Abstract
Purpose
The effect of the days of the week on the short-term outcomes after elective surgeries has been suggested; however, such data on esophagectomies remain limited. This study aimed to investigate the association between the day of the week and mortality rates after elective esophagectomy using a large-scale clinical database in Japan.
Methods
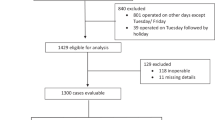
The data of elective esophagectomies, registered in the National Clinical Database in Japan, for esophageal cancer treatment between 2012 and 2017 were analyzed. We hypothesized that the later days of the week could have higher odds ratios of death after elective esophagectomy. With 22 relevant clinical variables and days of surgery, 90-day mortality was evaluated using hierarchical logistic regression modeling.
Results
Ninety-day mortality rates among 33,980 patients undergoing elective esophagectomy were 1.8% (range, 1.5–2.1%). Surgeries were largely concentrated on earlier days of the week, whereas esophagectomies performed on Fridays accounted for only 11.1% of all cases. Before risk adjustment, lower odds ratios of 90-day mortality were found on Tuesday and a tendency towards lower odds ratios on Thursday. In the hierarchical logistic regression model, 21 independent factors of 90-day mortality were identified. However, the adjusted odds ratios of 90-day mortality for Tuesday, Wednesday, Thursday, and Friday were 0.87, 1.09, 0.85, and 0.88, respectively, revealing no significant difference.
Conclusion
The results imply that the variation in 90-day mortality rates after esophagectomy on different days of the week may be attributed to differing preoperative risk factors of the patient group rather than the disparity in medical care provided.


Similar content being viewed by others
Data and/or code availability
All available data was presented in the manuscript and Supplementary Information.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Straatman J, van der Wielen N, Nieuwenhuijzen GA et al (2017) Techniques and short-term outcomes for total minimally invasive Ivor Lewis esophageal resection in distal esophageal and gastroesophageal junction cancers: pooled data from six European centers. Surg Endosc 31:119–126. https://doi.org/10.1007/s00464-016-4938-2
van der Werf LR, Wijnhoven BPL, Fransen LFC et al (2019) A national cohort study evaluating the association between short-term outcomes and long-term survival after esophageal and gastric cancer surgery. Ann Surg 270:868–876. https://doi.org/10.1097/SLA.0000000000003520
Oesophago-Gastric Anastomotic Audit (OGAA), Collaborative: Writing Committee, Steering Committee, National Leads, Site Leads, Collaborators (2021) Mortality from esophagectomy for esophageal cancer across low, middle, and high-income countries: an international cohort study. Eur J Surg Oncol 47:1481–1488. https://doi.org/10.1016/j.ejso.2020.12.006
Kakeji Y, Takahashi A, Hasegawa H et al (2020) Surgical outcomes in gastroenterological surgery in Japan: report of the National Clinical Database 2011-2018. Ann Gastroenterol Surg 4:250–274. https://doi.org/10.1002/ags3.12324
Yoshida N, Eto K, Horinouchi T et al (2022) Preoperative smoking cessation and prognosis after curative esophagectomy for esophageal cancer: a cross-sectional study. Ann Surg Oncol 29:8172–8180. https://doi.org/10.1245/s10434-022-12433-z
Mederos MA, de Virgilio MJ, Shenoy R et al (2021) Comparison of clinical outcomes of robot-assisted, video-assisted, and open esophagectomy for esophageal cancer: a systematic review and meta-analysis. JAMA Netw Open 4:e2129228. https://doi.org/10.1001/jamanetworkopen.2021.29228
Markar SR, Lagergren J (2020) Surgical and surgeon-related factors related to long-term survival in esophageal cancer: a review. Ann Surg Oncol 27:718–723. https://doi.org/10.1245/s10434-019-07966-9
Aylin P, Alexandrescu R, Jen MH et al (2013) Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ 346:f2424. https://doi.org/10.1136/bmj.f2424
Visser E, van Rossum PSN, Verhoeven RHA, Ruurda JP, van Hillegersberg R (2017) Impact of weekday of esophagectomy on short-term and long-term oncological outcomes: a nationwide population-based cohort study in the Netherlands. Ann Surg 266:76–81. https://doi.org/10.1097/SLA.0000000000001909
Jiwnani S, Pramesh CS, Ranganathan P (2023) The “weekday effect”-does it impact esophageal cancer surgery outcomes? J Gastrointest Cancer 54:970–977. https://doi.org/10.1007/s12029-022-00855-7
Lagergren J, Mattsson F, Lagergren P (2016) Weekday of esophageal cancer surgery and its relation to prognosis. Ann Surg 263:1133–1137. https://doi.org/10.1097/SLA.0000000000001324
Lagergren J, Mattsson F, Lagergren P (2016) Weekday of oesophageal cancer surgery in relation to early postoperative outcomes in a nationwide Swedish cohort study. BMJ Open 6:e011097. https://doi.org/10.1136/bmjopen-2016-011097
Miyata H, Gotoh M, Hashimoto H et al (2014) Challenges and prospects of a clinical database linked to the board certification system. Surg Today 44:1991–1999. https://doi.org/10.1007/s00595-013-0802-3
Maeda H, Endo H, Ichihara N et al (2021) Association of day of the week with mortality after elective right hemicolectomy for colon cancer: case analysis from the National Clinical Database. Ann Gastroenterol Surg 5:331–337. https://doi.org/10.1002/ags3.12420
Uemura S, Endo H, Ichihara N et al (2022) Day of surgery and mortality after pancreatoduodenectomy: a retrospective analysis of 29 270 surgical cases of pancreatic head cancer from Japan. J Hepatobiliary Pancreat Sci 29:778–784. https://doi.org/10.1002/jhbp.1043
Maeda H, Endo H, Ichihara N et al (2022) Correlation between surgical mortality for perforated peritonitis and days of the week for operations: a retrospective study using the Japanese National Clinical Database. Am J Surg 224:546–551. https://doi.org/10.1016/j.amjsurg.2022.02.038
Motoyama S, Yamamoto H, Miyata H et al (2020) Impact of certification status of the institute and surgeon on short-term outcomes after surgery for thoracic esophageal cancer: evaluation using data on 16,752 patients from the National Clinical Database in Japan. Esophagus 17:41–49. https://doi.org/10.1007/s10388-019-00694-9
Govindarajan A, Urbach DR, Kumar M et al (2015) Outcomes of daytime procedures performed by attending surgeons after night work. N Engl J Med 373:845–853. https://doi.org/10.1056/NEJMsa1415994
Concha OP, Gallego B, Hillman K, Delaney GP, Coiera E (2014) Do variations in hospital mortality patterns after weekend admission reflect reduced quality of care or different patient cohorts? A population-based study. BMJ Qual Saf 23:215–222. https://doi.org/10.1136/bmjqs-2013-002218
Visser E, van Rossum PSN, Ruurda JP, van Hillegersberg R (2017) Impact of lymph node yield on overall survival in patients treated with neoadjuvant chemoradiotherapy followed by esophagectomy for cancer: a population-based cohort study in the Netherlands. Ann Surg 266:863–869. https://doi.org/10.1097/SLA.0000000000002389
Acknowledgements
We appreciate all participants for their contributions to data registration in the National Clinical Database. This study was evaluated and accepted by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. This work was supported by the Japanese Society of Hepato-Biliary-Pancreatic Surgery in terms of funding and assistance in setting up and recording research meetings.
Funding
This study was supported by the Japanese Society of Hepato-Biliary-Pancreatic Surgery.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design: Dr Endo Hideki, Dr. Ichihara Nao, and Dr. Miyata Hiroaki had full access to all of the data in the study and took responsibility for the integrity of the data. Data analysis was performed by Dr. Endo Hideki and Dr. Ichihara Nao. All authors contributed to the interpretation. Dr. Maeda Hiromichi, Dr. Endo Hideki, Dr. Uemura Sunao, and Dr. Hanazaki Kazuhiro made significant contributions to manuscript drafting. All authors reviewed the manuscript. Dr. Kakeji Yoshihiro and Dr. Kitagawa Yuko performed critical revisions of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study’s protocol was accepted by the Japanese Society of Gastrointestinal Surgery and the Japanese Society of Hepato-Biliary-Pancreatic Surgery Committees. The study protocol was approved by the institutional review board of Kochi Medical School (ID: 31-67).
Consent to participate
The requirement for individual written informed consent was waived due to the retrospective design of this study.
Consent for publication
The requirement for individual written informed consent was waived due to the retrospective design of this study.
Competing interests
Dr. Hideki Endo, Dr. Nao Ichihara, and Dr. Hiroaki Miyata are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo, which is a social collaboration department supported by the National Clinical Database, Johnson & Johnson K.K., Nipro Corporation, and Intuitive Surgical Sàrl. Dr. Kitagawa reports grants and personal fees from ASAHI KASEI PHARMA CORPORATION, grants and personal fees from ONO PHARMACEUTICAL CO., LTD., grants, personal fees and other from TAIHO PHARMACEUTICAL CO., LTD, grants, personal fees and other from CHUGAI PHARMACEUTICAL CO., LTD., grants and personal fees from KAKEN PHARMACEUTICAL CO., LTD., grants and personal fees from EA Pharma Co., Ltd., grants and personal fees from Takeda Pharmaceutical Company Limited, grants and personal fees from TSUMURA & CO., personal fees from AstraZeneca K.K., personal fees from Ethicon Inc., personal fees from Olympus Corporation, personal fees from Cardinal Health K.K., personal fees from SHIONOGI & CO., LTD., personal fees from Bristol-Myers Squibb K.K., personal fees from MSD K.K., personal fees from Smith & Nephew KK, personal fees from ASKA Pharmaceutical Co., Ltd., personal fees from MIYARISAN PHARMACEUTICAL CO. LTD., personal fees from Toray Industries, Inc., personal fees from DAIICHI SANKYO COMPANY, LIMITED, personal fees from Chugai Foundation for Innovative Drug Discovery Science, personal fees from Nippon Kayaku Co., Ltd., personal fees from Intuitive Surgical G.K., personal fees and other from SYSMEX CORPORATION, personal fees from AI Medical Service Inc., personal fees from Kowa Company, Ltd., personal fees from Eisai Co., Ltd., other from Medicaroid Corporation, outside the submitted work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 41 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maeda, H., Endo, H., Ichihara, N. et al. Days of the week and 90-day mortality after esophagectomy: analysis of 33,980 patients from the National Clinical Database. Langenbecks Arch Surg 409, 36 (2024). https://doi.org/10.1007/s00423-023-03214-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03214-7