Abstract
Background
Complete mesocolic excision (CME) with central ligation or D3 lymphadenectomy has been reported to provide increased lymph node retrieval with the prospect of superior oncological results in colon cancer. However, right hemicolectomy with CME or D3 lymphadenectomy by laparoscopy is considered to be a technically challenging and time-consuming procedure with a higher risk of causing intraoperative injuries. Here, we introduce a novel laparoscopic approach for the D3 right hemicolectomy and report its feasibility, safety, and efficacy in cancer clearance.
Methods
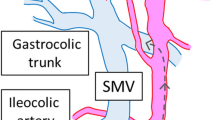
This purely medial to lateral approach of D3 hemicolectomy was characterized by the following two features: a series of repeated, unidirectional dissections along the superior mesentery vein (SMV) that were started below the ileocolic vein and ended at the pancreatic neck, followed by the exposure of the whole SMV and its colonic branches precisely before the ligation. From January 2012 to December 2015, 58 patients underwent this procedure. The short-term outcomes and long-term survival are reported.
Results
All 58 operations were finished with this procedure successfully, with one injury of the jejunal vein. The mean operation time was 164 ± 28.3 min, the mean blood loss was 64 ± 63.5 ml, and the mean number of retrieved lymph nodes was 28 ± 13.9. No mortality or major morbidity was observed. The 4-year overall survival was 78%, and the disease-free survival was 77%.
Conclusion
This novel, unidirectionally progressive, pancreas-oriented procedure for laparoscopic radical right hemicolectomy with D3 lymphadenectomy is safe and feasible, with the merit of providing an easier and safer way to tackle the variable tributaries of the SMV.



Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1(3):144–150
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100(1):75–82. https://doi.org/10.1002/bjs.8945
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol : Off J Am Soc Clin Oncol 25(21):3061–3068. https://doi.org/10.1200/jco.2006.09.7758
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, Ito M, Saito S, Fujii S, Konishi F, Saida Y, Hasegawa H, Akagi T, Sugihara K, Yamaguchi T, Masaki T, Fukunaga Y, Murata K, Okajima M, Moriya Y, Shimada Y (2017) Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol 2(4):261–268. https://doi.org/10.1016/s2468-1253(16)30207-2
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishihara S, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Boku N, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K, Japanese Society for Cancer of the C, Rectum (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20(2):207–239. https://doi.org/10.1007/s10147-015-0801-z
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol : Off J Am Soc Clin Oncol 30(15):1763–1769. https://doi.org/10.1200/JCO.2011.38.3992
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Color Dis : Off J Assoc Coloproctol G B Irel 11(4):354–364; discussion 364-355. https://doi.org/10.1111/j.1463-1318.2008.01735.x
Bertelsen CA, Neuenschwander AU, Jansen JE, Wilhelmsen M, Kirkegaard-Klitbo A, Tenma JR, Bols B, Ingeholm P, Rasmussen LA, Jepsen LV, Iversen ER, Kristensen B, Gogenur I, Danish Colorectal Cancer G (2015) Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 16(2):161–168. https://doi.org/10.1016/S1470-2045(14)71168-4
Sondenaa K, Quirke P, Hohenberger W, Sugihara K, Kobayashi H, Kessler H, Brown G, Tudyka V, D'Hoore A, Kennedy RH, West NP, Kim SH, Heald R, Storli KE, Nesbakken A, Moran B (2014) The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery : proceedings of a consensus conference. Int J Color Dis 29(4):419–428. https://doi.org/10.1007/s00384-013-1818-2
Matsuda T, Iwasaki T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2016) Laparoscopic complete mesocolic excision for right-sided colon cancer using a cranial approach: anatomical and embryological consideration. Int J Color Dis 32:139–141. https://doi.org/10.1007/s00384-016-2673-8
Kontovounisios C, Kinross J, Tan E, Brown G, Rasheed S, Tekkis P (2015) Complete mesocolic excision in colorectal cancer: a systematic review. Color Dis : Off J Assoc Coloproctology G B Irel 17(1):7–16. https://doi.org/10.1111/codi.12793
Bae SU, Saklani AP, Lim DR, Kim DW, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2014) Laparoscopic-assisted versus open complete mesocolic excision and central vascular ligation for right-sided colon cancer. Ann Surg Oncol 21(7):2288–2294. https://doi.org/10.1245/s10434-014-3614-9
Li H, He Y, Lin Z, Xiong W, Diao D, Wang W, Wan J, Zou L (2016) Laparoscopic caudal-to-cranial approach for radical lymph node dissection in right hemicolectomy. Langenbeck's Arch Surg/ Dtsch Ges Chir 401(5):741–746. https://doi.org/10.1007/s00423-016-1465-5
Zhao LY, Li GX, Zhang C, Yu J, Deng HJ, Wang YN, Hu YF, Cheng X (2012) Vascular anatomy of the right colon and vascular complications during laparoscopic surgery. Zhonghua wei chang wai ke za zhi = Chinese journal of gastrointestinal surgery 15(4):336–341
Spasojevic M, Stimec BV, Fasel JF, Terraz S, Ignjatovic D (2011) 3D relations between right colon arteries and the superior mesenteric vein: a preliminary study with multidetector computed tomography. Surg Endosc 25(6):1883–1886. https://doi.org/10.1007/s00464-010-1480-5
Benz S (2016) The uncinate-first approach for laparoscopic complete mesocolic right hemicolectomy—a video vignette. Color Dis : Off J Assoc Coloproctology G B Irel 18(1):109. https://doi.org/10.1111/codi.13157
Benz S, Tam Y, Tannapfel A, Stricker I (2016) The uncinate process first approach: a novel technique for laparoscopic right hemicolectomy with complete mesocolic excision. Surg Endosc 30(5):1930–1937. https://doi.org/10.1007/s00464-015-4417-1
Yamaguchi S, Kuroyanagi H, Milsom JW, Sim R, Shimada H (2002) Venous anatomy of the right colon: precise structure of the major veins and gastrocolic trunk in 58 cadavers. Dis Colon Rectum 45(10):1337–1340. https://doi.org/10.1097/01.DCR.0000027284.76452.84
Ogino T, Takemasa I, Horitsugi G, Furuyashiki M, Ohta K, Uemura M, Nishimura J, Hata T, Mizushima T, Yamamoto H, Doki Y, Mori M (2014) Preoperative evaluation of venous anatomy in laparoscopic complete mesocolic excision for right colon cancer. Ann Surg Oncol 21(Suppl 3):S429–S435. https://doi.org/10.1245/s10434-014-3572-2
Nesgaard JM, Stimec BV, Bakka AO, Edwin B, Ignjatovic D, group RCCs (2015) Navigating the mesentery: a comparative pre- and per-operative visualization of the vascular anatomy. Color Dis :Off J Assoc Coloproctology G B Irel 17(9):810–818. https://doi.org/10.1111/codi.13003
Mori S, Baba K, Yanagi M, Kita Y, Yanagita S, Uchikado Y, Arigami T, Uenosono Y, Okumura H, Nakajo A, Maemuras K, Ishigami S, Natsugoe S (2015) Laparoscopic complete mesocolic excision with radical lymph node dissection along the surgical trunk for right colon cancer. Surg Endosc 29(1):34–40. https://doi.org/10.1007/s00464-014-3650-3
Matsuda T, Iwasaki T, Mitsutsuji M, Hirata K, Maekawa Y, Tanaka T, Shimada E, Kakeji Y (2015) Cranial-to-caudal approach for radical lymph node dissection along the surgical trunk in laparoscopic right hemicolectomy. Surg Endosc 29(4):1001. https://doi.org/10.1007/s00464-014-3761-x
Zou L, Xiong W, Mo D, He Y, Li H, Tan P, Wang W, Wan J (2016) Laparoscopic radical extended right hemicolectomy using a caudal-to-cranial approach. Ann Surg Oncol 23(8):2562–2563. https://doi.org/10.1245/s10434-016-5215-2
Matsuda T, Iwasaki T, Mitsutsuji M, Hirata K, Maekawa Y, Tsugawa D, Sugita Y, Sumi Y, Shimada E, Kakeji Y (2015) Cranially approached radical lymph node dissection around the middle colic vessels in laparoscopic colon cancer surgery. Langenbeck's Arch Surg/ Dtsch Ges Chir 400(1):113–117. https://doi.org/10.1007/s00423-014-1250-2
Kanemitsu Y, Komori K, Kimura K, Kato T (2013) D3 lymph node dissection in right hemicolectomy with a no-touch isolation technique in patients with colon cancer. Dis Colon Rectum 56(7):815–824. https://doi.org/10.1097/DCR.0b013e3182919093
Merrie AE, Phillips LV, Yun K, McCall JL (2001) Skip metastases in colon cancer: assessment by lymph node mapping using molecular detection. Surgery 129(6):684–691. https://doi.org/10.1067/msy.2001.113887
Chen G, McIver CM, Texler M, Lloyd JM, Rieger N, Hewett PJ, Sen Wan D, Hardingham JE (2004) Detection of occult metastasis in lymph nodes from colorectal cancer patients: a multiple-marker reverse transcriptase-polymerase chain reaction study. Dis Colon Rectum 47(5):679–686. https://doi.org/10.1007/s10350-003-0118-2
Kobayashi H, West NP, Takahashi K, Perrakis A, Weber K, Hohenberger W, Quirke P, Sugihara K (2014) Quality of surgery for stage III colon cancer: comparison between England, Germany, and Japan. Ann Surg Oncol 21(Suppl 3):S398–S404. https://doi.org/10.1245/s10434-014-3578-9
Moritani K, Hasegawa H, Okabayashi K, Ishii Y, Endo T, Kitagawa Y (2014) Difference in the recurrence rate between right- and left-sided colon cancer: a 17-year experience at a single institution. Surg Today 44(9):1685–1691. https://doi.org/10.1007/s00595-013-0748-5
Acknowledgements
We also thank a doctor of our team, Yazhou He (MD, Department of Gastrointestinal Surgery, West China Hospital, Sichuan University, Chengdu, China; and Institute of Genetics and Molecular Medicine, Western General Hospital, Edinburgh University, Edinburgh, UK), who revised this manuscript.
Funding
This study was funded by the Scientific and Technology department of Sichuan Province (grant no. 2016SZ0043).
Author information
Authors and Affiliations
Contributions
Xiangbing Deng and Tao Hu analyzed the data and drafted of manuscript; Tao Hu, Mingtian Wei, Qingbin Wu, and Tinghan Yang contributed for the acquisition and interpretation of the data; Wenjian Meng and Ziqiang Wang revised this manuscript; Wenjian Meng and Ziqiang Wang contributed for the study conception, design, and revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. In addition, this study was approved by the Ethics Committee of West China Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Supplementary Fig 1
the enlarged and vulnerable AIPDVs. Red arrows: AIPDVs; black arrows: RGEV; if the operation ligating the GTH is shown as a white arrow, the AIPDVs may cause troublesome bleeding, and haemostatic procedure may injure the pancreas. (PNG 16020 kb)
Rights and permissions
About this article
Cite this article
Deng, X., Hu, T., Wei, M. et al. Feasibility of a unidirectionally progressive, pancreas-oriented procedure for laparoscopic D3 right hemicolectomy. Langenbecks Arch Surg 403, 761–768 (2018). https://doi.org/10.1007/s00423-018-1703-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1703-0