Abstract
Purpose
Surgery offers exciting opportunities but comes with demanding challenges that require attention from both surgical program administrators and aspiring surgeons. The hashtag #NoTrainingTodayNoSurgeonsTomorrow on 𝕏 (previously Twitter) underscores the importance of ongoing training. Our scoping review identifies educational challenges and opportunities for the next generation of surgeons, analyzing existing studies and filling gaps in the literature.
Methods
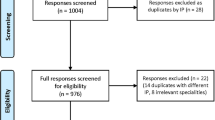
Following the PRISMA guidelines, MEDLINE/PubMed was searched in February 2022, using the MeSH terms “surgeons/education,” for articles in English or German on general, abdominal, thoracic, vascular, and hand surgery and traumatology targeting medical students, surgical residents, future surgeons, and fellows.
Results
The initial search yielded 1448 results. After a step-by-step evaluation process, 32 publications remained for complete review. Three main topics emerged: surgical innovations and training (n = 7), surgical culture and environment (n = 19), and mentoring (n = 6). The articles focusing on surgical innovations and training mainly described the incorporation of structured surgical training methods and program initiatives. Articles on surgical culture examined residents’ burnout, well-being, and gender issues. Challenges faced by women, including implicit bias and sexual harassment, were highlighted. Regarding mentoring, mentees’ needs, training challenges, and the qualities expected of both mentors and mentees were addressed.
Conclusion
At a time of COVID-19-driven surgical innovations, the educational and working environment of the new generation of surgeons is changing. Robotic technology and other innovations require future surgeons to acquire additional technological and digital expertise. With regard to the cultural aspects of training, surgery needs to adapt curricula to meet the demands of the new generation of surgeons, but even more it has to transform its culture.

Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AI:
-
Artificial intelligence
- EPA:
-
Entrustable professional activities
- ETO:
-
Educational time-out
- GA:
-
General autonomy
- HPB:
-
Hepato-pancreato-biliary
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews
- SCS:
-
Swiss College of Surgeons
References
Elnikety S, Badr E, Abdelaal A (2022) Surgical training fit for the future: the need for a change. Postgrad Med J 98(1165):820–823
Bingmer K, Ofshteyn A, Stein SL, Marks JM, Steinhagen E (2020) Decline of open surgical experience for general surgery residents. Surg Endosc 34(2):967–972
Khoushhal Z, Hussain MA, Greco E, Mamdani M, Verma S, Rotstein O et al (2017) Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg 152(3):265–272
Kent TS, Freischlag J, Minter R, Hawn M, Al-Refaie W, James BC et al (2020) Overcoming a hostile work and learning environment in academic surgery-tools for change at every level. J Surg Res 252:281–284
Essex R (2022) How resistance shapes health and well-being. J Bioeth Inq 19(2):315–325
Peters MDJ, Marnie C, Colquhoun H, Garritty CM, Hempel S, Horsley T et al (2021) Scoping reviews: reinforcing and advancing the methodology and application. Syst Rev 10(1):263
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473
Pantoja JL, Archie MM, Baril DT, Moore WS, Lawrence PF (2021) Trainee experience in simulation-based education of open vascular surgery. Ann Vasc Surg 73:147–154
Gerull W, Zihni A, Awad M (2020) Operative performance outcomes of a simulator-based robotic surgical skills curriculum. Surg Endosc 34(10):4543–4548
Summers S, Anderson J, Petzel A, Tarr M, Kenton K (2015) Development and testing of a robotic surgical training curriculum for novice surgeons. J Robot Surg 9(1):27–35
Merali N, Veeramootoo D, Singh S (2019) Eye-Tracking Technology in Surgical Training. J Invest Surg 32(7):587–593
Baimas-George M, Watson M, Martinie J, Vrochides D (2021) Curriculum matrix development for a hepato-pancreato-biliary robotic surgery fellowship. Can J Surg 64(6):E657–E662
Lareyre F, Adam C, Carrier M, Chakfé N, Raffort J (2020) Artificial intelligence for education of vascular surgeons. Eur J Vasc Endovasc Surg 59(6):870–871
Uemura M, Tomikawa M, Miao T, Souzaki R, Ieiri S, Akahoshi T et al (2018) Feasibility of an AI-based measure of the hand motions of expert and novice surgeons. Comput Math Methods Med 2018:9873273
Lebares CC, Braun HJ, Guvva EV, Epel ES, Hecht FM (2018) Burnout and gender in surgical training: a call to re-evaluate coping and dysfunction. Am J Surg 216(4):800–804
Hekman KE, Sullivan BP, Bronsert M, Chang KZ, Reed A, Velazquez-Ramirez G et al (2021) Modifiable risk factors for burnout in vascular surgery trainees. J Vasc Surg 73(6):2155-2163.e3
Zaheer F, Aziz I, Arif S, Khan MO, Khan AA, Osama M et al (2020) Predicament of doctors; discerning burnout level amongst surgical residents of Karachi, Pakistan. J Ayub Med Coll Abbottabad 32(3):331–335
Felton J, Martin O, Kubicki N, Kidd-Romero S, Kavic SM (2021) Understanding the well-being of general surgery residents. Am Surg 87(3):432–436
Janko MR, Smeds MR (2019) Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg 69(4):1233–1242
Nukala M, Freedman-Weiss M, Yoo P, Smeds MR (2020) Sexual harassment in vascular surgery training programs. Ann Vasc Surg 62:92–97
Yeo HL, Abelson JS, Symer MM, Mao J, Michelassi F, Bell R et al (2018) Association of time to attrition in surgical residency with individual resident and programmatic factors. JAMA Surg 153(6):511–517
Audu CO, Coleman DM (2019) Prioritizing personal well-being during vascular surgery training. Semin Vasc Surg 32(1–2):23–26
Gerull KM, Loe M, Seiler K, McAllister J, Salles A (2019) Assessing gender bias in qualitative evaluations of surgical residents. Am J Surg 217(2):306–313
Burgos CM, Josephson A (2014) Gender differences in the learning and teaching of surgery: a literature review. Int J Med Educ 15(5):110–124
Umoetok F, Van Wyk JM, Madiba TE (2017) Does gender impact on female doctors’ experiences in the training and practice of surgery? A single centre study. S Afr J Surg 55(3):8–12
Morton MJ, Sonnad SS (2007) Women on professional society and journal editorial boards. J Natl Med Assoc 99(7):764–771
Myers SP, Hill KA, Nicholson KJ, Neal MD, Hamm ME, Switzer GE et al (2018) A qualitative study of gender differences in the experiences of general surgery trainees. J Surg Res 228:127–134
Schlick CJR, Ellis RJ, Etkin CD, Greenberg CC, Greenberg JA, Turner PL et al (2021) Experiences of gender discrimination and sexual harassment among residents in general surgery programs across the US. JAMA Surg 156(10):942–952
Meyerson SL, Odell DD, Zwischenberger JB, Schuller M, Williams RG, Bohnen JD et al (2019) The effect of gender on operative autonomy in general surgery residents. Surgery 166(5):738–743
Liang R, Dornan T, Nestel D (2019) Why do women leave surgical training? A qualitative and feminist study. Lancet 393(10171):541–549
Han JJ, Mays JC, Sukhavasi A, Patrick WL, Helmers MR, Iyengar A et al (2021) Characteristics and attitudes of aspiring cardiothoracic surgeons: a survey study. Ann Thorac Surg 112(6):2063–2069
Aziz F, Talhelm L, Keefer J, Krawiec C (2019) Vascular surgery residents spend one fifth of their time on electronic health records after duty hours. J Vasc Surg 69(5):1574–1579
Mohammadzadeh N, Tadbir Vajargah K, Nilforoushan N, Ashouri M, Jafarian A, Emami-Razavi SH (2022) The impact of the COVID-19 pandemic on surgical education: a survey and narrative review. Ann Med Surg (Lond) 82:104598
Coleman JR, Abdelsattar JM, Glocker RJ, RAS-ACS COVID-19 Task Force (2021) COVID-19 pandemic and the lived experience of surgical residents, fellows, and early-career surgeons in the American College of Surgeons. J Am Coll Surg. 232(2):119-135.e20
Smeds MR, Huynh C, Thrush CR, Moursi MM, Amankwah KS (2017) Effects of mentorship on graduating vascular surgery trainees. Ann Vasc Surg 44:234–240
Lin J, Reddy RM (2019) Teaching, mentorship, and coaching in surgical education. Thorac Surg Clin 29(3):311–320
Verrier ED (2019) The surgeon as educator. Thorac Surg Clin 29(3):227–232
Kapadia MR, Hrabe JE, Shelton J, Erdahl LM (2021) Teaching and mentoring early in surgical practice. Am Surg 87(6):933–937
Stephens EH, Goldstone AB, Fiedler AG, Vardas PN, Pattakos G, Lou X et al (2018) Appraisal of mentorship in cardiothoracic surgery training. J Thorac Cardiovasc Surg 156(6):2216–2223
Sudan R, Olivere LA, Nussbaum MS, Dunnington GL (2019) The business of educating the next generation of surgeons. Am J Surg 217(2):205–208
Bingmer K, Wojnarski CM, Brady JT, Stein SL, Ho VP, Steinhagen E (2019) A model for a formal mentorship program in surgical residency. J Surg Res 243:64–70
Champion C, Bennett S, Carver D, El Tawil K, Fabbro S, Howatt N et al (2015) Providing mentorship support to general surgery residents: a model for structured group facilitation. Can J Surg 58(6):372–373
Grunwald T, Krummel T, Sherman R (2004) Advanced technologies in plastic surgery: how new innovations can improve our training and practice. Plast Reconstr Surg 114(6):1556–1567
Sridhar AN, Briggs TP, Kelly JD, Nathan S (2017) Training in robotic surgery-an overview. Curr Urol Rep 18(8):58
Kelley WE (2008) The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. JSLS 12(4):351–357
Bresler L, Perez M, Hubert J, Henry JP, Perrenot C (2020) Residency training in robotic surgery: the role of simulation. J Visc Surg 157(3 Suppl 2):S123–S129
Thomas WEG (2006) Teaching and assessing surgical competence. Ann R Coll Surg Engl 88(5):429–432
Meling TR, Meling TR (2021) The impact of surgical simulation on patient outcomes: a systematic review and meta-analysis. Neurosurg Rev 44(2):843–854
Müller PC, Kuemmerli C, Cizmic A, Sinz S, Probst P, de Santibanes M et al (2022) Learning curves in open, laparoscopic, and robotic pancreatic surgery: a systematic review and proposal of a standardization. Ann Surg Open 3(1):e111
Pernar LIM, Robertson FC, Tavakkoli A, Sheu EG, Brooks DC, Smink DS (2017) An appraisal of the learning curve in robotic general surgery. Surg Endosc 31(11):4583–4596
Ten Cate O, Taylor DR (2021) The recommended description of an entrustable professional activity: AMEE Guide No. 140. Med Teach 43(10):1106–14
Huber T, Richardsen I, Klinger C, Mille M, Roeth AA, AsTerOiD-Study Group (2020) See (n)One, Do (n)One, Teach (n)One: reality of surgical resident training in Germany. World J Surg 44(8):2501–10
Lim WH, Wong C, Jain SR, Ng CH, Tai CH, Devi MK et al (2021) The unspoken reality of gender bias in surgery: a qualitative systematic review. PLoS ONE 16(2):e0246420
Hu YY, Ellis RJ, Hewitt DB, Yang AD, Cheung EO, Moskowitz JT et al (2019) Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med 381(18):1741–1752
Zhang LM, Ellis RJ, Ma M, Cheung EO, Hoyt DB, Bilimoria KY et al (2020) Prevalence, types, and sources of bullying reported by US general surgery residents in 2019. JAMA 323(20):2093–2095
Sorber R, Weaver ML, Tsai LL (2020) Training of male and female surgical residents. JAMA Surg 155(10):998
Bellini MI, Adair A, Fotopoulou C, Graham Y, Hutson A, McNally S et al (2019) Changing the norm towards gender equity in surgery: the women in surgery working group of the Association of Surgeons of Great Britain and Ireland’s perspective. J R Soc Med 112(8):325–329
Singh TSS, Singh A (2018) Abusive culture in medical education: mentors must mend their ways. J Anaesthesiol Clin Pharmacol 34(2):145–147
Smith CB, Saillant NN, Mendoza AE (2021) Perceptions of differences in graduated autonomy between male and female surgical residents. Surgery 170(4):1281–1284
Lillemoe HA, Stonko DP, George BC, Schuller MC, Fryer JP, Sullivan ME et al (2020) A preoperative educational time-out is associated with improved resident goal setting and strengthens educational experiences. J Surg Educ 77(1):18–26
Lane SM, Young KA, Hayek SA, Dove JT, Sharp NE, Shabahang MM et al (2020) Meaningful autonomy in general surgery training: exploring for gender bias. Am J Surg 219(2):240–244
Joh DB, van der Werf B, Watson BJ, French R, Bann S, Dennet E et al (2020) Assessment of autonomy in operative procedures among female and male New Zealand general surgery trainees. JAMA Surg 155(11):1019–1026
Entezami P, Franzblau LE, Chung KC (2012) Mentorship in surgical training: a systematic review. Hand (N Y) 7(1):30–36
Skinner SC, Mazza S, Carty MJ, Lifante JC, Duclos A (2022) Coaching for surgeons: a scoping review of the quantitative evidence. Ann Surg Open 3(3):e179
Zhang H, Isaac A, Wright ED, Alrajhi Y, Seikaly H (2017) Formal mentorship in a surgical residency training program: a prospective interventional study. J Otolaryngol Head Neck Surg 46(1):13
Chia MC, Hu YY, Li RD, Cheung EO, Eng JS, Zhan T et al (2022) Prevalence and risk factors for burnout in U.S. vascular surgery trainees. J Vasc Surg 75(1):308-315.e4
Author information
Authors and Affiliations
Contributions
A.P.: Acquisition of data, writing – Drafting of manuscript, Visualization, Analysis and interpretation of data, Critical revision of manuscript; R.S.: Acquisition of data, writing—Drafting of manuscript, Analysis and interpretation of data, Critical revision of manuscript; D.D.: Acquisition of data, Analysis and interpretation of data, Critical revision of manuscript; P.P.: Study conception and design, Acquisition of data, Analysis and interpretation of data, Critical revision of manuscript; A.B.: Critical revision of manuscript; B.M.: Critical revision of manuscript; J.K.: Study conception and design, Acquisition of data, Visualization, Analysis and interpretation of data, Critical revision of manuscript, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Preregistration of studies
We did not preregister our research with an independent, institutional registry. However, we did create a formal analysis plan for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adisa Poljo and Rosita Sortino share first authorship.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Poljo, A., Sortino, R., Daume, D. et al. Educational challenges and opportunities for the future generation of surgeons: a scoping review. Langenbecks Arch Surg 409, 82 (2024). https://doi.org/10.1007/s00423-024-03270-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03270-7