Abstract
Aim
Single-incision laparoscopic surgery (SILS) has been introduced as a new technique for the treatment of various colorectal diseases. Recurrent or complicated diverticulitis of the sigmoid colon is a frequent indication for minimally invasive sigmoid colectomy. The aim of this study was to investigate the impact of obesity on the outcome of SILS sigmoid colectomy.
Methods
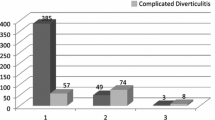
From September 2009 to October 2014, data from 377 patients who had intended SILS sigmoid colectomy for diverticulitis at our institution were collected in a prospective database. The patients were categorized in the following subgroups: group 1 (normal weight, body mass index (BMI) < 25 kg/m2) , group 2 (overweight, BMI 25–29.9 kg/m2), group 3 (obesity, BMI 30–34.9 kg/m2), and group 4 (morbid obesity, BMI > 35 kg/m2).
Results
The groups were equivalent for sex, age, status of diverticulitis, the presence of acute inflammation in the specimen, and the percentage of teaching operations, but the percentage of patients with accompanying diseases was significantly more frequent in groups 2, 3, and 4 (p = 0.04, 0.008, and 0.018, respectively). As compared to group 1, the conversion rate was significantly increased in groups 2 and 4 (2.3 vs. 9.3 % (p = 0.013) and 2.3 vs. 12.5 % (p = 0.017), respectively). The duration of surgery, hospitalization, and morbidity did not differ between the four groups.
Conclusion
Up to a body mass index of 35 kg/m2, increased body weight does not significantly reduce the feasibility and outcome of single-incision laparoscopic surgery for diverticulitis.
Similar content being viewed by others
References
Andersen JC, Bundgaard L, Elbrond H, Laurberg S, Walker LR, Stovring J (2012) Danish national guidelines for treatment of diverticular disease. Dan Med J 59(5):C4453
Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R et al (2013) Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol: Off Clin Pract J Am Gastroenterol Assoc 11(12):1609–1613
Jeyarajah S, Faiz O, Bottle A, Aylin P, Bjarnason I, Tekkis PP et al (2009) Diverticular disease hospital admissions are increasing, with poor outcomes in the elderly and emergency admissions. Aliment Pharmacol Ther 30(11–12):1171–1182
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ et al (2012) Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 143(5):1179–1187, e1-3
Etzioni DA, Mack TM, Beart RW Jr, Kaiser AM (2009) Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg 249(2):210–217
Tursi A, Brandimarte G, Elisei W, Picchio M, Forti G, Pianese G et al (2013) Randomised clinical trial: mesalazine and/or probiotics in maintaining remission of symptomatic uncomplicated diverticular disease—a double-blind, randomised, placebo-controlled study. Aliment Pharmacol Ther 38(7):741–751
Parente F, Bargiggia S, Prada A, Bortoli A, Giacosa A, Germana B et al (2013) Intermittent treatment with mesalazine in the prevention of diverticulitis recurrence: a randomised multicentre pilot double-blind placebo-controlled study of 24-month duration. Int J Color Dis 28(10):1423–1431
Chabok A, Pahlman L, Hjern F, Haapaniemi S, Smedh K (2012) Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 99(4):532–539
Rafferty J, Shellito P, Hyman NH, Buie WD (2006) Practice parameters for sigmoid diverticulitis. Dis Colon Rectum 49(7):939–944
Ritz JP, Lehmann KS, Frericks B, Stroux A, Buhr HJ, Holmer C (2011) Outcome of patients with acute sigmoid diverticulitis: multivariate analysis of risk factors for free perforation. Surgery 149(5):606–613
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD et al (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57(3):284–294
Kruis W, Germer CT, Leifeld L (2014) Diverticular disease: guidelines of the German Society for Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Digestion 90(3):190–207
Leifeld L, Germer CT, Bohm S, Dumoulin FL, Hauser W, Kreis M et al (2014) S2k guidelines diverticular disease/diverticulitis. Z Gastroenterol 52(7):663–710, S2k-Leitlinie Divertikelkrankheit/Divertikulitis
Wolff BG, Boostrom SY (2012) Prophylactic resection, uncomplicated diverticulitis, and recurrent diverticulitis. Dig Dis 30(1):108–113
Gervaz P, Inan I, Perneger T, Schiffer E, Morel P (2010) A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg 252(1):3–8
Raue W, Paolucci V, Asperger W, Albrecht R, Buchler MW, Schwenk W (2011) Laparoscopic sigmoid resection for diverticular disease has no advantages over open approach: midterm results of a randomized controlled trial. Langenbeck’s Arch Surg/Deut Ges fur Chir 396(7):973–980
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev 3, CD003145
Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES et al (2009) Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg 249(1):39–44
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ (2001) Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy: a comparative study. Dis Colon Rectum 44(12):1800–1807
Chung CC, Tsang WW, Kwok SY, Li MK (2003) Laparoscopy and its current role in the management of colorectal disease. Colorectal Dis: Off J Assoc Coloproctology Great Br Ireland 5(6):528–543
Rink AD, John-Enzenauer K, Haaf F, Straub E, Nagelschmidt M, Vestweber KH (2009) Laparoscopic-assisted or laparoscopic-facilitated sigmoidectomy for diverticular disease? A prospective randomized trial on postoperative pain and analgesic consumption. Dis Colon Rectum 52(10):1738–1745
Yang TX, Chua TC (2013) Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Color Dis 28(1):89–101
Vestweber B, Galetin T, Lammerting K, Paul C, Giehl J, Straub E et al (2013) Single-incision laparoscopic surgery: outcomes from 224 colonic resections performed at a single center using SILS. Surg Endosc 27(2):434–442
Vestweber B, Alfes A, Paul C, Haaf F, Vestweber KH (2010) Single-incision laparoscopic surgery: a promising approach to sigmoidectomy for diverticular disease. Surg Endosc 24(12):3225–3228
Gash KJ, Goede AC, Kaldowski B, Vestweber B, Dixon AR (2011) Single incision laparoscopic (SILS) restorative proctocolectomy with ileal pouch-anal anastomosis. Surg Endosc 25(12):3877–3880
Leblanc F, Makhija R, Champagne BJ, Delaney CP (2011) Single incision laparoscopic total colectomy and proctocolectomy for benign disease: initial experience. Colorectal Dis: Off J Assoc Coloproctol Great Br Ireland 13(11):1290–1293
Rijcken E, Mennigen R, Argyris I, Senninger N, Bruewer M (2012) Single-incision laparoscopic surgery for ileocolic resection in Crohn’s disease. Dis Colon Rectum 55(2):140–146
Mynster T, Hammer J, Wille-Jorgensen P (2012) Preliminary results after single-port laparoscopic colonic surgery. Dan Med J 59(12):A4551
Champagne BJ, Papaconstantinou HT, Parmar SS, Nagle DA, Young-Fadok TM, Lee EC et al (2012) Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg 255(1):66–69
Bulut O, Nielsen CB, Jespersen N (2011) Single-port access laparoscopic surgery for rectal cancer: initial experience with 10 cases. Dis Colon Rectum 54(7):803–809
Humes DJ, Spiller RC (2014) Review article: the pathogenesis and management of acute colonic diverticulitis. Aliment Pharmacol Ther 39(4):359–370
Pisanu A, Vacca V, Reccia I, Podda M, Uccheddu A (2013) Acute diverticulitis in the young: the same disease in a different patient. Gastroenterol Res Pract 2013:867961
Pilgrim SM, Hart AR, Speakman CT (2013) Diverticular disease in younger patients—is it clinically more complicated and related to obesity? Colorectal Dis: Off J Assoc Coloproctol Great Br Ireland 15(10):1205–1210
Hjern F, Wolk A, Hakansson N (2012) Obesity, physical inactivity, and colonic diverticular disease requiring hospitalization in women: a prospective cohort study. Am J Gastroenterol 107(2):296–302
Bailey MB, Davenport DL, Procter L, McKenzie S, Vargas HD (2013) Morbid obesity and diverticulitis: results from the ACS NSQIP dataset. J Am Coll Surg 217(5):874–880, e1
Benoist S, Panis Y, Alves A, Valleur P (2000) Impact of obesity on surgical outcomes after colorectal resection. Am J Surg 179(4):275–281
Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR et al (2002) Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg 95(6):1788–1792, table of contents
Wick EC, Hirose K, Shore AD, Clark JM, Gearhart SL, Efron J et al (2011) Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg 146(9):1068–1072
Howard DP, Datta G, Cunnick G, Gatzen C, Huang A (2010) Surgical site infection rate is lower in laparoscopic than open colorectal surgery. Colorectal Dis: Off J Assoc Coloproctol Great Br Ireland 12(5):423–427
Weiss HG, Brunner W, Biebl MO, Schirnhofer J, Pimpl K, Mittermair C et al (2014) Wound complications in 1145 consecutive transumbilical single-incision laparoscopic procedures. Ann Surg 259(1):89–95
Esteban F, Cerdan FJ, Garcia-Alonso M, Sanz-Lopez R, Arroyo A, Ramirez JM et al (2014) A multicentre comparison of a fast track or conventional postoperative protocol following laparoscopic or open elective surgery for colorectal cancer surgery. Colorectal Dis: Off J Assoc Coloproctol Great Br Ireland 16(2):134–140
Li MZ, Xiao LB, Wu WH, Yang SB, Li SZ (2012) Meta-analysis of laparoscopic versus open colorectal surgery within fast-track perioperative care. Dis Colon Rectum 55(7):821–827
Kang CY, Halabi WJ, Chaudhry OO, Nguyen V, Ketana N, Carmichael JC et al (2013) A nationwide analysis of laparoscopy in high-risk colorectal surgery patients. J Gastrointest Surg: Off J Soc Surg Aliment Tract 17(2):382–391
Poon JT, Law WL, Wong IW, Ching PT, Wong LM, Fan JK et al (2009) Impact of laparoscopic colorectal resection on surgical site infection. Ann Surg 249(1):77–81
Shapiro R, Vogel JD, Kiran RP (2011) Risk of postoperative venous thromboembolism after laparoscopic and open colorectal surgery: an additional benefit of the minimally invasive approach? Dis Colon Rectum 54(12):1496–1502
Feroci F, Kroning KC, Lenzi E, Moraldi L, Cantafio S, Scatizzi M (2011) Laparoscopy within a fast-track program enhances the short-term results after elective surgery for resectable colorectal cancer. Surg Endosc 25(9):2919–2925
Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW (2012) Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Color Dis 27(6):773–780
Makino T, Shukla PJ, Rubino F, Milsom JW (2012) The impact of obesity on perioperative outcomes after laparoscopic colorectal resection. Ann Surg 255(2):228–236
Vestweber B, Vestweber KH, Paul C, Rink AD (2015) Single-port laparoscopic resection for diverticular disease: experiences with more than 300 consecutive patients. Surg Endosc. doi:10.1007/s00464-015-4160-7
Hansen O, Stock, W (1999) Prophylaktische operation bei der divertikelkrankheit des kolons - stufenkonzept durch exaktes stadieneinteilung. Langenbecks Arch Chir (Suppl 2)1257–1260
Alves A, Panis Y, Slim K, Heyd B, Kwiatkowski F, Mantion G (2005) French multicentre prospective observational study of laparoscopic versus open colectomy for sigmoid diverticular disease. Br J Surg 92(12):1520–1525
Lu KC, Cone MM, Diggs BS, Rea JD, Herzig DO (2011) Laparoscopic converted to open colectomy: predictors and outcomes from the Nationwide Inpatient Sample. Am J Surg 201(5):634–639
Dwivedi A, Chahin F, Agrawal S, Chau WY, Tootla A, Tootla F et al (2002) Laparoscopic colectomy vs. open colectomy for sigmoid diverticular disease. Dis Colon Rectum 45(10):1309–1314, discussion 14–5
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G et al (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216(6):1037–1047, discussion 47–8
Sangster W, Kulaylat AN, Stewart DB, Schubart JR, Koltun WA, Messaris E (2015) Hernia incidence following single-site vs standard laparoscopic colorectal surgery. Colorectal Dis: Off J Assoc Coloproctol Great Br Ireland 17(3):250–256
Marks JH, Montenegro GA, Shields MV, Frenkel JL, Marks GJ (2015) Single-port laparoscopic colorectal surgery shows equivalent or better outcomes to standard laparoscopic surgery: results of a 190-patient, 7-criterion case-match study. Surg Endosc 29(6):1492–1499
Markar SR, Wiggins T, Penna M, Paraskeva P (2014) Single-incision versus conventional multiport laparoscopic colorectal surgery—systematic review and pooled analysis. J Gastrointest Surg: Off J Soc Surg Aliment Tract 18(12):2214–2227
Acknowledgments
We thank Dr. Jörg Haensel for linguistically and grammatically reviewing our manuscript.
Compliance with ethical standards
ᅟ
Funding
None
Conflicts of interest
Boris Vestweber got fees for developing, teaching, and supervising single-port laparoscopic colorectal surgery from Covidien. There are no other conflicts of interest.
Informed consent
All patients included in this trial gave informed consent concerning the use of the surgical methods described in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rink, A.D., Vestweber, B., Hahn, J. et al. Single-incision laparoscopic surgery for diverticulitis in overweight patients. Langenbecks Arch Surg 400, 797–804 (2015). https://doi.org/10.1007/s00423-015-1333-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1333-8