Abstract
Purpose
While the importance of lymphadenectomy is well-established for patients with resectable pancreatic cancer, its direct impact on survival in relation to other predictive factors is still ill-defined.
Methods
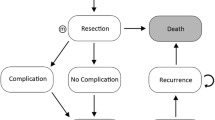
The National Cancer Data Base 2006–2015 was queried for patients with resected pancreatic adenocarcinoma (stage IA–IIB). Patients were dichotomized into the following two groups, those with 1–14 resected lymph nodes and those with ≥ 15. Optimal number of resected lymph nodes and the effect of lymphadenectomy on survival were assessed using various statistical modeling techniques. Mediation analysis was performed to differentiate the direct and indirect effect of lymph node resection on survival.
Results
A total of 21,912 patients were included; median age was 66 years (IQR 59–73), 48.9% were female. Median number of resected lymph nodes was 15 (IQR 10–22), 10,163 (46.4%) had 1–14 and 11,749 (53.6%) had ≥ 15 lymph nodes retrieved. Lymph node positivity increased by 4.1% per lymph node up to eight examined lymph nodes, and by 0.6% per lymph node above eight. Five-year overall survival was 17.9%. Overall survival was better in the ≥ 15 lymph node group (adjusted HR 0.91, CI 0.88–0.95, p < 0.001). On a continuous scale, survival improved with increasing LNs collected. Patients who underwent adjuvant chemotherapy and were treated at high-volume centers had improved overall survival compared with their counterparts (adjusted HR 0.59, CI 0.57–0.62, p < 0.001; adjusted HR 0.86, CI 0.83–0.89, p < 0.001, respectively). Mediation analysis revealed that lymphadenectomy had only 18% direct effect on improved overall survival, while 82% of its effect were mediated by other factors like treatment at high-volume hospitals and adjuvant chemotherapy.
Discussion
While higher number of resected lymph nodes increases lymph node positivity and is associated with better overall survival, most of the observed survival benefit is mediated by chemotherapy and treatment at high-volume centers.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34. https://doi.org/10.3322/caac.21551
Strobel O, Neoptolemos J, Jager D, Buchler MW (2019) Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol 16(1):11–26. https://doi.org/10.1038/s41571-018-0112-1
Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J (2010) Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med 7(4):e1000267. https://doi.org/10.1371/journal.pmed.1000267
Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, Faluyi O, O'Reilly DA, Cunningham D, Wadsley J, Darby S, Meyer T, Gillmore R, Anthoney A, Lind P, Glimelius B, Falk S, Izbicki JR, Middleton GW, Cummins S, Ross PJ, Wasan H, McDonald A, Crosby T, Ma YT, Patel K, Sherriff D, Soomal R, Borg D, Sothi S, Hammel P, Hackert T, Jackson R, Buchler MW, European Study Group for Pancreatic C (2017) Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet 389(10073):1011–1024. https://doi.org/10.1016/S0140-6736(16)32409-6
Uesaka K, Boku N, Fukutomi A, Okamura Y, Konishi M, Matsumoto I, Kaneoka Y, Shimizu Y, Nakamori S, Sakamoto H, Morinaga S, Kainuma O, Imai K, Sata N, Hishinuma S, Ojima H, Yamaguchi R, Hirano S, Sudo T, Ohashi Y, Group JS (2016) Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 388(10041):248–257. https://doi.org/10.1016/S0140-6736(16)30583-9
Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul JL, Chone L, Francois E, Artru P, Biagi JJ, Lecomte T, Assenat E, Faroux R, Ychou M, Volet J, Sauvanet A, Breysacher G, Di Fiore F, Cripps C, Kavan P, Texereau P, Bouhier-Leporrier K, Khemissa-Akouz F, Legoux JL, Juzyna B, Gourgou S, O'Callaghan CJ, Jouffroy-Zeller C, Rat P, Malka D, Castan F, Bachet JB, Canadian Cancer Trials G, the Unicancer GIPG (2018) FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med 379(25):2395–2406. https://doi.org/10.1056/NEJMoa1809775
Hartwig W, Hackert T, Hinz U, Gluth A, Bergmann F, Strobel O, Buchler MW, Werner J (2011) Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg 254(2):311–319. https://doi.org/10.1097/SLA.0b013e31821fd334
Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Yu HC, Kang KJ, Kim SG, Kim SW (2014) A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg 259(4):656–664. https://doi.org/10.1097/SLA.0000000000000384
Nimura Y, Nagino M, Takao S, Takada T, Miyazaki K, Kawarada Y, Miyagawa S, Yamaguchi A, Ishiyama S, Takeda Y, Sakoda K, Kinoshita T, Yasui K, Shimada H, Katoh H (2012) Standard versus extended lymphadenectomy in radical pancreatoduodenectomy for ductal adenocarcinoma of the head of the pancreas: long-term results of a Japanese multicenter randomized controlled trial. J Hepatobiliary Pancreat Sci 19(3):230–241. https://doi.org/10.1007/s00534-011-0466-6
Farnell MB, Pearson RK, Sarr MG, DiMagno EP, Burgart LJ, Dahl TR, Foster N, Sargent DJ, Pancreas Cancer Working G (2005) A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery 138(4):618–628; discussion 628-630. https://doi.org/10.1016/j.surg.2005.06.044
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, Coleman J, Abrams RA, Hruban RH (2002) Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg 236(3):355–366; discussion 366-358. https://doi.org/10.1097/00000658-200209000-00012
Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C, Kloppel G, Dhaene K, Michelassi F (1998) Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy study group. Ann Surg 228(4):508–517. https://doi.org/10.1097/00000658-199810000-00007
Niesen W, Hank T, Buchler M, Strobel O (2019) Local radicality and survival outcome of pancreatic cancer surgery. Ann Gastroenterol Surg 3(5):464–475. https://doi.org/10.1002/ags3.12273
Warschkow R, Widmann B, Beutner U, Marti L, Steffen T, Schiesser M, Schmied BM (2017) The more the better-lower rate of stage migration and better survival in patients with retrieval of 20 or more regional lymph nodes in pancreatic cancer: a population-based propensity score matched and trend SEER analysis. Pancreas 46(5):648–657. https://doi.org/10.1097/MPA.0000000000000784
Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, Andren-Sandberg A, Asbun HJ, Bockhorn M, Buchler MW, Conlon KC, Fernandez-Cruz L, Fingerhut A, Friess H, Hartwig W, Izbicki JR, Lillemoe KD, Milicevic MN, Neoptolemos JP, Shrikhande SV, Vollmer CM, Yeo CJ, Charnley RM, International Study Group on Pancreatic S (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156(3):591–600. https://doi.org/10.1016/j.surg.2014.06.016
Schwarz RE, Smith DD (2006) Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol 13(9):1189–1200. https://doi.org/10.1245/s10434-006-9016-x
Huebner M, Kendrick M, Reid-Lombardo KM, Que F, Therneau T, Qin R, Donohue J, Nagorney D, Farnell M, Sarr M (2012) Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg 16(5):920–926. https://doi.org/10.1007/s11605-012-1853-2
Vuarnesson H, Lupinacci RM, Semoun O, Svrcek M, Julie C, Balladur P, Penna C, Bachet JB, Resche-Rigon M, Paye F (2013) Number of examined lymph nodes and nodal status assessment in pancreaticoduodenectomy for pancreatic adenocarcinoma. Eur J Surg Oncol 39(10):1116–1121. https://doi.org/10.1016/j.ejso.2013.07.089
Tomlinson JS, Jain S, Bentrem DJ, Sekeris EG, Maggard MA, Hines OJ, Reber HA, Ko CY (2007) Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg 142(8):767–723; discussion 773-764. https://doi.org/10.1001/archsurg.142.8.767
Contreras CM, Lin CP, Oster RA, Reddy S, Wang T, Vickers S, Heslin M (2017) Increased pancreatic cancer survival with greater lymph node retrieval in the National Cancer Data Base. Am J Surg 214(3):442–449. https://doi.org/10.1016/j.amjsurg.2017.06.036
MacKinnon DP, Fairchild AJ, Fritz MS (2007) Mediation analysis. Annu Rev Psychol 58:593–614. https://doi.org/10.1146/annurev.psych.58.110405.085542
Rochon J, du Bois A, Lange T (2014) Mediation analysis of the relationship between institutional research activity and patient survival. BMC Med Res Methodol 14:9. https://doi.org/10.1186/1471-2288-14-9
Yu Q, Wu X, Li B, Scribner RA (2019) Multiple mediation analysis with survival outcomes: with an application to explore racial disparity in breast cancer survival. Stat Med 38(3):398–412. https://doi.org/10.1002/sim.7977
Fan X (2013) General multiple mediation analysis with an application to explore racial disparities in breast cancer survival. J Biom Biostat 05. https://doi.org/10.4172/2155-6180.1000189
Yu Q, Medeiros KL, Wu X, Jensen RE (2018) Nonlinear predictive models for multiple mediation analysis: with an application to explore ethnic disparities in anxiety and depression among cancer survivors. Psychometrika 83(4):991–1006. https://doi.org/10.1007/s11336-018-9612-2
American College of Surgeons (2019) National Cancer Database. https://www.facs.org/quality-programs/cancer/ncdb. Accessed Nov 2019
Kagedan DJ, Goyert N, Li Q, Paszat L, Kiss A, Earle CC, Karanicolas PJ, Wei AC, Mittmann N, Coburn NG (2017) The impact of increasing hospital volume on 90-day postoperative outcomes following pancreaticoduodenectomy. J Gastrointest Surg 21(3):506–515. https://doi.org/10.1007/s11605-016-3346-1
van der Geest LG, Besselink MG, Busch OR, de Hingh IH, van Eijck CH, Dejong CH, Lemmens VE (2016) Elderly patients strongly benefit from centralization of pancreatic cancer surgery: a population-based study. Ann Surg Oncol 23(6):2002–2009. https://doi.org/10.1245/s10434-016-5089-3
Szumilas M (2010) Explaining odds ratios. J Can Acad Child Adolesc Psychiatry 19(3):227–229
Case LD, Kimmick G, Paskett ED, Lohman K, Tucker R (2002) Interpreting measures of treatment effect in cancer clinical trials. Oncologist 7(3):181–187. https://doi.org/10.1634/theoncologist.7-3-181
Angrist JD, Imbens GW, Rubin DB (1996) Identification of causal effects using instrumental variables. J Am Stat Assoc vol 91:444–455
Holland PW (1988) Causal inference, path analysis, and recursive structural equations models. Sociol Methodol 18:449
Muggeo VM (2003) Estimating regression models with unknown break-points. Stat Med 22(19):3055–3071. https://doi.org/10.1002/sim.1545
Cleveland WS (1979) Robust locally weighted regression and smoothing scatterplots. J am stat Assoc 74:829–836
Kang MJ, Jang JY, Kim SW (2016) Surgical resection of pancreatic head cancer: what is the optimal extent of surgery? Cancer Lett 382(2):259–265. https://doi.org/10.1016/j.canlet.2016.01.042
Jang JY, Kang JS, Han Y, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Park JS, Yu HC, Kang KJ, Kim SG, Lee H, Kwon W, Yoon YS, Han HS, Kim SW (2017) Long-term outcomes and recurrence patterns of standard versus extended pancreatectomy for pancreatic head cancer: a multicenter prospective randomized controlled study. J Hepatobiliary Pancreat Sci 24(7):426–433. https://doi.org/10.1002/jhbp.465
Basturk O, Saka B, Balci S, Postlewait LM, Knight J, Goodman M, Kooby D, Sarmiento JM, El-Rayes B, Choi H, Bagci P, Krasinskas A, Quigley B, Reid MD, Akkas G, Maithel SK, Adsay V (2015) Substaging of lymph node status in resected pancreatic ductal adenocarcinoma has strong prognostic correlations: proposal for a revised N classification for TNM staging. Ann Surg Oncol 22(Suppl 3):S1187–S1195. https://doi.org/10.1245/s10434-015-4861-0
Malleo G, Maggino L, Capelli P, Gulino F, Segattini S, Scarpa A, Bassi C, Butturini G, Salvia R (2015) Reappraisal of nodal staging and study of lymph node station involvement in pancreaticoduodenectomy with the Standard International Study Group of Pancreatic Surgery definition of lymphadenectomy for cancer. J Am Coll Surg 221(2):367–379 e364. https://doi.org/10.1016/j.jamcollsurg.2015.02.019
Strobel O, Hinz U, Gluth A, Hank T, Hackert T, Bergmann F, Werner J, Buchler MW (2015) Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg 261(5):961–969. https://doi.org/10.1097/SLA.0000000000000814
Murakami Y (2010) Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg vol 211
Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, Niedergethmann M, Zulke C, Fahlke J, Arning MB, Sinn M, Hinke A, Riess H (2013) Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA 310(14):1473–1481. https://doi.org/10.1001/jama.2013.279201
Neoptolemos JP, Stocken DD, Bassi C, Ghaneh P, Cunningham D, Goldstein D, Padbury R, Moore MJ, Gallinger S, Mariette C, Wente MN, Izbicki JR, Friess H, Lerch MM, Dervenis C, Olah A, Butturini G, Doi R, Lind PA, Smith D, Valle JW, Palmer DH, Buckels JA, Thompson J, McKay CJ, Rawcliffe CL, Buchler MW, European Study Group for Pancreatic C (2010) Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA 304(10):1073–1081. https://doi.org/10.1001/jama.2010.1275
Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine F, Falconi M, Pederzoli P, Pap A, Spooner D, Kerr DJ, Buchler MW, European Study Group for Pancreatic C (2004) A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N Engl J Med 350(12):1200–1210. https://doi.org/10.1056/NEJMoa032295
Tempero MA, Reni M, Riess H, Pelzer U, O'Reilly EM, Winter JM, Oh D-Y, Li C-P, Tortora G, Chang H-M, Lopez CD, Tabernero J, Cutsem EV, Philip PA, Goldstein D, Berlin J, Ferrara S, Li M, Lu BD, Biankin A (2019) APACT: phase III, multicenter, international, open-label, randomized trial of adjuvant nab-paclitaxel plus gemcitabine (nab-P/G) vs gemcitabine (G) for surgically resected pancreatic adenocarcinoma. J Clin Oncol 37(15_suppl):4000. https://doi.org/10.1200/JCO.2019.37.15_suppl.4000
Neoptolemos JP, Dunn JA, Stocken DD, Almond J, Link K, Beger H, Bassi C, Falconi M, Pederzoli P, Dervenis C, Fernandez-Cruz L, Lacaine F, Pap A, Spooner D, Kerr DJ, Friess H, Buchler MW, European Study Group for Pancreatic C (2001) Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet 358(9293):1576–1585. https://doi.org/10.1016/s0140-6736(01)06651-x
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137. https://doi.org/10.1056/NEJMsa012337
Mamidanna R, Ni Z, Anderson O, Spiegelhalter SD, Bottle A, Aylin P, Faiz O, Hanna GB (2016) Surgeon volume and cancer esophagectomy, gastrectomy, and pancreatectomy: a population-based study in England. Ann Surg 263(4):727–732. https://doi.org/10.1097/SLA.0000000000001490
Guller U, Warschkow R, Ackermann CJ, Schmied B, Cerny T, Ess S (2017) Lower hospital volume is associated with higher mortality after oesophageal, gastric, pancreatic and rectal cancer resection. Swiss Med Wkly 147:w14473. https://doi.org/10.4414/smw.2017.14473
Bilimoria KY, Talamonti MS, Wayne JD, Tomlinson JS, Stewart AK, Winchester DP, Ko CY, Bentrem DJ (2008) Effect of hospital type and volume on lymph node evaluation for gastric and pancreatic cancer. Arch Surg 143(7):671–678; discussion 678. https://doi.org/10.1001/archsurg.143.7.671
Bilimoria KY, Talamonti MS, Sener SF, Bilimoria MM, Stewart AK, Winchester DP, Ko CY, Bentrem DJ (2008) Effect of hospital volume on margin status after pancreaticoduodenectomy for cancer. J Am Coll Surg 207(4):510–519. https://doi.org/10.1016/j.jamcollsurg.2008.04.033
La Torre M, Cavallini M, Ramacciato G, Cosenza G, Rossi Del Monte S, Nigri G, Ferri M, Mercantini P, Ziparo V (2011) Role of the lymph node ratio in pancreatic ductal adenocarcinoma. Impact on patient stratification and prognosis. J Surg Oncol 104(6):629–633. https://doi.org/10.1002/jso.22013
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K, Kehlet H, Reynolds JV, Kaser SA, Naredi P, Borel-Rinkes I, Biondo S, Pinto-Marques H, Gnant M, Nafteux P, Ryska M, Bechstein WO, Martel G, Dimick JB, Krawczyk M, Olah A, Pinna AD, Popescu I, Puolakkainen PA, Sotiropoulos GC, Tukiainen EJ, Petrowsky H, Clavien PA (2018) Toward a consensus on centralization in surgery. Ann Surg 268(5):712–724. https://doi.org/10.1097/SLA.0000000000002965
de Wilde RF, Besselink MG, van der Tweel I, de Hingh IH, van Eijck CH, Dejong CH, Porte RJ, Gouma DJ, Busch OR, Molenaar IQ, Dutch Pancreatic Cancer G (2012) Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg 99(3):404–410. https://doi.org/10.1002/bjs.8664
Acknowledgments
We thank the American College of Surgeons and the American Cancer Society for providing patient information through the NCDB used for this investigation. Furthermore, we thank the patients whose information through the NCDB allowed us to perform the investigation for this manuscript. RW holds a masters’ degree in biostatistics from the University of Heidelberg, Germany.
Funding
This study was in part supported by the Swiss Cancer Foundation.
Author information
Authors and Affiliations
Contributions
R.W, C.T, and M.W. participated in the conceptualization of the study; R.W. and M.W. worked on the methodology; R.W. participated in formal analysis and investigation; R.W, C.T, and M.W. participated in the writing of the original draft; S.E, N. K, B.S, D.N, B.G, and S.A.M reviewed and edited the manuscript; D.N, D.B, and M.W. provided the resources; and B.S, B.G, S.A.M, and D.B. were the ones who supervised.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective cohort study was approved by the Duke Institutional Review Board. This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was in part presented as a poster at the International Hepato-Pancreato-Biliary Association Conference in Geneva, Switzerland on September 4–7, 2018.
Rights and permissions
About this article
Cite this article
Warschkow, R., Tsai, C., Köhn, N. et al. Role of lymphadenectomy, adjuvant chemotherapy, and treatment at high-volume centers in patients with resected pancreatic cancer—a distinct view on lymph node yield. Langenbecks Arch Surg 405, 43–54 (2020). https://doi.org/10.1007/s00423-020-01859-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01859-2