Abstract
Purpose
Technical challenges and a perceived higher risk of complications hinder a wide adoption of minimally invasive pancreatoduodenectomy. We aim to further define the place of minimally invasive pancreatoduodenectomy by comparison with the traditional open approach.
Methods
A comparison of the surgical outcomes and survival after laparoscopic (LPD) versus open pancreatoduodenectomy (OPD) was retrospectively performed from a prospectively kept database. To reduce the effect of bias and confounding, baseline characteristics of both groups were matched using propensity score matching (NCT05110573; Nov 8, 2021; retrospectively registered).
Results
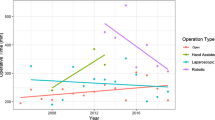
From a total of 67 LPD and 105 OPD patients, propensity score matching resulted in two balanced groups of 38 patients. In both groups, 87% of surgeries were performed for cancer. In the LPD group, conversion rate was 22.4%. Mean operative time was significantly longer after LPD versus OPD (320.1 ± 53.8 vs. 277.7 ± 63.8 min; p = .008). Hospital stay was significantly shorter after LPD versus OPD (median 13.5 vs. 17.0 days; p = .039). No significant differences were observed in blood loss, total complication rate (73.7% vs. 86.8%; p = .249), major complication rate (26.5% vs. 10.5%; p = .137), postoperative pancreatic fistula rate (13.2% vs. 7.9%; p = .711), 90-day mortality rate (5.3% vs. 0%; p = .493), R0 resection rate (85.4% vs. 85.8%), or number of lymph nodes (median 10.0 vs. 8.5; p = .273). In cancer patients, no significant differences were observed in overall survival (median 27.1 vs. 23.9 months; p = .693), disease-free survival, or recurrence rate.
Conclusion
LPD provided acceptable short-term and oncological outcomes. Compared to OPD, we noted a higher major complication rate, without compromising surgical safety or oncological outcomes.



Similar content being viewed by others
Change history
16 February 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00423-023-02824-5
Abbreviations
- PD:
-
Pancreatoduodenectomy
- MIPD:
-
Minimally invasive pancreatoduodenectomy
- RCT:
-
Randomized controlled trial
- RPD:
-
Robotic pancreatoduodenectomy
- LPD:
-
Laparoscopic pancreatoduodenectomies
- OPD:
-
Open pancreatoduodenectomies
- POPF:
-
Postoperative pancreatic fistula
- CR-POPF:
-
Clinically relevant postoperative pancreatic fistula
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- ICU:
-
Intensive care unit
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- DGE:
-
Delayed gastric emptying
- PPH:
-
Post-pancreatectomy haemorrhage
- BMI:
-
Body mass index
- CCI:
-
Charlson Comorbidity Index
- LOS:
-
Length of hospital stay
- CI:
-
Confidence intervals
- PSM:
-
Propensity score matching
- GDA:
-
Gastroduodenal artery
References
Wang S, Shi N, You L, Dai M, Zhao Y (2017) Minimally invasive surgical approach versus open procedure for pancreaticoduodenectomy: a systematic review and meta-analysis Medicine 96(50): e8619. https://doi.org/10.1097/MD.0000000000008619
Cesaretti M, Bifulco L, Costi R, Zarzavadjian Le Bian A (2017) Pancreatic resection in the era of laparoscopy: State of Art A systematic review. Int J Surg 44:309–316. https://doi.org/10.1016/j.ijsu.2017.07.028
Chen K, Pan Y, Xiao-long L et al (2017) Minimally invasive pancreaticoduodenectomy for periampullary disease: a comprehensive review of literature and meta-analysis of outcomes compared with open surgery. BMC Gastroenterol 17:1–15. https://doi.org/10.1186/s12876-017-0691-9
Kamarajah SK, Bundred J, Marc OS, Jiao LR, Manas D, Abu Hilal M, White SA (2020) Robotic versus conventional laparoscopic pancreaticoduodenectomy a systematic review and meta-analysis. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology, 46(1), 6–14. https://doi.org/10.1016/j.ejso.2019.08.007
Yoo D, Song KB, Lee JW et al (2020) A comparative study of laparoscopic versus open pancreaticoduodenectomy for ampulla of vater carcinoma. J Clin Med 9:2214. https://doi.org/10.3390/jcm9072214
Vandeputte M, D’Hondt M, Willems E et al (2019) Stepwise implementation of laparoscopic pancreatic surgery. Case series of a single centre’s experience. Int J Surg 72:137–143. https://doi.org/10.1016/j.ijsu.2019.10.037
Poves I, Burdío F, Morató O et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: : the PADULAP randomized controlled trial. Ann Surg 268:731–739. https://doi.org/10.1097/SLA.0000000000002893
Palanivelu C, Senthilnathan P, Sabnis SC et al (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104:1443–1450. https://doi.org/10.1002/bjs.10662
van Hilst J, de Rooij T, Bosscha K et al (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4:199–207. https://doi.org/10.1016/S2468-1253(19)30004-4
van Hilst J, de Graaf N, Abu Hilal M, Besselink MG (2021) The landmark series: minimally invasive pancreatic resection. Ann Surg Oncol 28:1447–1456. https://doi.org/10.1245/s10434-020-09335-3
Zwart MJW, Nota CLM, de Rooij T et al (2021) Outcomes of a multicenter training program in robotic pancreatoduodenectomy (LAELAPS-3). Ann Surg Publish Ah. https://doi.org/10.1097/sla.0000000000004783
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–96
Ducreux M, Sa Cuhna A, Caramella C et al (2015) Cancer of the pancreas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up †. Ann Oncol 26:56–68. https://doi.org/10.1093/annonc/mdv295
Jimenez RE, Warshaw AL, Fernandez-Del Castillo C (2000) Laparoscopy and peritoneal cytology in the staging of pancreatic cancer. J Hepatobiliary Pancreat Surg 7:15–20. https://doi.org/10.1007/s005340000070015.534
Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, Wellge EB, Kunzler F, Besselink MG, Asbun H, Scott MJ, Dejong CHC, Vrochides D, Aloia T, Izbicki JR, Demartines N (2020) Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World journal of surgery, 44(7): 2056–2084. https://doi.org/10.1007/s00268-020-05462-w
Gouma DJ, Traverso LW, Fingerhut A et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768. https://doi.org/10.1016/j.surg.2007.05.005
Bassi C, Marchegiani G, Dervenis C et al (2017) Pancreas The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161:584–591. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH)-An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25. https://doi.org/10.1016/j.surg.2007.02.001
von Elm E, Altman DG, Egger M et al (2008) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008
Thoemmes F (2012) Propensity score matching in SPSS. arXiv 1201.6385:
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424. https://doi.org/10.1080/00273171.2011.568786
Yao XI, Wang X, Speicher PJ et al (2017) Reporting and guidelines in propensity score analysis: a systematic review of cancer and cancer surgical studies. J Natl Cancer Inst 109:1–9. https://doi.org/10.1093/jnci/djw323
Han SH, Kang CM, Hwang HK et al (2020) The Yonsei experience of 104 laparoscopic pancreaticoduodenectomies: a propensity score-matched analysis with open pancreaticoduodenectomy. Surg Endosc 34:1658–1664. https://doi.org/10.1007/s00464-019-06942-4
Mazzola M, Giani A, Crippa J et al (2020) Totally laparoscopic versus open pancreaticoduodenectomy: a propensity score matching analysis of short-term outcomes. Eur J Surg Oncol 47:674–680. https://doi.org/10.1016/j.ejso.2020.10.036
Shin SH, Kim SC, Song KB et al (2015) A comparative study of laparoscopic vs open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2014.10.014
Yin S-M, Liu Y-W, Liu Y-Y et al (2020) Short-term outcomes after minimally invasive versus open pancreaticoduodenectomy in elderly patients: a propensity score-matched analysis. BMC Surg. https://doi.org/10.1186/s12893-021-01052-2
Bencini L, Tofani F, Paolini C et al (2020) Single-centre comparison of robotic and open pancreatoduodenectomy: a propensity score-matched study. Surg Endosc 34:5402–5412. https://doi.org/10.1007/s00464-019-07335-3
Raoof M, Ituarte PHG, Woo Y et al (2018) Propensity score-matched comparison of oncological outcomes between laparoscopic and open distal pancreatic resection. Br J Surg 105:578–586. https://doi.org/10.1002/bjs.10747
Shi Y, Jin J, Qiu W et al (2020) Short-term outcomes after robot-assisted vs open pancreaticoduodenectomy after the learning curve. JAMA Surg 155:389–394. https://doi.org/10.1001/jamasurg.2020.0021
Cai J, Ramanathan R, Zenati MS et al (2020) Robotic pancreaticoduodenectomy is associated with decreased clinically relevant pancreatic fistulas: a propensity-matched analysis. J Gastrointest Surg 24:1111–1118. https://doi.org/10.1007/s11605-019-04274-1
Austin PC (2014) The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 33:1242–1258. https://doi.org/10.1002/sim.5984
Vollmer CM, Asbun HJ, Barkun J et al (2017) Proceedings of the first international state-of-the-art conference on minimally-invasive pancreatic resection (MIPR). HPB 19:171–177. https://doi.org/10.1016/j.hpb.2017.01.015
Butturini G, Daskalaki D, Molinari E et al (2008) Pancreatic fistula: definition and current problems. J Hepatobiliary Pancreat Surg 15:247–251. https://doi.org/10.1007/s00534-007-1301-y
Hu BY, Wan T, Zhang WZ, Dong JH (2016) Risk factors for postoperative pancreatic fistula: analysis of 539 successive cases of pancreaticoduodenectomy. World J Gastroenterol 22:7797–7805. https://doi.org/10.3748/wjg.v22.i34.7797
Wellner UF, Kayser G, Lapshyn H et al (2010) A simple scoring system based on clinical factors related to pancreatic texture predicts postoperative pancreatic fistula preoperatively. HPB 12:696–702. https://doi.org/10.1111/j.1477-2574.2010.00239.x
de Rooij T, van Hilst J, Topal B et al (2019) Outcomes of a multicenter training program in laparoscopic pancreatoduodenectomy (LAELAPS-2). Ann Surg 269:344–350. https://doi.org/10.1097/SLA.0000000000002563
Stauffer JA, Coppola A, Villacreses D et al (2017) Laparoscopic versus open pancreaticoduodenectomy for pancreatic adenocarcinoma: long-term results at a single institution. Surg Endosc Other Interv Tech 31:2233–2241. https://doi.org/10.1007/s00464-016-5222-1
Kamarajah SK, Bundred J, Saint MO et al (2019) Robotic versus conventional laparoscopic pancreaticoduodenectomy a systematic review and meta-analysis. Eur J Surg Oncol 46:6–14. https://doi.org/10.1016/j.ejso.2019.08.007
Wang M, Meng L, Cai Y et al (2016) Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg 20:924–935. https://doi.org/10.1007/s11605-016-3105-3
Lu C, Jin W, Mou Y-P et al (2016) Analysis of learning curve for laparoscopic pancreaticoduodenectomy. J Vis Surg 2:145. https://doi.org/10.21037/jovs.2016.07.25
Nagakawa Y, Nakamura Y, Honda G et al (2018) Learning curve and surgical factors influencing the surgical outcomes during the initial experience with laparoscopic pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci 25:498–507. https://doi.org/10.1002/jhbp.586
McCulloch P, Cook JA, Altman DG et al (2013) IDEAL framework for surgical innovation 1: the idea and development stages. BMJ 346:f3012. https://doi.org/10.1136/bmj.f3012
Halls MC, Alseidi A, Berardi G, Cipriani F, Van der Poel M, Davila D, Ciria R, Besselink M, D'Hondt M, Dagher I, Alrdrighetti L, Troisi RI, Abu Hilal M (2019) A comparison of the learning curves of laparoscopic liver surgeons in differing stages of the IDEAL paradigm of surgical Innovation: standing on the shoulders of pioneers. Annals of Surgery 269(2):221–228. https://doi.org/10.1097/SLA.0000000000002996
Asbun HJ, Moekotte AL, Vissers FL et al (2020) The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271:1–14. https://doi.org/10.1097/SLA.0000000000003590
Giulianotti PC, Mangano A, Bustos RE et al (2018) Operative technique in robotic pancreaticoduodenectomy (RPD) at University of Illinois at Chicago (UIC): 17 steps standardized technique: lessons learned since the first worldwide RPD performed in the year 2001. Surg Endosc 32:4329–4336. https://doi.org/10.1007/s00464-018-6228-7
Author information
Authors and Affiliations
Contributions
Study conception and design: MV, MDH, FV. Acquisition of data: FV, MDH, MV, CD. Analysis and interpretation of data: MV, MDH. Drafting of manuscript: MV, MDH, WC. Critical revision of manuscript: MDH, WC.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local ethics committee (B3962020000032). This article was written in accordance with the ethical standards of the institutional review board and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all human subjects as is the standard of care and as with compliance with institution guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vandeputte, M., Vansteenkiste, F., Ceelen, W. et al. Morbidity and survival after laparoscopic versus open pancreatoduodenectomy: propensity score matched comparison. Langenbecks Arch Surg 408, 16 (2023). https://doi.org/10.1007/s00423-023-02758-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02758-y