Abstract
Purpose
To evaluate the safety and benefits of major hepatectomy with extrahepatic bile duct resection in older perihilar cholangiocarcinoma patients and to identify possible predictors of surgical mortality.
Methods
We retrospectively analyzed the data of 102 consecutive patients who underwent major hepatectomy with extrahepatic bile duct resection for perihilar cholangiocarcinoma in our institution between 2004 and 2021. The patients were included and divided into two groups: older patients ≥ 75 years and non-older patients < 75 years. Patient characteristics, preoperative nutritional and operative risk scores, intraoperative details, postoperative outcomes, and long-term prognosis were compared between the groups. Univariate and multivariate analyses were used to identify the predictors of 90-day mortality after major hepatectomy with extrahepatic bile duct resection.
Results
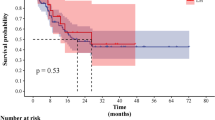
Significant differences were identified for some preoperative surgical risk scores, but not for nutritional scores. Older patients had a higher morbidity rate of respiratory complications (p = 0.016), but there were no significant differences in overall (p = 0.735) or disease-specific survival (p = 0.858). A high Dasari’s score was identified as an independent predictive factor of 90-day mortality.
Conclusions
Major hepatectomy with extrahepatic bile duct resection can be performed for optimally selected older and younger patients with perihilar cholangiocarcinoma, resulting in a good prognosis. However, indications for extended surgery should be recognized. Dasari’s preoperative risk score may be a good predictor of 90-day mortality.



Similar content being viewed by others
References
Aitken R, Harun NS, Maier AB (2021) Which preoperative screening tool should be applied to older patients undergoing elective surgery to predict short-term postoperative outcomes? Lessons from systematic reviews, meta-analyses and guidelines. Intern Emerg Med 16:37–48. https://doi.org/10.1007/s11739-020-02415-y
Yamada M, Nishiguchi S, Fukutani N, Aoyama T, Arai H (2015) Mail-based intervention for sarcopenia prevention increased anabolic hormone and skeletal muscle mass in community-dwelling Japanese older adults: The INE (Intervention by Nutrition and Exercise) Study. J Am Med Dir Assoc 16:654–660. https://doi.org/10.1016/j.jamda.2015.02.017
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y (2013) Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg 258:129–140. https://doi.org/10.1097/SLA.0b013e3182708b57
Findlay JM, Gillies RS, Sgromo B, Marshall REK, Middleton MR, Maynard ND (2014) Individual risk modelling for esophagectomy: a systematic review. J Gastrointest Surg 18:1532–1542. https://doi.org/10.1007/s11605-014-2524-2
Kanda M (2020) Preoperative predictors of postoperative complications after gastric cancer resection. Surg Today 50:3–11. https://doi.org/10.1007/s00595-019-01877-8
Longchamp G, Labgaa I, Demartines N, Joliat GR (2021) Predictors of complications after liver surgery: A systematic review of the literature. HPB (Oxford) 23:645–655. https://doi.org/10.1016/j.hpb.2020.12.009
Oishi K, Itamoto T, Kohashi T, Matsugu Y, Nakahara H, Kitamoto M (2014) Safety of hepatectomy for elderly patients with hepatocellular carcinoma. World J Gastroenterol 20:15028–15036. https://doi.org/10.3748/wjg.v20.i41.15028
Tzeng CW, Cooper AB, Vauthey JN, Curley SA, Aloia TA (2014) Predictors of morbidity and mortality after hepatectomy in elderly patients: analysis of 7621 NSQIP patients. HPB (Oxford) 16:459–468. https://doi.org/10.1111/hpb.12155
Yamada S, Shimada M, Miyake H, Utsunomiya T, Morine Y, Imura S, Ikemoto T, Mori H, Hanaoka J, Iwahashi S, Saito Y (2012) Outcome of hepatectomy in super-elderly patients with hepatocellular carcinoma. Hepatol Res 42:454–458. https://doi.org/10.1111/j.1872-034X.2011.00952.x
Tsujita E, Utsunomiya T, Yamashita Y, Ohta M, Tagawa T, Matsuyama A, Okazaki J, Yamamoto M, Tsutsui S, Ishida T (2012) Outcome of hepatectomy in hepatocellular carcinoma patients aged 80 years and older. Hepatogastroenterology 59:1553–1555. https://doi.org/10.5754/hge09485
Yamashita M, Adachi T, Ono S, Matsumura N, Adachi T, Natsuda K, Hidaka M, Eguchi S (2021) Pancreaticoduodenectomy can be indicated for elderly patients: risk prediction using the estimation of physiologic ability and surgical stress (E-PASS) system. J Hepatobiliary Pancreat Sci 28:165–173. https://doi.org/10.1002/jhbp.840
Al-Refaie WB, Parsons HM, Henderson WG, Jensen EH, Tuttle TM, Vickers SM, Rothenberger DA, Virnig BA (2010) Major cancer surgery in the elderly: results from the American College of Surgeons National Surgical Quality Improvement Program. Ann Surg 251:311–318. https://doi.org/10.1097/SLA.0b013e3181b6b04c
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Brierley JD, Gospodarowicz MK, Wittekind C (2017) TNM Classification of malignant tumors, 8th edn. John Wiley & Sons Ltd, Oxford
Extermann M (2000) Measuring comorbidity in older cancer patients. Eur J Cancer 36:453–471. https://doi.org/10.1016/s0959-8049(99)00319-6
Gomez D, Morris-Stiff G, Toogood GJ, Lodge JP, Prasad KR (2008) Impact of systemic inflammation on outcome following resection for intrahepatic cholangiocarcinoma. J Surg Oncol 97:513–518. https://doi.org/10.1002/jso.21001
Ohira M, Yoshizumi T, Yugawa K, Kosai-Fujimoto Y, Inokuchi S, Motomura T, Mano Y, Toshima T, Itoh S, Harada N, Ikegami T, Soejima Y, Taketomi A, Mori M (2020) Association of inflammatory biomarkers with long-term outcomes after curative surgery for mass-forming intrahepatic cholangiocarcinoma. Surg Today 50:379–388. https://doi.org/10.1007/s00595-019-01905-7
Chen Q, Dai Z, Yin D, Yang LX, Wang Z, Xiao YS, Fan J, Zhou J (2015) Negative impact of preoperative platelet–lymphocyte ratio on outcome after hepatic resection for intrahepatic cholangiocarcinoma. Med (Baltim) 94:e574. https://doi.org/10.1097/MD.0000000000000574
Zhang C, Wang H, Ning Z, Xu L, Zhuang L, Wang P, Meng Z (2016) Prognostic nutritional index serves as a predictive marker of survival and associates with systemic inflammatory response in metastatic intrahepatic cholangiocarcinoma. Onco Targets Ther 9:6417–6423. https://doi.org/10.2147/OTT.S112501
Akgül Ö, Bagante F, Olsen G, Cloyd JM, Weiss M, Merath K, Alexandrescu S, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Koerkamp BG, Guglielmi A, Itaru E, Pawlik TM (2018) Preoperative prognostic nutritional index predicts survival of patients with intrahepatic cholangiocarcinoma after curative resection. J Surg Oncol 118:422–430. https://doi.org/10.1002/jso.25140
Noguchi D, Kuriyama N, Nakagawa Y, Maeda K, Shinkai T, Gyoten K, Hayasaki A, Fujii T, Iizawa Y, Tanemura A, Murata Y, Kishiwada M, Sakurai H, Mizuno S (2021) The prognostic impact of lymphocyte-to-C-reactive protein score in patients undergoing surgical resection for intrahepatic cholangiocarcinoma: a comparative study of major representative inflammatory / immunonutritional markers. PLoS One 16:e0245946. https://doi.org/10.1371/journal.pone.0245946
Pan QX, Su ZJ, Zhang JH, Wang CR, Ke SY (2017) Glasgow prognostic score predicts prognosis of intrahepatic cholangiocarcinoma. Mol Clin Oncol 6:566–574. https://doi.org/10.3892/mco.2017.1166
Miyata T, Yamashita YI, Higashi T, Taki K, Izumi D, Kosumi K, Tokunaga R, Nakagawa S, Okabe H, Imai K, Hashimoto D, Chikamoto A, Baba H (2018) The prognostic impact of controlling nutritional status (CONUT) in intrahepatic cholangiocarcinoma following curative hepatectomy: A retrospective single institution study. World J Surg 42:1085–1091. https://doi.org/10.1007/s00268-017-4214-1
Dutta S, Horgan PG, McMillan DC (2010) POSSUM and its related models as predictors of postoperative mortality and morbidity in patients undergoing surgery for gastro-oesophageal cancer: a systematic review. World J Surg 34:2076–2082. https://doi.org/10.1007/s00268-010-0685-z
Richards CH, Leitch FE, Horgan PG, McMillan DC (2010) A systematic review of POSSUM and its related models as predictors of post-operative mortality and morbidity in patients undergoing surgery for colorectal cancer. J Gastrointest Surg 14:1511–1520. https://doi.org/10.1007/s11605-010-1333-5
Haga Y, Miyamoto A, Wada Y, Takami Y, Takeuchi H (2016) Value of E-PASS models for predicting postoperative morbidity and mortality in resection of perihilar cholangiocarcinoma and gallbladder carcinoma. HPB (Oxford) 18:271–278. https://doi.org/10.1016/j.hpb.2015.09.001
Coelen RJ, Olthof PB, van Dieren S, Besselink MGH, Busch ORC, van Gulik TM (2016) External validation of the estimation of physiologic ability and surgical stress (E-PASS) risk model to predict operative risk in perihilar cholangiocarcinoma. JAMA Surg 151:1132–1138. https://doi.org/10.1001/jamasurg.2016.2305
Visser A, Geboers B, Gouma DJ, Goslings JC, Ubbink DT (2015) Predictors of surgical complications: a systematic review. Surgery 158:58–65. https://doi.org/10.1016/j.surg.2015.01.012
Dasari BVM, Hodson J, Sutcliffe RP, Marudanayagam R, Roberts KJ, Abradelo M, Muiesan P, Mirza DF, Isaac J (2019) Developing and validating a preoperative risk score to predict 90-day mortality after liver resection. J Surg Oncol 119:472–478. https://doi.org/10.1002/jso.25350
Wiggers JK, Groot Koerkamp B, Cieslak KP, Doussot A, van Klaveren D, Allen PJ, Besselink MG, Busch OR, D’Angelica MI, DeMatteo RP, Gouma DJ, Kingham TP, van Gulik TM, Jarnagin WR (2016) Postoperative mortality after liver resection for perihilar cholangiocarcinoma: development of a risk score and importance of biliary drainage of the future liver remnant. J Am Coll Surg 223:321-331.e1. https://doi.org/10.1016/j.jamcollsurg.2016.03.035
Kuriyama N, Komatsubara H, Nakagawa Y, Maeda K, Shinkai T, Noguchi D, Ito T, Gyoten K, Hayasaki A, Fujii T, Iizawa Y, Murata Y, Tanemura A, Kishiwada M, Sakurai H, Mizuno S (2021) Impact of combined vascular resection and reconstruction in patients with advanced perihilar cholangiocarcinoma. J Gastrointest Surg 25:3108–3118. https://doi.org/10.1007/s11605-021-05004-2
Yokoyama Y, Nishio H, Ebata T, Igami T, Sugawara G, Nagino M (2010) Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 97:1260–1268. https://doi.org/10.1002/bjs.7084
Otsubo T, Kobayashi S, Sano K, Misawa T, Ota T, Katagiri S, Yanaga K, Yamaue H, Kokudo N, Unno M, Fujimoto J, Miura F, Miyazaki M, Yamamoto M (2017) Safety-related outcomes of the Japanese Society of Hepato-Biliary-Pancreatic Surgery board certification system for expert surgeons. J Hepatobiliary Pancreat Sci 24:252–261. https://doi.org/10.1002/jhbp.444
Ueno K, Ajiki T, Tsugawa D, Akita M, Hashimoto Y, Awazu M, Mukubo H, Komatsu S, Kuramitsu K, Terai S, Tanaka M, Toyama H, Kido M, Fukumoto T (2019) Effectiveness of omega-3 fatty acid administration on completion rate of adjuvant chemotherapy for biliary tract cancer: study protocol for a single-centre, open-label, single-arm, historically controlled study. BMJ Open 9(8):e029915. https://doi.org/10.1136/bmjopen-2019-029915
Akashi K, Ebata T, Mizuno T, Yokoyama Y, Igami T, Yamaguchi J, Onoe S, Nagino M (2018) Surgery for perihilar cholangiocarcinoma from a viewpoint of age: is it beneficial to octogenarians in an aging society? Surgery 164:1023–1029. https://doi.org/10.1016/j.surg.2018.05.051
Yasukawa K, Shimizu A, Kubota K, Notake T, Sugenoya S, Hosoda K, Ikehara T, Hayashi H, Kobayashi R, Soejima Y (2021) The survival benefit of surgery for perihilar cholangiocarcinoma in octogenarians: Shinshu University experience. J Surg Oncol 124:67–78. https://doi.org/10.1002/jso.26488
Yu X, Yan YC, Chen G, Yu H (2018) The efficacy and safety of totally laparoscopic hepatectomy for non-cirrhotic hepatocellular carcinoma in the elderly. BMC Surg 18:118. https://doi.org/10.1186/s12893-018-0444-x
Schiergens TS, Stielow C, Schreiber S, Hornuss C, Jauch KW, Rentsch M, Thasler WE (2014) Liver resection in the elderly: significance of comorbidities and blood loss. J Gastrointest Surg 18:1161–1170. https://doi.org/10.1007/s11605-014-2516-2
Yeh CN, Jan YY, Chen MF (2006) Hepatectomy for peripheral cholangiocarcinoma in elderly patients. Ann Surg Oncol 13:1553–1559. https://doi.org/10.1245/s10434-006-9085-x
Wabitsch S, Haber PK, Ekwelle N, Kästner A, Krenzien F, Benzing C, Atanasov G, Bellingrath JS, Bauer G, Schöning W, Öllinger R, Pratschke J, Schmelzle M (2019) Minimally invasive liver surgery in elderly patients—a single-center experience. J Surg Res 239:92–97. https://doi.org/10.1016/j.jss.2019.01.058
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B (2015) Laparoscopic major hepatectomy for colorectal liver metastases in elderly patients: a single-center, case-matched study. Surg Endosc 29:1368–1375. https://doi.org/10.1007/s00464-014-3806-1
Goh BKP, Chua D, Syn N, Teo JY, Chan CY, Lee SY, Jeyaraj PR, Cheow PC, Chow PKH, Ooi LLPJ, Chung AYF (2018) Perioperative outcomes of laparoscopic minor hepatectomy for hepatocellular carcinoma in the elderly. World J Surg 42:4063–4069. https://doi.org/10.1007/s00268-018-4741-4
Notarnicola M, Felli E, Roselli S, Altomare DF, De Fazio M, de’Angelis N, Piardi T, Acquafredda S, Ammendola M, Verbo A, Pessaux P, Memeo R (2019) Laparoscopic liver resection in elderly patients: systematic review and meta-analysis. Surg Endosc 33:2763–2773. https://doi.org/10.1007/s00464-019-06840-9
Lallement M, Maulat C, Suc B, Péré G, Lozano S, Bérard E, Muscari F (2020) Short-term autonomy and survival after hepatectomy in the elderly. J Visc Surg 157:378–386. https://doi.org/10.1016/j.jviscsurg.2020.01.001
Takahashi Y, Ebata T, Yokoyama Y, Igami T, Sugawara G, Nagino M (2013) Surgical treatment of perihilar cholangiocarcinoma in octogenarians: a single center experience. J Hepatobiliary Pancreat Sci 20:324–331. https://doi.org/10.1007/s00534-012-0529-3
Vitale A, Spolverato G, Bagante F, Gani F, Popescu I, Marques HP, Aldrighetti L, Gamblin TC, Maithel SK, Sandroussi C, Bauer TW, Shen F, Poultsides GA, Marsh JW, Pawlik TM (2016) A multi-institutional analysis of elderly patients undergoing a liver resection for intrahepatic cholangiocarcinoma. J Surg Oncol 113:420–426. https://doi.org/10.1002/jso.24148
Watanabe Y, Kuboki S, Shimizu H, Ohtsuka M, Yoshitomi H, Furukawa K, Miyazaki M (2018) A new proposal of criteria for the future remnant liver volume in older patients undergoing major hepatectomy for biliary tract cancer. Ann Surg 267:338–345. https://doi.org/10.1097/SLA.0000000000002080
Kawakatsu S, Ebata T, Watanabe N, Onoe S, Yamaguchi J, Mizuno T, Igami T, Yokoyama Y, Matsuo K, Nagino M (2020) Mild prognostic impact of postoperative complications on long-term survival of perihilar cholangiocarcinoma. Ann Surg. https://doi.org/10.1097/SLA.0000000000004465 (Published online ahead of print)
Franken LC, Schreuder AM, Roos E, van Dieren S, Busch OR, Besselink MG, van Gulik TM (2019) Morbidity and mortality after major liver resection in patients with perihilar cholangiocarcinoma: a systematic review and meta-analysis. Surgery 165:918–928. https://doi.org/10.1016/j.surg.2019.01.010
Giuliante F, Ardito F, Aldrighetti L, Ferrero A, Pinna AD, DeCarlis L, Cillo U, Jovine E, Portolani N, Gruttadauria S, Mazzaferro V, Massani M, Rosso E, Ettorre GM, Ratti F, Guglielmi A, Italian Association of HepatoBilioPancreatic Surgeons-AICEP, Italian Association of Hepato-Biliary-Pancreatic Surgeons-AICEP, Cescon M, Colasanti M, Di Sandro S, Gringeri E, Russolillo N, Ruzzenente A, Sposito C, Zanello M, Zimmitti G (2021) Liver resection for perihilar cholangiocarcinoma: Impact of biliary drainage failure on postoperative outcome. Results of an Italian multicenter study. Surgery 170:383–389. https://doi.org/10.1016/j.surg.2021.01.021
Olthof PB, Wiggers JK, Groot Koerkamp B, Coelen RJ, Allen PJ, Besselink MG, Busch OR, D’Angelica MI, DeMatteo RP, Kingham TP, van Lienden KP, Jarnagin WR, van Gulik TM (2017) Postoperative liver failure risk score: identifying patients with resectable perihilar cholangiocarcinoma who can benefit from portal vein embolization. J Am Coll Surg 225:387–394. https://doi.org/10.1016/j.jamcollsurg.2017.06.007
Lee JW, Lee JH, Park Y, Lee W, Kwon J, Song KB, Hwang DW, Kim SC (2020) Risk factors of posthepatectomy liver failure for perihilar cholangiocarcinoma: risk score and significance of future liver remnant volume-to-body weight ratio. J Surg Oncol 122:469–479. https://doi.org/10.1002/jso.25974
Efanov M, Alikhanov R, Zamanov E, Melekhina O, Kulezneva Y, Kazakov I, Vankovich A, Koroleva A, Tsvirkun V (2021) Combining E-PASS model and disease specific risk factors to predict severe morbidity after liver and bile duct resection for perihilar cholangiocarcinoma. HPB (Oxford) 23:387–393. https://doi.org/10.1016/j.hpb.2020.07.009
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing and Dr. Toru Ogura (Clinical Research Support Center, Mie University Hospital) for statistical support.
Author information
Authors and Affiliations
Contributions
Study conception and design: KM and NK. Acquisition of data: TI, KG, AH, TF, YI, YM, AT, and MK. Analysis and interpretation of data: KM. Drafting of manuscript: KM and NK. Critical revision of manuscript: SM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Completing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maeda, K., Kuriyama, N., Ito, T. et al. Safety and benefits of major hepatectomy with extrahepatic bile duct resection in older perihilar cholangiocarcinoma patients. Langenbecks Arch Surg 407, 2861–2872 (2022). https://doi.org/10.1007/s00423-022-02654-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02654-x