Abstract
Purpose
Esophagectomy for esophageal cancer is a very invasive surgery that induces an intense systemic inflammatory response. Postoperative infectious complications worsen survival after esophagectomy through inflammatory responses, and this study aimed to investigate the impact of the response on disease recurrence.
Methods
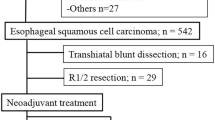
We assessed 230 patients who underwent curative minimally invasive esophagectomy for esophageal squamous cell carcinoma. The area under the curve of serum C-reactive protein levels from preoperative day through postoperative day 7 was defined as the cumulative magnitude of postoperative inflammatory response.
Results
Relapse-free survival was compared among quartiles of the area, and fourth quartile showed the worst relapse-free survival. Patients in the fourth quartile were the high group, and others were low group. Compared with low group (n = 173), high group (n = 57) showed significantly worse relapse-free survival and overall survival (P = 0.014 and 0.028, respectively). Multivariate analyses found that high group (P = 0.048) was an independent risk factor for recurrence but not overall survival. Higher body mass index (P < 0.001) and postoperative infections (P < 0.001) were independent risk factors to become high group. However, the influence of high group on recurrence was not affected by postoperative infections in interaction analysis (P = 0.889).
Conclusions
Postoperative intense systemic inflammatory response independently increased the risk of recurrence after curative minimally invasive esophagectomy for esophageal squamous cell carcinoma. Factors associating with intensified inflammatory response are higher body mass index and postoperative infections. Therefore, surgeons should make every effort to prevent postoperative infections to improve the long-term outcomes of patients.



Similar content being viewed by others
References
Okamura A, Takeuchi H, Matsuda S, Ogura M, Miyasho T, Nakamura R, Takahashi T, Wada N, Kawakubo H, Saikawa Y, Kitagawa Y (2015) Factors affecting cytokine change after esophagectomy for esophageal cancer. Ann Surg Oncol 22:3130–3135
Takeuchi H, Saikawa Y, Oyama T, Ozawa S, Suda K, Wada N, Takahashi T, Nakamura R, Shigematsu N, Ando N, Kitajima M, Kitagawa Y (2010) Factors influencing the long-term survival in patients with esophageal cancer who underwent esophagectomy after chemoradiotherapy. World J Surg 34:277–284
Booka E, Takeuchi H, Nishi T, Matsuda S, Kaburagi T, Fukuda K, Nakamura R, Takahashi T, Wada N, Kawakubo H, Omori T, Kitagawa Y (2015) The impact of postoperative complications on survivals after esophagectomy for esophageal cancer. Medicine 94:e1369
Markar S, Gronnier C, Duhamel A, Mabrut JY, Bail JP, Carrere N, Lefevre JH, Brigand C, Vaillant JC, Adham M, Msika S, Demartines N, Nakadi IE, Meunier B, Collet D, Mariette C (2015) The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg 262:972–980
Baba Y, Yoshida N, Shigaki H, Iwatsuki M, Miyamoto Y, Sakamoto Y, Watanabe M, Baba H (2016) Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg 264:305–311
Yamashita K, Makino T, Miyata H, Miyazaki Y, Takahashi T, Kurokawa Y, Yamasaki M, Nakajima K, Takiguchi S, Mori M, Doki Y (2016) Postoperative infectious complications are associated with adverse oncologic outcomes in esophageal cancer patients undergoing preoperative chemotherapy. Ann Surg Oncol 23:2106–2114
Kataoka K, Takeuchi H, Mizusawa J, Igaki H, Ozawa S, Abe T, Nakamura K, Kato K, Ando N, Kitagawa Y (2017) Prognostic impact of postoperative morbidity after esophagectomy for esophageal cancer: exploratory analysis of JCOG9907. Ann Surg 265:1152–1157
Saeki H, Tsutsumi S, Tajiri H, Yukaya T, Tsutsumi R, Nishimura S, Nakaji Y, Kudou K, Akiyama S, Kasagi Y, Nakanishi R, Nakashima Y, Sugiyama M, Ohgaki K, Sonoda H, Oki E, Maehara Y (2017) Prognostic significance of postoperative complications after curative resection for patients with esophageal squamous cell carcinoma. Ann Surg 265:527–533
Hayami M, Watanabe M, Ishizuka N, Mine S, Imamura Y, Okamura A, Kurogochi T, Yamashita K (2018) Prognostic impact of postoperative pulmonary complications following salvage esophagectomy after definitive chemoradiotherapy. J Surg Oncol 117:1251–1259
Shimada H, Fukagawa T, Haga Y, Oba K (2017) Does postoperative morbidity worsen the oncological outcome after radical surgery for gastrointestinal cancers? A systematic review of the literature. Ann Gastroenterol Surg 1:11–23
Haldar R, Ben-Eliyahu S (2018) Reducing the risk of post-surgical cancer recurrence: a perioperative anti-inflammatory anti-stress approach. Future Oncol 14:1017–1021
Matsuda S, Takeuchi H, Kawakubo H, Fukuda K, Nakamura R, Takahashi T, Wada N, Saikawa Y, Kitagawa Y (2015) Correlation between intense postoperative inflammatory response and survival of esophageal cancer patients who underwent transthoracic esophagectomy. Ann Surg Oncol 22:4453–4460
Brierley JD, Gospodarowicz MK, Wittekind C (eds) (2017) TNM classification of malignant tumors. International Union Against Cancer, 8th edn. Wiley, Oxford
Kuwano H, Nishimura Y, Oyama T, Kato H, Kitagawa Y, Kusano M, Shimada H, Takiuchi H, Toh Y, Doki Y, Naomoto Y, Matsubara H, Miyazaki T, Muto M, Yanagisawa A (2015) Guidelines for diagnosis and treatment of carcinoma of the esophagus April 2012 edited by the Japan Esophageal Society. Esophagus 12:1–30
Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, Nakamura T, Yabusaki H, Aoyama N, Kurita A, Ikeda K, Kanda T, Tsujinaka T, Nakamura K, Fukuda H (2012) A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol 19:68–74
Toh Y, Sakaguchi Y, Ikeda O, Adachi E, Ohgaki K, Yamashita Y, Oki E, Minami K, Okamura T (2009) The triangulating stapling technique for cervical esophagogastric anastomosis after esophagectomy. Surg Today 39:201–206
Yoshida N, Baba Y, Watanabe M, Hiyoshi Y, Ishimoto T, Iwagami S, Kurashige J, Sakamoto Y, Miyamoto Y, Baba H (2015) Triangulating stapling technique covered with the pedicled omental flap for esophagogastric anastomosis: a safe anastomosis with fewer complications. J Am Coll Surg 220:e13–e16
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Oka M, Yamamoto K, Takahashi M et al (1996) Relationship between serum levels of interleukin 6, various disease parameters and malnutrition in patients with esophageal squamous cell carcinoma. Cancer Res 56:2776–2780
Wang LS, Chow KC, Wu CW (1999) Expression and up-regulation of interleukin-6 in esophageal carcinoma cells by n-sodium butyrate. Br J Cancer 80:1617–1622
Yoneda M, Fujiwara H, Furutani A et al (2013) Prognostic impact of tumor IL-6 expression after preoperative chemoradiotherapy in patients with advanced esophageal squamous cell carcinoma. Anticancer Res 33:2699–2705
Ogura M, Takeuchi H, Kawakubo H, Nishi T, Fukuda K, Nakamura R, Takahashi T, Wada N, Saikawa Y, Omori T, Miyasho T, Yamada S, Kitagawa Y (2013) Clinical significance of CXCL-8/CXCR-2 network in esophageal squamous cell carcinoma. Surgery 154:512–520
Nishi T, Takeuchi H, Matsuda S, Ogura M, Kawakubo H, Fukuda K, Nakamura R, Takahashi T, Wada N, Saikawa Y, Omori T, Kitagawa Y (2015) CXCR2 expression and postoperative complications affect long-term survival in patients with esophageal cancer. World J Surg Oncol 13:232
Blaser MJ (2008) Understanding microbe-induced cancers. Cancer Prev Res (Phila) 1:15–20
Chochi K, Ichikura T, Kinoshita M, Majima T, Shinomiya N, Tsujimoto H, Kawabata T, Sugasawa H, Ono S, Seki S, Mochizuki H (2008) Helicobacter pylori augments growth of gastric cancers via the lipopolysaccharide-toll-like receptor 4 pathway whereas its lipopolysaccharide attenuates antitumor activities of human mononuclear cells. Clin Cancer Res 14:2909–2917
Bonnet M, Buc E, Sauvanet P, Darcha C, Dubois D, Pereira B, Dechelotte P, Bonnet R, Pezet D, Darfeuille-Michaud A (2014) Colonization of the human gut by E. coli and colorectal cancer risk. Clin Cancer Res 20:859–867
Watanabe M, Mine S, Nishida K, Yamada K, Shigaki H, Oya S, Matsumoto A, Kurogochi T, Okamura A, Imamura Y, Sano T (2016) Improvement in short-term outcomes after esophagectomy with a multidisciplinary perioperative care team. Esophagus 13:337–342
Miki Y, Toyokawa T, Kubo N, Tamura T, Sakurai K, Tanaka H, Muguruma K, Yashiro M, Hirakawa K, Ohira M (2017) C-reactive protein indicates early stage of postoperative infectious complications in patients following minimally invasive esophagectomy. World J Surg 41:796–803
Okamura A, Watanabe M, Fukudome I, Yamashita K, Yuda M, Hayami M, Imamura Y, Mine S (2018) Relationship between visceral obesity and postoperative inflammatory response following minimally invasive esophagectomy. World J Surg 42:3651–3657
Asti E, Bonitta G, Melloni M, Tornese S, Milito P, Sironi A, Costa E, Bonavina L (2018) Utility of C-reactive protein as predictive biomarker of anastomotic leak after minimally invasive esophagectomy. Langenbeck's Arch Surg 403:235–244
Park JK, Kim JJ, Moon SW (2017) C-reactive protein for the early prediction of anastomotic leak after esophagectomy in both neoadjuvant and non-neoadjuvant therapy case: a propensity score matching analysis. J Thorac Dis 9:3963–3702
Yamashita K, Watanabe M, Mine S, Toihata T, Fukudome I, Okamura A, Yuda M, Hayami M, Ishizuka N, Imamura Y (2018) Minimally invasive esophagectomy attenuates the postoperative inflammatory response and improves survival compared with open esophagectomy in patients with esophageal cancer: a propensity score matched analysis. Surg Endosc 32:4443–4450
Mariette C, Markar SR, Dabakuyo-Yonli TS et al (2019) Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med 380:152–162
Kataoka K, Takeuchi H, Mizusawa J, Ando M, Tsubosa Y, Koyanagi K, Daiko H, Matsuda S, Nakamura K, Kato K, Kitagawa Y (2016) A randomized phase III trial of thoracoscopic versus open esophagectomy for thoracic esophageal cancer: Japan clinical oncology group study JCOG1409. Jpn J Clin Oncol 46:174–177
Rahman SH, Evans J, Toogood GJ, Lodge PA, Prasad KR (2008) Prognostic utility of postoperative C-reactive protein for posthepatectomy liver failure. Arch Surg 143:247–253 discussion 53
Thompson D, Pepys MB, Wood SP (1999) The physiological structure of human C-reactive protein and its complex with phosphocholine. Structure 7:169–177
Watt DG, Horgan PG, McMillan DC (2015) Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery 157:362–380
Author information
Authors and Affiliations
Contributions
Study conception and design: all authors. Acquisition of data: all authors. Analysis and interpretation of data: Okamura, Watanabe, Yamashita, Mine. Drafting manuscript: Okamura, Watanabe, Yamashita, Mine. Critical revision of manuscript: all authors.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okamura, A., Yamashita, K., Kozuki, R. et al. Inflammatory response and recurrence after minimally invasive esophagectomy. Langenbecks Arch Surg 404, 761–769 (2019). https://doi.org/10.1007/s00423-019-01818-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01818-6