Abstract
Purpose
Pancreatic malignancy with mesenterico-portal venous involvement can be safely managed with en bloc vein resection with comparable survival outcomes. Non-constructible venous encasement is regarded as criteria of unresectability in pancreatic cancer. In long-standing extra-hepatic venous obstruction, hepatopetal blood flow is established by collateralization in the hepatoduodenal and mesenteric region. Their importance in pancreatic malignancies is being recently acknowledged.
Methods
The records of patients undergoing pancreatoduodenectomies were retrospectively evaluated from 2012 to 2019. Pre and intraoperative records of patients undergoing concomitant vein resection were evaluated for the presence of venous collaterals, and its impact on oncological management was studied.
Results
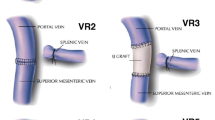
Over a period of 7 years, 947 pancreatoduodenectomies were performed, of which 56 patients underwent concomitant vein resection. Among these, six patients had significant collaterals due to venous obstruction. They had pancreatic adenocarcinoma (2), neuroendocrine tumour (2) and solid pseudopapillary epithelial neoplasm (2) respectively. All these patients successfully underwent pancreatoduodenectomy with vein resection without vascular reconstruction. Superior mesenteric vein (SMV) was resected in four patients, whereas spleno-portal junction was resected in two patients. Dominant collaterals were preserved in all, without compromising oncological safety. Bowel congestion was checked by tolerability to 20-minute mesenteric venous clamping test. There was no major morbidity or hospital mortality following this surgical approach.
Conclusion
We recommend vein resection without reconstruction (VROR) as a novel approach in locally advanced pancreatic tumours (due to non-constructible vein involvement) with significant venous collaterals and emphasize the need to assess venous collateralization pre and intraoperatively.



Similar content being viewed by others
Data availability
The data is represented in the manuscript in tables.
Abbreviations
- CD grade:
-
Clavien-Dindo grade
- CT:
-
Computed tomography
- DGE:
-
Delayed gastric emptying
- ERAS:
-
Enhanced recovery after surgery
- IMV:
-
Inferior mesenteric vein
- ISGPS:
-
International Study Group for Pancreatic Surgery
- LGV:
-
Left gastric vein.
- MDT:
-
Multidisciplinary team
- mFOLFIRINOX:
-
Modified FOLFIRINOX regimen
- NET:
-
Neuroendocrine tumour
- PDAC:
-
Pancreatic ductal adenocarcinoma
- NCCN:
-
National Comprehensive Cancer Network
- PD:
-
Pancreatoduodenectomy
- POPF:
-
Post-operative pancreatic fistula
- PV:
-
Portal vein
- SMA:
-
Superior mesenteric artery
- SMV:
-
Superior mesenteric vein
- SPEN:
-
Solid pseudopapillary epithelial neoplasm
- SSI:
-
Surgical site infection
- SV:
-
Splenic vein
- VROR:
-
Vein resection without reconstruction
- N:
-
Number of cases
- N/A:
-
Data not available
References
Kelly K, Winslow E, Kooby D, Lad N, Parikh A, Scoggins C, Ahmad S, Martin R, Maithel S, Kim H, Merchant N, Cho C, Weber S (2013) Vein involvement during pancreaticoduodenectomy: is there a need for redefinition of “borderline resectable disease”? J Gastrointest Surg 17:1209–1217
Nakagohri T, Kinoshita T, Konishi M, Inoue K, Takahashi S (2003) Survival benefits of portal vein resection for pancreatic cancer. Am J Surg 186:149–153
Bockhorn M, Uzunoglu F, Adham M, Imrie C, Milicevic M, Sandberg A, Asbun H, Bassi C, Büchler M, Charnley R, Conlon K, Cruz L, Dervenis C, Fingerhutt A, Friess H, Gouma D, Hartwig W, Lillemoe K, Montorsi M, Neoptolemos J, Shrikhande S, Takaori K, Traverso W, Vashist Y, Vollmer C, Yeo C, Izbicki J, International Study Group of Pancreatic Surgery (2014) Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 155:977–988
Khanna R, Sarin S (2014) Non-cirrhotic portal hypertension – diagnosis and management. J Hepatol 60:421–441
Gage M, Reames B, Ejaz A, Sham J, Fishman E, Weiss M, Wolfgang C, He J (2018) Pancreaticoduodenectomy with en bloc vein resection for locally advanced pancreatic cancer: a case series without venous reconstruction. Chin Clin Oncol 7:7
Jouffret L, Guilbaud T, Turrini O, Delpero J (2018) Pancreaticoduodenectomy with combined superior mesenteric vein resection without reconstruction is possible: a case report and review of the literature. World J Clin Cases 6:214–218
Maley W, Yeo C (2017) Vascular resections during the Whipple procedure. Adv Surg 51:41–63
Hashimoto M, Makuuchi M, Matsuda M, Watanabe G (2010) Superior mesenteric vein resection without reconstruction in pylorus-preserving pancreatoduodenectomy for pancreatic head cancer. Hepatogastroenterology 57:1087–1089
Tsuchikawa T, Kondo S, Hirano S, Tanaka E, Kawasaki R, Kato K, Matsumoto J, Shichinohe T (2011) Distal pancreatectomy and portal vein resection without vascular reconstruction for endocrine tumors with massive intraportal growth: report of a case. Hepatogastroenterology 58:1029–1031
Shrikhande S, Shinde R, Chaudhari V, Kurunkar S, Desouza A, Agarwal V, Bhandare M (2019) Twelve hundred consecutive pancreato-duodenectomies from single centre: impact of centre of excellence on pancreatic cancer surgery across India. World J Surg 44:2784–2793. https://doi.org/10.1007/s00268-019-05235-0
Kumar N, Bhandare M, Chaudhari V, Sasi S, Shrikhande S (2019) Analysis of 50 cases of solid pseudopapillary tumor of pancreas: aggressive surgical resection provides excellent outcomes. Eur J Surg Oncol 45:187–191
Sanjay P, Takaori K, Govil S, Shrikhande S (2012) “Artery first” approaches to pancreatoduodenectomy. Br J Surg 99:1027–1035
Amico E, Alves J, Joao S, Costa de Medeiros J, Sousa R (2017) Venous occlusion test applied to the tributaries of superior mesenteric veins of the pancreas head infiltrated by the tumor. J Surg Case Rep 6:1–3
Shrikhande S, Barreto G, Shukla P (2008) Pancreatic fistula after pancreaticoduodenectomy: the impact of a standardized technique of pancreaticojejunostomy. Langenbeck's Arch Surg 393:87–91
Agarwal V, Thomas M, Joshi R, Chaudhari V, Bhandare M, Mitra A, Desouza A, Ambulkar R, Shrikhande S (2018) Improved outcomes in 394 pancreatic cancer resections: the impact of enhanced recovery pathway. J Gastrointest Surg 22:1732–1742
Shrikhande S, Barreto S, Somashekar B, Suradkar K, Shetty G, Talole S, Sirohi B, Goel M, Shukla P (2013) Evolution of pancreatoduodenectomy in a tertiary cancer center in India: improved results from service reconfiguration. Pancreatology 13:63–71
Nakao A, Kanzaki A, Fujii T, Kodera Y, Yamada S, Sugimoto H, Nomoto S, Nakamura S, Morita S, Takeda S (2012) Correlation between radiographic classification and pathological grade of portal vein wall invasion in pancreatic head cancer. Ann Surg 255:103–108
Oehme F, Distler M, Müssle B, Kahlert C, Weitz J, Welsch T (2019) Results of portosystemic shunts during extended pancreatic resections. Langenbeck's Arch Surg 404:959–966
Katz M, Fleming J, Pisters P, Lee J, Evans D (2008) Anatomy of superior mesenteric vein with special reference to the surgical management of first order branch involvement at pancreatoduodenectomy. Ann Surg 248:1098–1102
Tempero M, Malafa M, Chiorean E, Czito B, Scaife C, Narang A, Fountzilas C, Wolpin B, Al-Hawary M, Asbun H, Behrman S, Benson A, Binder E, Cardin D, Cha C, Chung V, Dillhoff M, Dotan E, Ferrone C, Fisher G, Hardacre J, Hawkins W, Ko A, LoConte N, Lowy A, Moravek C, Nakakura E, O’Reilly E, Obando J, Reddy S, Thayer S, Wolff R, Burns J, Zuccarino-Catania G (2019) Pancreatic adenocarcinoma, version 1.2019. J Natl Compr Cancer Netw 17:202–210
Author information
Authors and Affiliations
Contributions
Acquisition, analysis and interpretation of data, drafting of the article, critical revision for the intellectual content and final approval of the version to be submitted: RVK and VP. (both are shared first authors). Analysis and interpretation of data, drafting and revision of the article, critical revision for the intellectual content and final approval of the version to be submitted: MSB and VAC. Conception and design of the study, drafting and revision of the article, critical revision for intellectual content and final approval of the version to be submitted: SVS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The study data was collected in the course of common clinical practice, and accordingly, written informed consent was obtained from the patients before the surgical procedure. All procedures performed in the study were in accordance with the ethical standards of the institutional research committee. The protocol conformed to the “World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human subjects” adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, as revised in Brazil 2013. In order to protect the patient information, HIPAA (Health Insurance Portability and Accountability Act) compliance was also ensured throughout the study. There was no requirement of any formal ethical approval as the data was collected in the course of common clinical practice, in retrospective manner.
Consent to participate
Written informed consent was obtained from all the individual participants included in the study.
Consent for publication
All the individual participants signed an informed consent regarding publishing their clinical details and/or clinical images in research study.
Submission declaration
The research was presented as Poster in the Indian Chapter of International Hepato-Pancreato-Biliary Association conference held at Jaipur, India, on February 15–17, 2019. This manuscript has not been published previously and is not under consideration for publication elsewhere. It has been approved by all the authors listed and by authorities where this work was carried out. This manuscript will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rugved V. Kulkarni and Vijayraj Patil are shared first authors.
Rights and permissions
About this article
Cite this article
Kulkarni, R.V., Patil, V., Bhandare, M.S. et al. Vein resection without reconstruction (VROR) in pancreatoduodenectomy: expanding the surgical spectrum for locally advanced pancreatic tumours. Langenbecks Arch Surg 405, 929–937 (2020). https://doi.org/10.1007/s00423-020-01954-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01954-4