Abstract
Objective
This study evaluated the prevalence and perioperative risk factors for early high-output ileostomy (EHOI) and developed a precise nomogram model to predict the occurrence of EHOI.
Methods
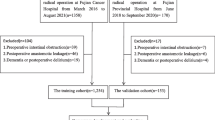
140 patients who underwent ileostomy surgery at three hospitals in Wuhan, Hubei Province, between January 2022 and May 2022 were enrolled in this prospective cohort study. By using univariate and multifactorial logistic regression, independent risk variables for the development of EHOI were examined, and the nomogram model for predicting the risk of EHOI was created by using R software. The calibration curve and area under the receiver operating characteristic curve (ROC AUC) were used to evaluate the calibration and discrimination of the prediction model, Hosmer–Lemeshow to verify the fit of the model. Clinical impact curve (CIC) and decision curve analysis (DCA) were used to assess the model's clinical efficacy.
Results
A total of 132 patients participated in the study, and the incidence of EHOI was 25.8% (34/132). The nomogram model incorporated 3 risk factors hypertension, drinking habits, and high white blood cell (WBC) count after surgery. The AUC was 0.742, and the nomogram showed great calibration and clinical validity by comparing the calibration curve, DCA, and CIC.
Conclusions
Hypertension, drinking, and high WBC was significantly correlated with EHOI. The nomogram model has great clinical value in predicting the EHOI.





Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
References
Yuan JM, Zhang JE, Zheng MC, Bu XQ (2018) Stigma and its influencing factors among Chinese patients with stoma. Psychooncology 27:1565–1571. https://doi.org/10.1002/pon.4695
Dossa F, Josse J, Acuna SA, Baxter NN (2018) Health State Utility Values for Ileostomies and Colostomies: a Systematic Review and Meta-Analysis. J Gastrointest Surg 22:894–905. https://doi.org/10.1007/s11605-018-3671-7
Murken DR, Bleier JIS (2019) Ostomy-Related Complications. Clin Colon Rectal Surg 32:176–182. https://doi.org/10.1055/s-0038-1676995
Nakanishi R, Konishi T, Nakaya E, Zaitsu Y, Mukai T, Yamaguchi T, Nagasaki T, Akiyoshi T, Nagayama S, Fukunaga Y (2021) Predisposing factors and clinical impact of high-output syndrome after sphincter-preserving surgery with covering ileostomy for rectal cancer: a retrospective single-center cohort study. Int J Clin Oncol 26:118–125. https://doi.org/10.1007/s10147-020-01781-z
Fielding A, Woods R, Moosvi SR, Wharton RQ, Speakman CTM, Kapur S, Shaikh I, Hernon JM, Lines SW, Stearns AT (2020) Renal impairment after ileostomy formation: a frequent event with long-term consequences. Colorectal Dis 22:269–278. https://doi.org/10.1111/codi.14866
Arenas Villafranca JJ, López-Rodríguez C, Abilés J, Rivera R, Gándara Adán N, Utrilla Navarro P (2015) Protocol for the detection and nutritional management of high-output stomas. Nutr J 14:45–45. https://doi.org/10.1186/s12937-015-0034-z
Santamaría MM, Villafranca JJA, Abilés J, Ruiz FR, Navarro PU, Goitia BT (2021) Impact of a nutrition consultation on the rate of high output stoma-related readmission: an ambispective cohort study. Sci Rep 11:16620. https://doi.org/10.1038/s41598-021-96136-7
Seifarth C, Augustin LN, Lehmann KS, Stroux A, Lauscher JC, Kreis ME, Holmer C (2021) Assessment of Risk Factors for the Occurrence of a High-Output Ileostomy. Front Surg 8: 642288. https://doi.org/10.3389/fsurg.2021.642288
Baker ML, Williams RN, Nightingale JM (2011) Causes and management of a high-output stoma. Colorectal Dis 13:191–197. https://doi.org/10.1111/j.1463-1318.2009.02107.x
Takeda M, Takahashi H, Haraguchi N, Miyoshi N, Hata T, Yamamoto H, Matsuda C, Mizushima T, Doki Y, Mori M (2019) Factors predictive of high-output ileostomy: a retrospective single-center comparative study. Surg Today 49:482–487. https://doi.org/10.1007/s00595-018-1756-2
Yde J, Larsen HM, Laurberg S, Krogh K, Moeller HB (2018) Chronic diarrhea following surgery for colon cancer-frequency, causes and treatment options. Int J Colorectal Dis 33:683–694. https://doi.org/10.1007/s00384-018-2993-y
Gaertner WB, Madoff RD, Mellgren A, Kwaan MR, Melton GB (2015) Postoperative diarrhea and high ostomy output impact postoperative outcomes after elective colon and rectal operations regardless of Clostridium difficile infection. Am J Surg 210:759–765. https://doi.org/10.1016/j.amjsurg.2015.03.032
Ohta H, Miyake T, Ueki T, Kojima M, Kawasaki M, Tatsuta T, Iuchi T, Kamitani S, Shimizu T, Mekata E, Tani M (2022) Predictors and clinical impact of postoperative diarrhea after colorectal cancer surgery: a prospective, multicenter, observational study (SHISA-1602). Int J Colorectal Dis 37:657–664. https://doi.org/10.1007/s00384-022-04097-8
Hongqiu G, Junfeng W, Zhongheng Z, Zhirui Z (2019) Clinical Prediction Models: Model Development. Chin J Evid Bases Cardiovasc Med 11(14–16):23. https://doi.org/10.3969/j.issn.1674-4055.2019.01.04
Fujino S, Miyoshi N, Ohue M, Takahashi Y, Yasui M, Sugimura K, Akita H, Takahashi H, Kobayashi S, Yano M, Sakon M (2017) Prediction model and treatment of high-output ileostomy in colorectal cancer surgery. Mol Clin Oncol 7:468–472. https://doi.org/10.3892/mco.2017.1336
Cottam J, Richards K, Hasted A, Blackman A (2007) Results of a nationwide prospective audit of stoma complications within 3 weeks of surgery. Colorectal Dis 9:834–838. https://doi.org/10.1111/j.1463-1318.2007.01213.x
Hara Y, Miura T, Sakamoto Y, Morohashi H, Nagase H, Hakamada K (2020) Organ/space infection is a common cause of high output stoma and outlet obstruction in diverting ileostomy. BMC Surg 20:83. https://doi.org/10.1186/s12893-020-00734-7
Kamal A, Fain C, Park A, Wang P, Gonzalez-Velez E, Leffler DA, Hutfless SM (2019) Angiotensin II receptor blockers and gastrointestinal adverse events of resembling sprue-like enteropathy: a systematic review. Gastroenterol Rep 7:162–167. https://doi.org/10.1093/gastro/goz019
Barron AJ, Zaman N, Cole GD, Wensel R, Okonko DO, Francis DP (2013) Systematic review of genuine versus spurious side-effects of beta-blockers in heart failure using placebo control: recommendations for patient information. Int J Cardiol 168:3572–3579. https://doi.org/10.1016/j.ijcard.2013.05.068
Costetti M, Schiepatti A, Fraticelli S, Costa S, Maimaris S, Lenti MV, Villani L, Bianchi PI, Di Sabatino A, Corazza GR, Vanoli A, Biagi F (2021) Clinical and gastro-duodenal histopathological features of enteropathy due to angiotensin II receptor blockers. Dig Liver Dis 53:1262–1267. https://doi.org/10.1016/j.dld.2021.07.002
Meroni M, Longo M, Dongiovanni P (2019) Alcohol or Gut Microbiota: Who Is the Guilty? Int J Mol Sci 20. https://doi.org/10.3390/ijms20184568
Leclercq S, de Timary P, Delzenne NM, Stärkel P (2017) The link between inflammation, bugs, the intestine and the brain in alcohol dependence. Transl Psychiatry 7: e1048. https://doi.org/10.1038/tp.2017.15
Haber PS, Kortt NC (2021) Alcohol use disorder and the gut. Addiction (Abingdon, England) 116:658–667. https://doi.org/10.1111/add.15147
Bode C, Bode JC (2003) Effect of alcohol consumption on the gut. Best Pract Res Clin Gastroenterol 17:575–592. https://doi.org/10.1016/s1521-6918(03)00034-9
Pohl K, Moodley P, Dhanda AD (2021) Alcohol's Impact on the Gut and Liver. Nutrients 13. https://doi.org/10.3390/nu13093170
Hiramoto Y, Kawahara H, Matsumoto T, Takeda M, Misawa T, Yanaga K (2019) Preoperative Neutrophil-lymphocyte Ratio Is a Predictor of High-output Ileostomy After Colorectal Surgery. Anticancer Res 39: 3265–3268. https://doi.org/10.21873/anticanres.13468
Yunjie Z (2015) Overview of research on the mechanism of postoperative diarrhea in colorectal cancer. Chin J Coloproctol 35:59–61. https://doi.org/10.3969/j.issn.1000-1174.2015.01.036
Liyana Z, Norfilza M, Khairul N, Raja AR (2019) A randomized double-blind placebocontrolled trial of probiotics in post-surgical colorectal cancer. BMC Gastroenterol 19:131. https://doi.org/10.1186/s12876-019-1047-4
Yang Y, Xia Y, Chen H, Hong L, Feng J, Yang J, Yang Z, Shi C, Wu W, Gao R, Wei Q, Qin H, Ma Y (2016) The effect of perioperative probiotics treatment for colorectal cancer: short-term outcomes of a randomized controlled trial. Oncotarget 7: 8432–8440. https://doi.org/10.18632/oncotarget.7045
Wei L, Champman S, Li X, Li X, Li S, Chen R, Bo N, Chater A, Horne R (2017) Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open 7: e017293. https://doi.org/10.1136/bmjopen-2017-017293
Acknowledgements
The authors wish to express their gratitude to all investigators and participants of the studies included in this analysis.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Conceptualization, methodology, and writing of the original: Ying Chen; Formal analysis and investigation: Ying Chen; Writing—review and editing: Zhongxiang Cai, Yan Liu; Resources: Zhongxiang Cai, Jun Zhong; Supervision: Fan Cheng.
Corresponding author
Ethics declarations
Competing interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
The studies involving human participants were reviewed and approved by Clinical Research Ethics Committee of Renmin Hospital of Wuhan University. The patients/participants provided their written informed consent to participate in this study(no: WDRY2022-K063).
Consent to participate
Informed consent was obtained from all the individual participants included in the study.
Consent to publish
Informed consent was obtained from all the participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Cai, Z., Liu, Y. et al. Assessment of risk factors and establishment of a nomogram model to predict early high-output ileostomy. Langenbecks Arch Surg 408, 106 (2023). https://doi.org/10.1007/s00423-023-02850-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02850-3