, significantly increases NO concentrations and birth weights in IUGR pregnancies [158]. L-arginine has also been shown to alleviate the pathogenesis of malaria-induced adverse birth outcomes in pregnancy [159, 160].
Apart from NO, several metabolites of arginine, such as polyamines, are important nutrients required in multiple stages of pregnancy, including implantation, early embryogenesis, fetal growth, and placental development [161]. Polyamines, such as putrescine, spermine, and spermidine, will interact with negatively charged molecules, including DNA, RNA, acidic proteins, and phospholipids [162, 163]. Indeed, polyamine metabolism plays an important role in placental function during pregnancy [164]. Reductions in polyamine bioavailability in pregnant rodent models have been associated with abnormal placentation and fetal growth restriction [165, 166]. Polyamines are involved in the regulation of the inflammatory response due to their antioxidant properties [167] and modulate T cell responses [168]. Treatment with spermine inhibits lipopolysaccharide (LPS)-mediated production of pro-inflammatory cytokines, such as TNF-α and IL-6 in mouse macrophages [169]. The beneficial effects of polyamines may be attributed to the regulation of pathways involved in endothelial cell migration, proliferation, protein synthesis, and pro-angiogenic gene expression [164]. However, the underlying molecular pathways by which polyamines are involved in angiogenesis remain unclear. Recent study also reveals the epigenetic effects of placental polyamines via regulating acetyl-CoA level and histone acetylation [161].
These observations raise the possibility of practical dietary L-arginine supplementation during pregnancy as a NO donor to reduce the risk of preeclampsia. Nevertheless, although L-arginine is an inexpensive supplementation with a known safety profile in pregnancy, the bioavailability of arginine is relatively low, as 40% of oral arginine is catabolized by the intestine and another 9% is metabolized by the liver [159]. Therefore, the challenge of considering L-arginine as a dietary supplement targeting preeclampsia would be the low bioavailability.
L-citrulline
L-citrulline is an amino acid that is also the natural precursor and metabolite of L-arginine. L-citrulline is converted to L-arginine by arginosuccinate synthase. Activation of arginosuccinate synthase in cells isolated from preeclamptic patients has been shown to improve endothelial function, associated with increased NO production and reduced oxidative stress [170, 171]. On the other hand, compared to arginine, citrulline has been shown more effective to promote NO production as it can bypass hepatic metabolism, and not metabolized by arginase [159]. A few evidence has suggested that the protective effect of citrulline may not be analogous with arginine [172], and these two amino acids regulate gene expression in different manners [173]. Citrulline has also been shown to improve protein anabolism, increase nitrogen balance in rats [174], and enhance muscle protein synthesis in human [175] more efficiently than arginine. In addition, the usage of citrulline has an even greater safety profile than that of arginine, as none of the clinical trials have reported any adverse effects [176]. Therefore, these raise the hypothesis that citrulline can be a better supplementation than arginine in targeting hypertensive disorders of pregnancy.
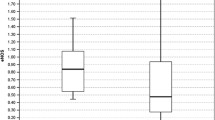
In our recently published study, we examined the effect of citrulline supplementation in a rat model of preeclampsia [177]. We have demonstrated the protective effects of citrulline supplementation in the Dahl salt-sensitive rats (DSSR). Citrulline supplementation in DSSR leads to the reduction of maternal blood pressure and markers of preeclampsia (sFlt-1). Pup-to-placenta weight ratio and maternal vascular function are improved by citrulline supplementation. In addition, the beneficial effects of citrulline in ameliorating placental fibrosis and senescence, and promoting angiogenesis in the placentas have been observed, in parts, attributable to the downregulation of toll-like receptor 4 (TLR4) and nuclear factor κB (NF-κB) in the placenta [177]. Coherently, another study has demonstrated the effect of L-citrulline supplementation in a mouse model of preeclampsia [178]. This study shows that L-citrulline supplementation can reduce blood pressure, increase vascular glycocalyx volume, and improve maternal vascular function ex vivo at gestation day 17.5 in the preeclampsia-like mouse model [178]. The beneficial effects of citrulline in maternal vascular function appear, in part, attributable to eNOS/NO signaling. In addition, L-citrulline supplementation has also been shown to enhance fetal growth and protein synthesis in rats with intrauterine growth restriction [179]. Maternal L-citrulline supplementation can prevent 50% caloric restriction-induced low nephron number and renal dysfunction in the offspring, although increased blood pressure has been observed in the offspring [180]. The effects in developmental programming of kidney disease and hypertension are associated with reduced ADMA in the plasma [180]. Also, maternal supplementation with citrulline has been shown to have long-term antihypertensive effects in the offspring of spontaneous hypertensive rats [181]. Moreover, maternal L-citrulline treatment prevents prenatal dexamethasone-induced programmed hypertension by restoration ADMA/NO balance, alterations of renin–angiotensin system and sodium transporters, and epigenetic regulation by histone deacetylases in mice [182].
Micronutrients
Micronutrients, including fatty acids, vitamins, and minerals, are chemical substances that are required in small amount but are important in regulating the metabolic and biochemical processes of the body [183]. Deficits in any of them can lead to deficiencies in growth and development, as well as abnormal physiological functions, and immunity. Current evidence supports the idea that deficiencies of these micronutrients have adverse effects in maternal health and the outcome of pregnancy.
Fatty acids
Lipid and fatty acids are involved in the generations of free radicals [184]. High-fat diet is atherogenic, while polyunsaturated fats are substrate for lipid peroxidation and have been reported to be increased in the diet of preeclamptic women [185]. On the other hand, omega-3 long-chain polyunsaturated fatty acids (n-3 PUFAs) have been suggested to be involved in the prevention of preeclampsia. Studies have revealed that levels of n-3 PUFAs were lower in erythrocytes of women with preeclampsia [186]. n-3 PUFAs are essential for fetal tissue formation [187]. In addition, n-3 PUFAs have been shown to have protective effects in cardiovascular function and alleviating inflammation [188, 189]. Eicosapentaenoic acid (EPA, 20:5), and docosahexaenoic acid (DHA, 22:6) have been associated with beneficial effects in vasodilation [190]. In addition, n-3 PUFAs have been shown to increase eNOS activity and NO production [191, 192]. The beneficial effects of n-3 PUFAs are suggested by the evidence that there is a reduced rate of preeclampsia in population that have large quantities of fish or fish oil intake [193]. In a recent systematic review and meta-analysis, the comparison of clinical trials has also suggested that n-3 PUFAs supplementation played a protective role against the risk of preeclampsia in women with low-risk pregnancies [194], probably by reducing placental inflammation and oxidative stress [195]. In a recent umbrella review of meta-analyses of randomized trials, n-3 PUFAs supplementation during pregnancy can exert beneficial effects in improving birth weight, preterm delivery, and post-partum depression, and reducing cardiometabolic risk factors in pregnant mothers, as well as can improve anthropometric measures, immune system, and visual activity in infants [196]. It has also been recently reported the effect of maternal intake of n-3 PUFAs during pregnancy influences the offspring DNA methylation [197]. Also, it has been recently shown that maternal n-3 PUFAs supplementations are closely correlated to infant telomere length [198]. However, the long-term effect of maternal intake of n-3 PUFAs in reducing future risk of metabolic and cardiovascular diseases in the offspring is unknown.
Calcium
Calcium supplementation has been reported to reduce the risk of preeclampsia [199]. Indeed, calcium is the most-studied micronutrient in relationship to preeclampsia. Various epidemiological studies have demonstrated the association between reduced calcium intake and preeclampsia [200, 201] and women with low calcium intake (< 800 mg/day) are considered at increased risk of preeclampsia [21]. Several randomized controlled trials have been performed to investigate the effect of calcium supplementation. The analysis of these trails has indicated a 32% reduction of the incidence of preeclampsia with calcium supplementation [199], while this beneficial effect is most prominent in low baseline calcium intake groups. However, one of the largest trials to date reported no effect of calcium supplementation on preeclampsia [202], probably due to the inclusion of pregnant women with adequate dietary calcium intake. Therefore, current evidence has supported the hypothesis that the incidence of preeclampsia can be reduced by calcium supplementation, while women with low calcium intake seem to be more likely to benefit from calcium supplementation [203]. In addition, prenatal supplementation with high-dose calcium has been shown to reduce the prevalence of gestational hypertension, serious maternal morbidity or death, and preterm birth [199]. Moreover, maternal calcium supplementation has been shown to improve the postpartum maternal bone health [204, 205], as well as to reduce the risk of increased systolic pressure in the offspring [206].
Vitamins
A recent systematic review and meta-analysis have shown the positive correlation between lower rate of preeclampsia and calcium and vitamin D intake [207]. Vitamin D is a pre-hormone, that can also be endogenously produced by the skin when exposed to UV-B. Vitamin D plays an important role in preventing bone diseases and improving calcium metabolism [208]. Recently, vitamin D has also been shown to regulate the expression of signature developmental and angiogenic genes in the placenta [209,210,211]. Vitamin D deficiency before 22 weeks of pregnancy is a strong and independent risk factor for preeclampsia [208]. Maternal vitamin D insufficiency could also lead to preterm birth, small for gestational age or IUGR and gestational diabetes mellitus [212]. The active vitamin D metabolite, 1,25-dihydroxyvitamin D3 [1,25-(OH)2D3], exerts immunosuppressive activity. It has anti-proliferative effect on Th1 cells and inhibits the secretion Th1 cytokines [213]. Deficiency of vitamin D is significantly associated with placenta calcification and aging [214]. Various studies have provided evidence supporting that vitamin D supplementation can reduce the incidences of preeclampsia [215,216,217]. Some recent studies have shown that vitamin D supplementation can improve mitochondrial function, reduce inflammation in the placenta and preserve placental functions [218, 219]. A few trails have shown that vitamin D supplementation can reduce the risk of having a preterm birth [220, 221], as well as improve fetal growth and peripheral blood flow in the fetus [222]. One study has shown that low vitamin D status is associated with lower adiposity at birth, but a greater offspring adiposity at age of 6 years [223]. However, the long-term effect of maternal vitamin D supplementation in the offspring is still unclear.
Vitamins C and E are important non-enzymes that involve in the endogenous cellular antioxidant system. Vitamin C is water soluble while vitamin E is lipid soluble [224]. Vitamin C level is decreased in women with preeclampsia [225, 226] while vitamin E has been shown to be reduced in some [225, 226] but not all cases [227, 228]. Vitamin E is consistently reduced in severe cases of preeclampsia [229, 230]. Adequate dietary intake of vitamins C and E appears to be mandatory to prevent oxidative stress [231]. Indeed, antioxidants have been proposed as prophylactic agents for preeclampsia [232, 233]. Various studies have demonstrated the beneficial effect of vitamin C and E supplementation in reducing preeclampsia by 4–12% depending on the risk level of the pregnant woman [234, 235]. Vitamin C or E supplementation can reduce the systolic blood pressure in the preeclampsia patient [235]. Supplementation with vitamins C and E can has been shown to reduce PAI-1/PAI-2 ratio during gestation [233], suggesting the beneficial effects of vitamins C and E may be attributed to alleviating endothelial senescence and placental insufficiency. Vitamin C administration improves endothelial function, as evidenced by the increased flow-mediated dilatation measured by in vivo ultrasonography, in previously preeclamptic women [55]. However, some of the studies did not observe any significant effects of vitamins C and E [147, 236]. Nevertheless, a recent meta-analysis has indicated that multivitamins supplementation can significantly reduce the risk of preeclampsia [237], suggesting that the beneficial effects of vitamins may be interrelated.
Resveratrol
Resveratrol (3,5,4′-trihydroxy-trans-stilbene) is a polyphenol found in grape fruits and can be obtained from drinking red wine [238]. Resveratrol has been widely studied on its anti-oxidant and anti-inflammatory activities [239,240,241]. The protective effects of resveratrol have been demonstrated in cancer, cardiovascular, metabolic, and neurodegenerative diseases [242,243,244]. Resveratrol exerts its beneficial effect in cardiovascular protection by increasing the production of NO, partly by, upregulating eNOS expression, stimulating eNOS activity, and preventing eNOS uncoupling [245]. Also, resveratrol can modulate the function of immune cell and inhibit immune cell infiltration [246, 247].
Resveratrol supplementation improves the efficacy of oral nifedipine treatment in preeclampsia [248]. Maternal resveratrol consumption could decrease inflammation and oxidative stress in placental and embryonic tissues [249]. Also, resveratrol treatment has been shown to increase uterine artery blood flow and fetal oxygenation, upregulate antioxidant enzymes in the placenta, reduce markers of endothelial dysfunction, and enhance placental and fetal weight in a rat model of severe hypoxia [250]. The expressions of endothelial dysfunction markers, including ICAM-1, von Willebrand factor, and Caspase-3, in endothelial cells and umbilical arteries from preeclampsia patients are coherently attenuated by resveratrol treatment [251]. A recent study has revealed that resveratrol ameliorates preeclampsia by upregulating VEGF through miR-363-3p-mediated pigment epithelium-derived factor (PEDF) downregulation [252]. Moreover, a systematic review of 31 studies has suggested that resveratrol possesses epigenetic effects in the development of placenta and fetal tissues during the gestational period [253]. Various animal studies have demonstrated the fetal reprogramming effects of maternal resveratrol supplementation that attenuate obesity, prevent hepatic steatosis, and improve insulin sensitivity and islet dysfunction in the offspring [254, 255].
Recently, the effects of sirtuin 1 (SIRT1) on the biological functions of trophoblasts and endothelial cells have gradually emerged, and the serum and placental level of SIRT1 is reduced in preeclampsia [256,257,258]. SIRT1, which can be activated directly or indirectly by resveratrol, is also known as a longevity enzyme. SIRT1 activity is controlled by intercellular nicotinamide adenosine dinucleotide (NAD) levels and is involved in transcriptional regulation of a large number of genes that are involved in different cellular functions [238]. SIRT1 can also activate eNOS and enhance endothelial function [238] and is an important player in regulating vascular function and preventing vascular aging [259]. The beneficial effects of resveratrol in cardiovascular diseases are comparable to calorie restriction or SIRT1-overexpression models in vivo [260, 261]. A recent study has demonstrated that treatment of recombinant SIRT1 protein can decrease maternal blood pressure and improves angiogenic imbalance, inflammation, and pregnancy outcome in a rat model of preeclampsia [257]. High levels of sFlt-1, TNF-α, and IL-6 in maternal plasma are normalized by the treatment of recombinant SIRT1 protein [257]. In another recent study, downregulation of SIRT1 has been correlated to the accelerated senescence of syncytiotrophoblast via downstream targets contributing to the regulation of the cell cycle, extracellular matrix production, and cytoskeleton reorganization, which lead to premature placental aging in preeclampsia [258]. Resveratrol-induced SIRT1 activation abrogates senescence in trophoblast-derived BeWo cells in vitro [258], suggesting the beneficial effect of resveratrol in ameliorating placental senescence in preeclampsia. In addition, resveratrol has also been studied for the beneficial effect on modulating gut microbiota [98, 245, 262]. Recent studies have discussed the causal association between gut dysbiosis and preeclampsia [263,264,265]. These raise the possibility that beneficial effect of resveratrol in alleviating preeclampsia is partly via gut microbiota remodeling.
Conclusion and future directions
Pregnancy-associated hypertensive disorders represent an important cause of maternal and infant mortality and morbidity, as well as increasing the risk for future metabolic and cardiovascular disease for both mother and offspring. Although the knowledge of pregnancy-associated hypertensive disorders has increased dramatically over the past years, the role of diet and the potential use of dietary supplements or therapy targeting preeclampsia has not been adequately studied. Currently, different clinical trials and meta-analyses have been performed to evaluate the effect of different dietary supplements on the development of preeclampsia (Table 1). However, these studies are mostly limited by the fact that the pathogenesis of preeclampsia could be multifactorial, severity of preeclampsia can be varying and heterogeneity between studies is very high. In addition, in most clinical cases of preeclampsia, it is not possible to discriminate the cause and effect between nutrient deficiencies and preeclampsia. Therefore, there is a need to apply novel animal models of preeclampsia for future studies in this field. To improve study quality, we must also try to explore the effects of these interventions and/or therapeutics in three important aspects: the maternal syndrome, fetal growth and survival, and the disease risk of the offspring at adult ages. Nevertheless, this review has summarized the current understanding of the pathophysiology of pregnancy-associated hypertensive disorders in a vascular perspective. We have also listed out the beneficial effects of a few dietary supplements targeting preeclampsia. This review aims to provide some potential insight and brainstorming for the future direction of studies with dietary interventions in preventing preeclampsia.
Data Availability
Not applicable.
References
World Health Organization. Fact sheet - maternal mortality. Available at: https://www.who.int/news-room/factsheets/detail/maternalmortality#:~:text=A%20woman's%20lifetime%20risk%20of,49%20in%20low%2Dincome%20countries
Say L et al (2014) Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health 2(6):e323–e333
Brown MA et al (2018) Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 72(1):24–43
Cunningham FG et al (2014) Williams obstetrics, 24e. Mcgraw-Hill New York, NY USA
Mol BWJ et al (2016) Pre-eclampsia. Lancet 387(10022):999–1011
Rich-Edwards JW et al (2014) Pregnancy characteristics and women’s future cardiovascular health: an underused opportunity to improve women’s health? Epidemiol Rev 36(1):57–70
Feig DS et al (2013) Preeclampsia as a risk factor for diabetes: a population-based cohort study. PLoS Med 10(4):e1001425
Irgens HU et al (2001) Long term mortality of mothers and fathers after pre-eclampsia: population based cohort study. BMJ 323(7323):1213–1217
Ray JG et al (2005) Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 366(9499):1797–1803
Gilbert JS et al (2008) Pathophysiology of hypertension during preeclampsia: linking placental ischemia with endothelial dysfunction. Am J Physiol Heart Circ Physiol 294(2):H541–H550
Englund-Ogge L et al (2014) Maternal dietary patterns and preterm delivery: results from large prospective cohort study. Bmj 348:g1446
Brantsaeter AL et al (2009) A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr 139(6):1162–1168
Kibret KT et al (2018) Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: a systematic review and meta-analysis. Public Health Nutr 22:1–15
Villar J et al (2006) Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol 194(4):921–931
Buchbinder A et al (2002) Adverse perinatal outcomes are significantly higher in severe gestational hypertension than in mild preeclampsia. Am J Obstet Gynecol 186(1):66–71
Strevens H et al (2003) Glomerular endotheliosis in normal pregnancy and pre-eclampsia. BJOG 110(9):831–836
Butalia S et al (2018) Hypertension Canada’s 2018 guidelines for the management of hypertension in pregnancy. Can J Cardiol 34(5):526–531
Magee LA et al (2014) Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can 36(7):575–576
Lowe SA et al (2015) The SOMANZ guidelines for the management of hypertensive disorders of pregnancy 2014. Aust N Z J Obstet Gynaecol 55(1):11–16
American College of Obstetricians and Gynecologists (2013) Task force on hypertension in pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol 122(5):1122–1131
Poon LC et al (2019) The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: a pragmatic guide for first-trimester screening and prevention. Int J Gynaecol Obstet 145:1–33
Leeman L, Dresang LT, Fontaine P (2016) Hypertensive disorders of pregnancy. Am Fam Physician 93(2):121–127
Mattar F, Sibai BM, Eclampsia VIII (2000) Risk factors for maternal morbidity. Am J Obstet Gynecol 182(2):307–312
Sibai BM (2005) Diagnosis, prevention, and management of eclampsia. Obstet Gynecol 105(2):402–410
Redman EK et al (2019) Clinical course, associated factors, and blood pressure profile of delayed-onset postpartum preeclampsia. Obstet Gynecol 134(5):995–1001
Patten IS et al (2012) Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature 485(7398):333–338
Newstead J, von Dadelszen P, Magee LA (2007) Preeclampsia and future cardiovascular risk. Expert Rev Cardiovasc Ther 5(2):283–294
Paauw ND et al (2016) Long-term renal and cardiovascular risk after preeclampsia: towards screening and prevention. Clin Sci (Lond) 130(4):239–246
Duley L (2009) The global impact of pre-eclampsia and eclampsia. Semin Perinatol 33(3):130–137
Aykas F et al (2015) Persistence of cardiovascular risk factors in women with previous preeclampsia: a long-term follow-up study. J Investig Med 63(4):641–645
Acosta-Sison H (1956) The relationship of hydatidiform mole to pre-eclampsia and eclampsia; a study of 85 cases. Am J Obstet Gynecol 71(6):1279–1282
Jauniaux E (1999) Partial moles: from postnatal to prenatal diagnosis. Placenta 20(5-6):379–388
Staff A.C (2019) The two-stage placental model of preeclampsia: an update. J Reprod Immunol 134-135:1–10
Mayne BT et al (2017) Accelerated placental aging in early onset preeclampsia pregnancies identified by DNA methylation. Epigenomics 9(3):279–289
Wu G et al (2004) Maternal nutrition and fetal development. J Nutr 134(9):2169–2172
Mignini LE, Villar J, Khan KS (2006) Mapping the theories of preeclampsia: the need for systematic reviews of mechanisms of the disease. Am J Obstet Gynecol 194(2):317–321
Whitley GS, Cartwright JE (2009) Trophoblast-mediated spiral artery remodelling: a role for apoptosis. J Anat 215(1):21–26
Lima PD et al (2014) Leukocyte driven-decidual angiogenesis in early pregnancy. Cell Mol Immunol 11(6):522–537
de Souza EA, Pisani LP (2020) The relationship among vitamin D, TLR4 pathway and preeclampsia. Mol Biol Rep 47(8):6259–6267
Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365(9461):785–799
Solomon CG, Seely EW (2006) Hypertension in pregnancy. Endocrinol Metab Clin North Am 35(1):157–171
Chappell LC et al (2021) Pre-eclampsia. Lancet 398(10297):341–354
Ness RB, Sibai BM (2006) Shared and disparate components of the pathophysiologies of fetal growth restriction and preeclampsia. Am J Obstet Gynecol 195(1):40–49
Kappou D et al (2015) Role of the angiopoietin/Tie system in pregnancy (Review). Exp Ther Med 9(4):1091–1096
Duhig KE et al (2019) Placental growth factor testing to assess women with suspected pre-eclampsia: a multicentre, pragmatic, stepped-wedge cluster-randomised controlled trial. Lancet 393(10183):1807–1818
Rath G et al (2016) HIF-1 Alpha and placental growth factor in pregnancies complicated with preeclampsia: a qualitative and quantitative analysis. J Clin Lab Anal 30(1):75–83
Maynard SE et al (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 111(5):649–658
Holme AM et al (2016) In vivo uteroplacental release of placental growth factor and soluble Fms-like tyrosine kinase-1 in normal and preeclamptic pregnancies. Am J Obstet Gynecol 215(6):782 e1–782 e9
Gebara N et al (2021) Angiogenic properties of placenta-derived extracellular vesicles in normal pregnancy and in preeclampsia. Int J Mol Sci 22(10):5402
Davidge ST (1998) Oxidative stress and altered endothelial cell function in preeclampsia. Semin Reprod Endocrinol 16(1):65–73
Roberts JM et al (1989) Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol 161(5):1200–1204
Bowyer L, Brown MA, Jones M (2003) Forearm blood flow in pre-eclampsia. BJOG 110(4):383–391
Lampinen KH et al (2006) Impaired vascular dilatation in women with a history of pre-eclampsia. J Hypertens 24(4):751–756
Savvidou MD et al (2003) Endothelial dysfunction and raised plasma concentrations of asymmetric dimethylarginine in pregnant women who subsequently develop pre-eclampsia. Lancet 361(9368):1511–1517
Chambers JC et al (2001) Association of maternal endothelial dysfunction with preeclampsia. JAMA 285(12):1607–1612
Cockell AP, Poston L (1997) Flow-mediated vasodilatation is enhanced in normal pregnancy but reduced in preeclampsia. Hypertension 30(2 Pt 1):247–251
Kublickiene KR et al (2000) Preeclampsia: evidence for impaired shear stress-mediated nitric oxide release in uterine circulation. Am J Obstet Gynecol 183(1):160–166
Deng L et al (1994) Plasma levels of von Willebrand factor and fibronectin as markers of persisting endothelial damage in preeclampsia. Obstet Gynecol 84(6):941–945
Shaarawy M, Didy HE (1996) Thrombomodulin, plasminogen activator inhibitor type 1 (PAI-1) and fibronectin as biomarkers of endothelial damage in preeclampsia and eclampsia. Int J Gynaecol Obstet 55(2):135–139
Szarka A et al (2010) Circulating cytokines, chemokines and adhesion molecules in normal pregnancy and preeclampsia determined by multiplex suspension array. BMC Immunol 11:59
Cindrova-Davies T et al (2011) Soluble FLT1 sensitizes endothelial cells to inflammatory cytokines by antagonizing VEGF receptor-mediated signalling. Cardiovasc Res 89(3):671–679
Gant NF et al (1974) A clinical test useful for predicting the development of acute hypertension in pregnancy. Am J Obstet Gynecol 120(1):1–7
Aggarwal PK et al (2012) The relationship between circulating endothelin-1, soluble fms-like tyrosine kinase-1 and soluble endoglin in preeclampsia. J Hum Hypertens 26(4):236–241
Wang YP et al (1991) The imbalance between thromboxane and prostacyclin in preeclampsia is associated with an imbalance between lipid peroxides and vitamin E in maternal blood. Am J Obstet Gynecol 165(6 Pt 1):1695–1700
McCarthy AL et al (1993) Abnormal endothelial cell function of resistance arteries from women with preeclampsia. Am J Obstet Gynecol 168(4):1323–1330
Var A et al (2003) Endothelial dysfunction in preeclampsia. Increased homocysteine and decreased nitric oxide levels. Gynecol Obstet Invest 56(4):221–224
Knock GA, Poston L (1996) Bradykinin-mediated relaxation of isolated maternal resistance arteries in normal pregnancy and preeclampsia. Am J Obstet Gynecol 175(6):1668–1674
Luksha L et al (2008) Endothelium-derived hyperpolarizing factor in preeclampsia: heterogeneous contribution, mechanisms, and morphological prerequisites. Am J Physiol Regul Integr Comp Physiol 294(2):R510–R519
Pascoal IF et al (1998) Preeclampsia selectively impairs endothelium-dependent relaxation and leads to oscillatory activity in small omental arteries. J Clin Invest 101(2):464–470
Reho JJ et al (2012) Increased myogenic reactivity of uterine arteries from pregnant rats with reduced uterine perfusion pressure. Pregnancy Hypertens 2(2):106–114
Enkhmaa D et al (2016) Preeclampsia and vascular function: a window to future cardiovascular disease risk. J Womens Health (Larchmt) 25(3):284–291
Powe CE, Levine RJ, Karumanchi SA (2011) Preeclampsia, a disease of the maternal endothelium: the role of antiangiogenic factors and implications for later cardiovascular disease. Circulation 123(24):2856–2869
Kelly AC, Powell TL, Jansson T (2020) Placental function in maternal obesity. Clin Sci (Lond) 134(8):961–984
Inzani I, Ozanne SE (2022) Programming by maternal obesity: a pathway to poor cardiometabolic health in the offspring. Proc Nutr Soc 81(3):227–242
Hayman R et al (2000) Plasma from women with pre-eclampsia induces an in vitro alteration in the endothelium-dependent behaviour of myometrial resistance arteries. BJOG 107(1):108–115
Myers J et al (2005) In preeclampsia, the circulating factors capable of altering in vitro endothelial function precede clinical disease. Hypertension 45(2):258–263
Garovic VD, Hayman SR (2007) Hypertension in pregnancy: an emerging risk factor for cardiovascular disease. Nat Clin Pract Nephrol 3(11):613–622
Lazzarin N et al (2012) Hypertension in pregnancy and endothelial activation: an emerging risk factor for cardiovascular disease. Pregnancy Hypertens 2(4):393–397
Vedmedovska N et al (2011) Placental pathology in fetal growth restriction. Eur J Obstet Gynecol Reprod Biol 155(1):36–40
Triunfo S et al (2014) Angiogenic factors at diagnosis of late-onset small-for-gestational age and histological placental underperfusion. Placenta 35(6):398–403
Noris M, Perico N, Remuzzi G (2005) Mechanisms of disease: pre-eclampsia. Nat Clin Pract Nephrol 1(2):98–114
Sukenik-Halevy R et al (2016) Telomere homeostasis in trophoblasts and in cord blood cells from pregnancies complicated with preeclampsia. Am J Obstet Gynecol 214(2):283 e1–283 e7
Londero AP et al (2016) Placental aging and oxidation damage in a tissue micro-array model: an immunohistochemistry study. Histochem Cell Biol 146(2):191–204
Yang JI et al (2015) The proteomic analysis of human placenta with pre-eclampsia and normal pregnancy. J Korean Med Sci 30(6):770–778
Friedman SA et al (1995) Biochemical corroboration of endothelial involvement in severe preeclampsia. Am J Obstet Gynecol 172(1 Pt 1):202–203
Salazar Garcia MD et al (2018) Early pregnancy immune biomarkers in peripheral blood may predict preeclampsia. J Reprod Immunol 125:25–31
Suvakov S et al (2019) Targeting senescence improves angiogenic potential of adipose-derived mesenchymal stem cells in patients with preeclampsia. Biol Sex Differ 10(1):49
Suvakov S et al (2021) Epigenetic and senescence markers indicate an accelerated ageing-like state in women with preeclamptic pregnancies. EBioMedicine 70:103536
Redman CW, Sargent IL (2009) Placental stress and pre-eclampsia: a revised view. Placenta 30:S38–S42
Gluckman PD et al (2009) Epigenetic mechanisms that underpin metabolic and cardiovascular diseases. Nat Rev Endocrinol 5(7):401
Wolf HT et al (2017) Multivitamin use and adverse birth outcomes in high-income countries: a systematic review and meta-analysis. Am J Obstet Gynecol 217(4):404 e1–404 e30
Barker DJ (2007) The origins of the developmental origins theory. J Intern Med 261(5):412–417
Esplin MS et al (2001) Paternal and maternal components of the predisposition to preeclampsia. N Engl J Med 344(12):867–872
Bateson P et al (2004) Developmental plasticity and human health. Nature 430(6998):419–421
Gluckman PD et al (2008) Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 359(1):61–73
Godfrey KM, Barker DJ (2000) Fetal nutrition and adult disease. Am J Clin Nutr 71(5 Suppl):1344S–1352S
Kwon EJ, Kim YJ (2017) What is fetal programming?: a lifetime health is under the control of in utero health. Obstet Gynecol Sci 60(6):506–519
Man AWC et al (2020) Involvement of gut microbiota, microbial metabolites and interaction with polyphenol in host immunometabolism. Nutrients 12(10):3054
Man AWC et al (2020) Fetal programming effects of pentaerythritol tetranitrate in a rat model of superimposed preeclampsia. J Mol Med (Berl) 98(9):1287–1299
Kulandavelu S et al (2012) Endothelial nitric oxide synthase deficiency reduces uterine blood flow, spiral artery elongation, and placental oxygenation in pregnant mice. Hypertension 60(1):231–238
Boeldt DS, Yi FX, Bird IM (2011) eNOS activation and NO function: pregnancy adaptive programming of capacitative entry responses alters nitric oxide (NO) output in vascular endothelium-new insights into eNOS regulation through adaptive cell signaling. J Endocrinol 210(3):243–258
Devendran A et al (2015) Allele, genotype and haplotype structures of functional polymorphic variants in endothelial nitric oxide synthase (eNOS), angiotensinogen (ACE) and aldosterone synthase (CYP11B2) genes in healthy pregnant women of Indian ethnicity. J Reprod Infertil 16(4):180–192
Suzuki T et al (2009) Gestational changes in production of NO and expression of NOS mRNA isoforms in the rat placenta. J Vet Med Sci 71(4):495–498
Shaheen G et al (2021) Association of endothelial nitric oxide synthase gene variants with preeclampsia. Reprod Health 18(1):163
Aggarwal PK, Jain V, Jha V (2010) Endothelial nitric oxide synthase, angiotensin-converting enzyme and angiotensinogen gene polymorphisms in hypertensive disorders of pregnancy. Hypertens Res 33(5):473–477
Li F et al (2012) eNOS deficiency acts through endothelin to aggravate sFlt-1-induced pre-eclampsia-like phenotype. J Am Soc Nephrol 23(4):652–660
Marshall SA et al (2018) Animal models of preeclampsia: translational failings and why. Am J Physiol Regul Integr Comp Physiol 314(4):R499–R508
Sunderland N, Hennessy A, Makris A (2011) Animal models of pre-eclampsia. Am J Reprod Immunol 65(6):533–541
Bakrania BA, George EM, Granger JP (2022) Animal models of preeclampsia: investigating pathophysiology and therapeutic targets. Am J Obstet Gynecol 226(2S):S973–S987
Lemery Magnin M et al (2018) Assessment of placental perfusion in the preeclampsia L-NAME rat model with high-field dynamic contrast-enhanced MRI. Fetal Diagn Ther 44(4):277–284
de Alwis N et al (2022) The L-NAME mouse model of preeclampsia and impact to long-term maternal cardiovascular health. Life Science Alliance 5(12)
Diket AL et al (1994) Nitric oxide inhibition causes intrauterine growth retardation and hind-limb disruptions in rats. Am J Obstet Gynecol 171(5):1243–1250
Eremina V et al (2003) Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest 111(5):707–716
Gillis EE et al (2015) The Dahl salt-sensitive rat is a spontaneous model of superimposed preeclampsia. Am J Physiol Regul Integr Comp Physiol 309(1):R62–R70
Terstappen F et al (2019) Prenatal Sildenafil therapy improves cardiovascular function in fetal growth restricted offspring of Dahl salt-sensitive rats. Hypertension 73(5):1120–1127
Dasinger JH et al (2020) Development of maternal syndrome in the Dahl salt-sensitive rats is dependent on T cells. Faseb J 34(S1):1–1
Terstappen F et al (2020) Sodium thiosulfate in the pregnant Dahl salt-sensitive rat, a model of preeclampsia. Biomolecules 10(2):302
Turbeville HR et al (2019) Superimposed preeclampsia exacerbates postpartum renal injury despite lack of long-term blood pressure difference in the Dahl salt-sensitive rat. Hypertension 73(3):650–658
Podjarny E, Losonczy G, Baylis C (2004) Animal models of preeclampsia. Semin Nephrol 24(6):596–606
Roberts JM, Hubel CA (1999) Is oxidative stress the link in the two-stage model of pre-eclampsia? Lancet 354(9181):788–789
Mando C et al (2014) Placental mitochondrial content and function in intrauterine growth restriction and preeclampsia. Am J Physiol Endocrinol Metab 306(4):E404–E413
Luo S et al (2014) Molecular mechanisms of endothelial NO synthase uncoupling. Curr Pharm Des 20(22):3548–3553
Guerby P et al (2021) Role of oxidative stress in the dysfunction of the placental endothelial nitric oxide synthase in preeclampsia. Redox Biol 40:101861
Venkatesha S et al (2006) Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 12(6):642–649
Shen L et al (2018) Placenta-associated serum exosomal miR-155 derived from patients with preeclampsia inhibits eNOS expression in human umbilical vein endothelial cells. Int J Mol Med 41(3):1731–1739
Nnate DA, Mabhala M, Massey A (2020) Effectiveness of nitric oxide agents in preventing the early onset of pre-eclampsia and possible modification of metabolic factors in high-risk pregnancies: a systematic review protocol. JBI Evid Synth 18(12):2658–2665
Ignarro LJ et al (1987) Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc Natl Acad Sci U S A 84(24):9265–9269
Krause BJ, Hanson MA, Casanello P (2011) Role of nitric oxide in placental vascular development and function. Placenta 32(11):797–805
Hamik A, Wang B, Jain MK (2006) Transcriptional regulators of angiogenesis. Arterioscler Thromb Vasc Biol 26(9):1936–1947
McDonald CR et al (2018) Malaria in pregnancy alters l-arginine bioavailability and placental vascular development. Sci Transl Med 10(431):eaan6007
Socco S et al (2017) Epigenetics: the third pillar of nitric oxide signaling. Pharmacol Res 121:52–58
Vasudevan D et al (2015) Nitric oxide regulates gene expression in cancers by controlling histone posttranslational modifications. Cancer Res 75(24):5299–5308
Foster MW, McMahon TJ, Stamler JS (2003) S-nitrosylation in health and disease. Trends Mol Med 9(4):160–168
Iyer AK, Rojanasakul Y, Azad N (2014) Nitrosothiol signaling and protein nitrosation in cell death. Nitric Oxide 42:9–18
Zhang HH, Wang YP, Chen DB (2011) Analysis of nitroso-proteomes in normotensive and severe preeclamptic human placentas. Biol Reprod 84(5):966–975
Kulandavelu S et al (2021) S-nitrosoglutathione reductase deficiency causes aberrant placental S-nitrosylation and preeclampsia. bioRxiv 1:183012
Liu W, Hajjar KA (2016) The annexin A2 system and angiogenesis. Biol Chem 397(10):1005–1016
Dasinger JH, Abais-Battad JM, Mattson DL (2020) Influences of environmental factors during preeclampsia. Am J Physiol Regul Integr Comp Physiol 319(1):R26–R32
Gernand AD et al (2016) Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol 12(5):274–289
Suchdev PS, Peña‐Rosas JP, De‐Regil LM (2015) Multiple micronutrient powders for home (point‐of‐use) fortification of foods in pregnant women. Cochrane Database Syst Rev (6):CD011158
Massari M et al (2020) Multiple micronutrients and docosahexaenoic acid supplementation during pregnancy: a randomized controlled study. Nutrients 12(8):2432
Santander Ballestin S et al (2021) Is supplementation with micronutrients still necessary during pregnancy? A review. Nutrients 13(9):3134
Martinez-Gonzalez MA, Bes-Rastrollo M (2014) Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol 25(1):20–26
Khemayanto H, Shi B (2014) Role of Mediterranean diet in prevention and management of type 2 diabetes. Chin Med J (Engl) 127(20):3651–3656
Xu H et al (2009) Role of nutrition in the risk of preeclampsia. Nutr Rev 67(11):639–657
Roberts JM et al (2003) Nutrient involvement in preeclampsia. J Nutr 133(5 Suppl 2):1684S–1692S
Rumbold AR et al (2006) Vitamins C and E and the risks of preeclampsia and perinatal complications. N Engl J Med 354(17):1796–1806
Villar J et al (2006) World Health Organization randomized trial of calcium supplementation among low calcium intake pregnant women. Am J Obstet Gynecol 194(3):639–649
Visek WJ (1986) Arginine needs, physiological state and usual diets. A reevaluation. J Nutr 116(1):36–46
Boger RH, Bode-Boger SM (2001) The clinical pharmacology of L-arginine. Annu Rev Pharmacol Toxicol 41:79–99
Jobgen WS et al (2006) Regulatory role for the arginine-nitric oxide pathway in metabolism of energy substrates. J Nutr Biochem 17(9):571–588
Creager MA et al (1992) L-arginine improves endothelium-dependent vasodilation in hypercholesterolemic humans. J Clin Invest 90(4):1248–1253
Adams MR et al (1997) Oral L-arginine improves endothelium-dependent dilatation and reduces monocyte adhesion to endothelial cells in young men with coronary artery disease. Atherosclerosis 129(2):261–269
Bode-Boger SM et al (1998) L-arginine-induced vasodilation in healthy humans: pharmacokinetic-pharmacodynamic relationship. Br J Clin Pharmacol 46(5):489–497
Dorniak-Wall T et al (2014) The role of L-arginine in the prevention and treatment of pre-eclampsia: a systematic review of randomised trials. J Hum Hypertens 28(4):230–235
Camarena Pulido EE et al (2016) Efficacy of L-arginine for preventing preeclampsia in high-risk pregnancies: a double-blind, randomized, clinical trial. Hypertens Pregnancy 35(2):217–225
Oludare GO, Jinadu HD, Aro OO (2018) L-arginine attenuates blood pressure and reverses the suppression of angiogenic risk factors in a rat model of preeclampsia. Pathophysiology 25(4):389–395
Xu L et al (2022) l-arginine supplementation improved neonatal outcomes in pregnancies with hypertensive disorder or intrauterine growth restriction: A systematic review and meta-analysis of randomized controlled trials. Clin Nutr 41(7):1512–1522
Weckman AM et al (2019) Perspective: L-arginine and L-citrulline supplementation in pregnancy: a potential strategy to improve birth outcomes in low-resource settings. Adv Nutr 10(5):765–777
Ngai M et al (2020) Malaria in pregnancy and adverse birth outcomes: new mechanisms and therapeutic opportunities. Trends Parasitol 36(2):127–137
Aye IL et al (2021) Placental polyamines regulate acetyl-coA and histone acetylation in a sex-dependent manner. bioRxiv 10:2021
Landau G et al (2012) Expression profiling and biochemical analysis suggest stress response as a potential mechanism inhibiting proliferation of polyamine-depleted cells. J Biol Chem 287(43):35825–35837
Park MH, Igarashi K (2013) Polyamines and their metabolites as diagnostic markers of human diseases. Biomol Ther (Seoul) 21(1):1–9
Fenelon JC, Murphy BD (2019) New functions for old factors: the role of polyamines during the establishment of pregnancy. Reprod Fertil Dev 31(7):1228–1239
Bazer FW et al (2018) Mechanisms for the establishment and maintenance of pregnancy: synergies from scientific collaborations. Biol Reprod 99(1):225–241
Hsu CN, Tain YL (2019) Impact of arginine nutrition and metabolism during pregnancy on offspring outcomes. Nutrients 11(7):1452
Kalac P (2014) Health effects and occurrence of dietary polyamines: a review for the period 2005-mid 2013. Food Chem 161:27–39
Puleston DJ et al (2014) Autophagy is a critical regulator of memory CD8+ T cell formation. Elife 3:e03706
Szabo C et al (1994) Inhibition by spermine of the induction of nitric oxide synthase in J774.2 macrophages: requirement of a serum factor. Br J Pharmacol 112(2):355–356
El-Kirsh AA, Abd El-Wahab HM, Abd-Ellah Sayed HF (2011) The effect of L-arginine or L-citrulline supplementation on biochemical parameters and the vascular aortic wall in high-fat and high-cholesterol-fed rats. Cell Biochem Funct 29(5):414–428
Guerreiro JR et al (2009) Argininosuccinate synthetase is a functional target for a snake venom anti-hypertensive peptide: role in arginine and nitric oxide production. J Biol Chem 284(30):20022–20033
Ham DJ et al (2015) L-Citrulline protects skeletal muscle cells from cachectic stimuli through an iNOS-dependent mechanism. PLoS One 10(10):e0141572
Lee YC et al (2018) L-Arginine and L-Citrulline supplementation have different programming effect on regulatory T-cells function of infantile rats. Front Immunol 9:2911
Osowska S et al (2006) Citrulline modulates muscle protein metabolism in old malnourished rats. Am J Physiol Endocrinol Metab 291(3):E582–E586
Jourdan M et al (2015) Citrulline stimulates muscle protein synthesis in the post-absorptive state in healthy people fed a low-protein diet - a pilot study. Clin Nutr 34(3):449–456
Khalaf D et al (2019) The effects of oral l-Arginine and l-Citrulline supplementation on blood pressure. Nutrients 11(7)
Man AW et al (2022) L-citrulline ameliorates pathophysiology in a rat model of superimposed preeclampsia. Br J Pharmacol:1–17
Gemmel M et al (2021) l-Citrulline supplementation during pregnancy improves perinatal and postpartum maternal vascular function in a mouse model of preeclampsia. Am J Physiol Regul Integr Comp Physiol 321(3):R364–R376
Bourdon A et al (2016) L-Citrulline supplementation enhances fetal growth and protein synthesis in rats with intrauterine growth restriction. J Nutr 146(3):532–541
Tain YL et al (2010) Effects of maternal L-citrulline supplementation on renal function and blood pressure in offspring exposed to maternal caloric restriction: the impact of nitric oxide pathway. Nitric Oxide 23(1):34–41
Koeners MP et al (2007) Maternal supplementation with citrulline increases renal nitric oxide in young spontaneously hypertensive rats and has long-term antihypertensive effects. Hypertension 50(6):1077–1084
Tain YL et al (2014) Maternal citrulline supplementation prevents prenatal dexamethasone-induced programmed hypertension. Free Radic Res 48(5):580–586
Chen Y, Michalak M, Agellon LB (2018) Importance of nutrients and nutrient metabolism on human health. Yale J Biol Med 91(2):95–103
Lobo V et al (2010) Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn Rev 4(8):118–126
Clausen T et al (2001) High intake of energy, sucrose, and polyunsaturated fatty acids is associated with increased risk of preeclampsia. Am J Obstet Gynecol 185(2):451–458
Williams MA et al (1995) Omega-3 fatty acids in maternal erythrocytes and risk of preeclampsia. Epidemiology 6(3):232–237
Innis SM et al (1999) Neonatal polyunsaturated fatty acid metabolism. Lipids 34(2):139–149
Maroon JC, Bost JW (2006) Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol 65(4):326–331
Zheng JS et al (2013) Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. Bmj 346:f3706
Mozaffarian D, Wu JH (2011) Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Coll Cardiol 58(20):2047–2067
Okuda Y et al (1997) Eicosapentaenoic acid enhances nitric oxide production by cultured human endothelial cells. Biochem Biophys Res Commun 232(2):487–491
Omura M et al (2001) Eicosapentaenoic acid (EPA) induces Ca(2+)-independent activation and translocation of endothelial nitric oxide synthase and endothelium-dependent vasorelaxation. FEBS Lett 487(3):361–366
Arvizu M et al (2019) Fat intake during pregnancy and risk of preeclampsia: a prospective cohort study in Denmark. Eur J Clin Nutr 73(7):1040–1048
Bakouei F et al (2020) Efficacy of n-3 fatty acids supplementation on the prevention of pregnancy induced-hypertension or preeclampsia: A systematic review and meta-analysis. Taiwan J Obstet Gynecol 59(1):8–15
Jones ML, Mark PJ, Waddell BJ (2014) Maternal dietary omega-3 fatty acids and placental function. Reproduction 147(5):R143–R152
Firouzabadi FD, Shab-Bidar S, Jayedi A (2022) The effects of omega-3 polyunsaturated fatty acids supplementation in pregnancy, lactation, and infancy: an umbrella review of meta-analyses of randomized trials. Pharmacol Res 177:106100
Bianchi M et al (2019) Maternal intake of n-3 polyunsaturated fatty acids during pregnancy is associated with differential methylation profiles in cord blood white cells. Front Genet 10:1050
Liu X et al (2021) Associations of maternal polyunsaturated fatty acids with telomere length in the cord blood and placenta in Chinese population. Front Nutr 8:779306
Hofmeyr GJ et al (2018) Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev 10(10):CD001059
Belizan JM, Villar J (1980) The relationship between calcium intake and edema-, proteinuria-, and hypertension-getosis: an hypothesis. Am J Clin Nutr 33(10):2202–2210
Belizan JM et al (1983) Preliminary evidence of the effect of calcium supplementation on blood pressure in normal pregnant women. Am J Obstet Gynecol 146(2):175–180
Levine RJ et al (1997) Trial of calcium to prevent preeclampsia. N Engl J Med 337(2):69–76
Belizan JM, Villar J, Repke J (1988) The relationship between calcium intake and pregnancy-induced hypertension: up-to-date evidence. Am J Obstet Gynecol 158(4):898–902
Cullers A et al (2019) Effect of prenatal calcium supplementation on bone during pregnancy and 1 y postpartum. Am J Clin Nutr 109(1):197–206
Jarjou LM et al (2010) Effect of calcium supplementation in pregnancy on maternal bone outcomes in women with a low calcium intake. Am J Clin Nutr 92(2):450–457
Belizan JM et al (1997) Long-term effect of calcium supplementation during pregnancy on the blood pressure of offspring: follow up of a randomised controlled trial. BMJ 315(7103):281–285
Gunabalasingam S et al (2022) Micronutrient supplementation interventions in preconception and pregnant women at increased risk of developing pre-eclampsia: a systematic review and meta-analysis. Eur J Clin Nutr 9:1–21
Raia-Barjat T et al (2021) Vitamin D deficiency during late pregnancy mediates placenta-associated complications. Sci Rep 11(1):20708
Simner CL et al (2020) Investigating a suitable model for the study of vitamin D mediated regulation of human placental gene expression. J Steroid Biochem Mol Biol 199:105576
Schulz EV et al (2017) Maternal vitamin D sufficiency and reduced placental gene expression in angiogenic biomarkers related to comorbidities of pregnancy. J Steroid Biochem Mol Biol 173:273–279
Ekstrom L, Storbjork L, Bjorkhem-Bergman L (2016) Genetic expression profile of vitamin D metabolizing enzymes in the first trimester. Horm Metab Res 48(12):834–839
Palacios C, Kostiuk LK, Pena-Rosas JP (2019) Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev 7(7):CD008873
Lemire J (2000) 1,25-Dihydroxyvitamin D3--a hormone with immunomodulatory properties. Z Rheumatol 59(Suppl 1):24–27
Mohammadi N et al (2020) Placental calcification and vitamin D Deficiency in low-risk pregnant women. Int J Pediatr 8(1):10749–10757
Kinshella MW et al (2021) Effects of maternal nutritional supplements and dietary interventions on placental complications: an umbrella review, meta-analysis and evidence map. Nutrients 13(2):472
Behjat Sasan S et al (2017) The effects of vitamin D supplement on prevention of recurrence of preeclampsia in pregnant women with a history of preeclampsia. Obstet Gynecol Int 2017:8249264
Arain N, Mirza WA, Aslam M (2015) Review-Vitamin D and the prevention of preeclampsia: A systematic review. Pak J Pharm Sci 28(3):1015–1021
Phillips EA et al (2022) Vitamin D supplementation improves mitochondrial function and reduces inflammation in placentae of obese women. Front Endocrinol (Lausanne) 13:893848
Dahma G et al (2022) The influence of maternal vitamin D supplementation in pregnancies associated with preeclampsia: a case-control study. Nutrients 14(15):3008
Asemi Z et al (2013) Effects of vitamin D supplementation on glucose metabolism, lipid concentrations, inflammation, and oxidative stress in gestational diabetes: a double-blind randomized controlled clinical trial. Am J Clin Nutr 98(6):1425–1432
Grant CC et al (2014) Vitamin D during pregnancy and infancy and infant serum 25-hydroxyvitamin D concentration. Pediatrics 133(1):e143–e153
Jakubiec-Wisniewska K, Huras H, Kolak M (2022) Effect of vitamin D supplementation on the cerebral placental ratio in pregnancy complicated with early fetal growth restriction. J Clin Med 11(9):2627
Crozier SR et al (2012) Maternal vitamin D status in pregnancy is associated with adiposity in the offspring: findings from the Southampton Women’s Survey. Am J Clin Nutr 96(1):57–63
Rose RC, Bode AM (1993) Biology of free radical scavengers: an evaluation of ascorbate. Faseb J 7(12):1135–1142
Mikhail MS et al (1994) Preeclampsia and antioxidant nutrients: decreased plasma levels of reduced ascorbic acid, alpha-tocopherol, and beta-carotene in women with preeclampsia. Am J Obstet Gynecol 171(1):150–157
Kharb S (2000) Vitamin E and C in preeclampsia. Eur J Obstet Gynecol Reprod Biol 93(1):37–39
Poranen AK et al (1996) Lipid peroxidation and antioxidants in normal and pre-eclamptic pregnancies. Placenta 17(7):401–405
Bowen RS et al (2001) Oxidative stress in pre-eclampsia. Acta Obstet Gynecol Scand 80(8):719–725
Sagol S, Ozkinay E, Ozsener S (1999) Impaired antioxidant activity in women with pre-eclampsia. Int J Gynaecol Obstet 64(2):121–127
Panburana P, Phuapradit W, Puchaiwatananon O (2000) Antioxidant nutrients and lipid peroxide levels in Thai preeclamptic pregnant women. J Obstet Gynaecol Res 26(5):377–381
Price KD, Price CS, Reynolds RD (2001) Hyperglycemia-induced ascorbic acid deficiency promotes endothelial dysfunction and the development of atherosclerosis. Atherosclerosis 158(1):1–12
Gulmezoglu AM, Hofmeyr GJ, Oosthuisen MM (1997) Antioxidants in the treatment of severe pre-eclampsia: an explanatory randomised controlled trial. Br J Obstet Gynaecol 104(6):689–696
Chappell LC et al (1999) Effect of antioxidants on the occurrence of pre-eclampsia in women at increased risk: a randomised trial. Lancet 354(9181):810–816
Yusuf H et al (2019) Associations of macro and micronutrients and antioxidants intakes with preeclampsia: a case-control study in Jordanian pregnant women. Nutr Metab Cardiovasc Dis 29(5):458–466
Lorzadeh N, Kazemirad Y, Kazemirad N (2020) Investigating the preventive effect of vitamins C and E on preeclampsia in nulliparous pregnant women. J Perinat Med 48(6):625–629
Beazley D et al (2005) Vitamin C and E supplementation in women at high risk for preeclampsia: a double-blind, placebo-controlled trial. Am J Obstet Gynecol 192(2):520–521
Fu ZM et al (2018) Vitamins supplementation affects the onset of preeclampsia. J Formos Med Assoc 117(1):6–13
Man AWC, Li H, Xia N (2020) Resveratrol and the Interaction between gut microbiota and arterial remodelling. Nutrients 12(1)
Bo S et al (2013) Anti-inflammatory and antioxidant effects of resveratrol in healthy smokers a randomized, double-blind, placebo-controlled, cross-over trial. Curr Med Chem 20(10):1323–1331
Peluso I et al (2018) Antioxidant, anti-inflammatory, and microbial-modulating activities of nutraceuticals and functional foods 2018. Oxidative Med Cell Longev 2018:3824509
Aguilar-Alonso P et al (2018) Evaluation of oxidative stress in cardiomyocytes during the aging process in rats treated with resveratrol. Oxidative Med Cell Longev 2018:1390483
Li H, Xia N, Förstermann U (2012) Cardiovascular effects and molecular targets of resveratrol. Nitric Oxide 26(2):102–110
Baur JA, Sinclair DA (2006) Therapeutic potential of resveratrol: the in vivo evidence. Nat RevDrug Discov 5(6):493
Springer M, Moco S (2019) Resveratrol and its human metabolites—effects on metabolic health and obesity. Nutrients 11(1):143
Li H et al (2019) Resveratrol and vascular function. Int J Mole Sci 20(9):2155
Ma C et al (2015) Anti-inflammatory effect of resveratrol through the suppression of NF-κB and JAK/STAT signaling pathways. Acta Biochim Et Biophysica Sinica 47(3):207–213
Sun Y et al (2014) Pharmacological activation of AMPK ameliorates perivascular adipose/endothelial dysfunction in a manner interdependent on AMPK and SIRT1. Pharmacol Res 89:19–28
Ding J et al (2017) Efficacy of resveratrol to supplement oral nifedipine treatment in pregnancy-induced preeclampsia. Endocr Connect 6(8):595–600
Darby JRT et al (2019) Subcutaneous maternal resveratrol treatment increases uterine artery blood flow in the pregnant ewe and increases fetal but not cardiac growth. J Physiol 597(20):5063–5077
Bourque SL et al (2012) Maternal resveratrol treatment during pregnancy improves adverse fetal outcomes in a rat model of severe hypoxia. Placenta 33(5):449–452
Bueno-Pereira TO et al (2022) Markers of endothelial dysfunction are attenuated by resveratrol in preeclampsia. Antioxidants (Basel) 11(11)
Liu J, Yao L, Wang Y (2022) Resveratrol alleviates preeclampsia-like symptoms in rats through a mechanism involving the miR-363-3p/PEDF/VEGF axis. Microvasc Res 146:104451
Darby JRT et al (2019) Systematic review: impact of resveratrol exposure during pregnancy on maternal and fetal outcomes in animal models of human pregnancy complications-Are we ready for the clinic? Pharmacol Res 144:264–278
Brawerman GM et al (2019) Maternal resveratrol administration protects against gestational diabetes-induced glucose intolerance and islet dysfunction in the rat offspring. J Physiol 597(16):4175–4192
Castro-Rodriguez DC et al (2021) Maternal obesity (MO) programs morphological changes in aged rat offspring small intestine in a sex dependent manner: effects of maternal resveratrol supplementation. Exp Gerontol 154:111511
Viana-Mattioli S et al (2020) Analysis of SIRT1 expression in plasma and in an in vitro model of preeclampsia. Oxid Med Cell Longev 2020:4561083
Huang Y, Zheng XD, Li H (2021) Protective role of SIRT1-mediated Sonic Hedgehog signaling pathway in the preeclampsia rat models. J Assist Reprod Genet 38(7):1843–1851
Wang Y et al (2022) SIRT1 regulates trophoblast senescence in premature placental aging in preeclampsia. Placenta 122:56–65
Man AWC, Li H, Xia N (2019) The role of Sirtuin1 in regulating endothelial function, arterial remodeling and vascular aging. Front Physiol 10:1173
Dang W (2014) The controversial world of sirtuins. Drug Discov Today: Technol 12:e9–e17
Pezzuto JM (2019) Resveratrol: twenty years of growth, development and controversy. Biomole Therap 27(1):1
Chaplin A, Carpéné C, Mercader J (2018) Resveratrol, metabolic syndrome, and gut microbiota. Nutrients 10(11):1651
Ahmadian E et al (2020) Pre-Eclampsia: microbiota possibly playing a role. Pharmacol Res 155:104692
Altemani F et al (2021) Pregnant women who develop preeclampsia have lower abundance of the butyrate-producer Coprococcus in their gut microbiota. Pregnancy Hypertens 23:211–219
Chen X et al (2020) Gut dysbiosis induces the development of pre-eclampsia through bacterial translocation. Gut 69(3):513–522
Funding
Open Access funding enabled and organized by Projekt DEAL. Original works from the authors’ laboratory contributing to this review were supported by grants LI-1042/1-1, LI-1042/3-1, LI-1042/5-1, MA9671/2-1, and XI 139/2-1 from the Deutsche Forschungsgemeinschaft (DFG), Bonn, Germany. HL and NX were supported by a research grant from the Boehringer Ingelheim Foundation for the collaborative research consortium “Novel and neglected cardiovascular risk factors: molecular mechanisms and therapeutic implications.”
Author information
Authors and Affiliations
Contributions
A.W.C.M. wrote the initial draft of the manuscript. Y.Z., N.X., and H.L. critically reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Man, A.W.C., Zhou, Y., Xia, N. et al. Dietary supplements and vascular function in hypertensive disorders of pregnancy. Pflugers Arch - Eur J Physiol 475, 889–905 (2023). https://doi.org/10.1007/s00424-023-02810-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02810-2