Abstract
Purpose
The objective of this study was to investigate the co-effect of long-term exposure to atmospheric particulate matter PM2.5 and single nucleotide polymorphisms on schizophrenia relapse.
Methods
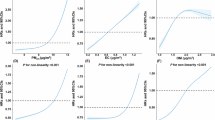
A total of 332 patients with schizophrenia were recruited. Genotyping of eight SNPs for five genes along the neurotrophin signaling pathway was performed by the Sequenom Massarray technology platform. Based on the data from the monitoring stations, the PM2.5 level of each patient's residence was assessed by the inverse distance weighting method using Arc GIS software. Cox regression analysis was used to determine independent risk factors. The relationship between PM2.5 levels and the risk of schizophrenia relapse was evaluated using the restricted cubic spline (RCS) method.
Results
In this study, a total of 191 of 332 patients with schizophrenia relapsed with hospitalization. The risk of schizophrenia relapse was 13.62 (95% CI 8.29 to 22.37) in areas with PM2.5 concentrations of 48.43 to 75.35 µg/m3. The risk of schizophrenia relapse was 5.81 (95% CI 3.58–9.42, p < 0.001) and 13.62 (95% CI 8.29–22.37, p < 0.001) in the exposure categories Q3 and Q4, respectively, compared with Q1, and non-linear relationship between cumulative PM2.5 exposure and risk of schizophrenia relapse. A greater association was observed in the YWHAB gene polymorphic locus rs6031849 genotype TG (Hazard ratio 16.62, 95% CI 5.73 to 48.24).
Conclusions
PM2.5 levels, YWHAB gene polymorphism locus rs6031849, and gender jointly influenced schizophrenia relapse, with long-term exposure to high levels of PM2.5 having the greatest effect on schizophrenia relapse.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
Data are available from the corresponding author upon reasonable request.
References
Allen JL et al (2017) Developmental neurotoxicity of inhaled ambient ultrafine particle air pollution: parallels with neuropathological and behavioral features of autism and other neurodevelopmental disorders. Neurotoxicology 59:140–154
Attademo L et al (2017) Environmental pollution and risk of psychotic disorders: a review of the science to date. Schizophr Res 181:55–59
Bai KJ et al (2019) Microglial activation and inflammation caused by traffic-related particulate matter. Chem Biol Interact 311:108762
Bai L et al (2020) Durational effect of particulate matter air pollution wave on hospital admissions for schizophrenia. Environ Res 187:109571
Benedetti F et al (2011) Recurrence of bipolar mania is associated with catechol-O-methyltransferase Val(108/158)Met polymorphism. J Affect Disord 132(1–2):293–296
Block ML et al (2012) The outdoor air pollution and brain health workshop. Neurotoxicology 33(5):972–984
Braithwaite I et al (2019) Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect 127(12):126002
Cacciottolo M et al (2020) Traffic-related air pollutants (TRAP-PM) promote neuronal amyloidogenesis through oxidative damage to lipid rafts. Free Radic Biol Med 147:242–251
Charlson FJ et al (2018) Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull 44(6):1195–1203
Costa LG et al (2017) Neurotoxicity of traffic-related air pollution. Neurotoxicology 59:133–139
Costa LG et al (2020) Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol Ther 210:107523
de Prado Bert P et al (2018) The effects of air pollution on the brain: a review of studies interfacing environmental epidemiology and neuroimaging. Curr Environ Health Rep 5(3):351–364
Duan J et al (2018) Is the serious ambient air pollution associated with increased admissions for schizophrenia? Sci Total Environ 644:14–19
Emsley R et al (2013) The nature of relapse in schizophrenia. BMC Psychiatry 13:50
Gao J et al (2021) Elevated environmental PM2.5 increases risk of schizophrenia relapse: mediation of inflammatory cytokines. Sci Total Environ 753:1428
GBD 2019 Mental Disorders Collaborators and others (2022) Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry 9(2):137–150
Gejman PV, Sanders AR, Kendler KS (2011) Genetics of schizophrenia: new findings and challenges. Annu Rev Genom Hum Genet 12:121–144
Green IW, Glausier JR (2016) Different paths to core pathology: the equifinal model of the schizophrenia syndrome. Schizophr Bull 42(3):542–549
Guo P et al (2020) Ambient air pollution and markers of fetal growth: a retrospective population-based cohort study of 2.57 million term singleton births in China. Environ Int 135:105410
Huang Y et al (2019) Prevalence of mental disorders in China: a cross-sectional epidemiological study. ThLancet Psychiatry 6(3):211–224
Huang J et al (2020) Phosphoinositide-3-kinase regulatory subunit 1 gene polymorphisms are associated with schizophrenia and bipolar disorder in the Han Chinese population. Metab Brain Dis 35(5):785–792
Huckins LM et al (2019) Gene expression imputation across multiple brain regions provides insights into schizophrenia risk. Nat Genet 51(4):659–674
Ikeda M et al (2008) Identification of YWHAE, a gene encoding 14-3-3epsilon, as a possible susceptibility gene for schizophrenia. Hum Mol Genet 17(20):3212–3222
Jacobsen KK et al (2015) Epistatic and gene wide effects in YWHA and aromatic amino hydroxylase genes across ADHD and other common neuropsychiatric disorders: association with YWHAE. Am J Med Genet B Neuropsychiatr Genet 168(6):423–432
Ji Y et al (2021) Particulate matter pollution associated with schizophrenia hospital re-admissions: a time-series study in a coastal Chinese city. Environ Sci Pollut Res Int 28(41):58355–58363
Khan A et al (2019) Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLoS Biol 17(8):e3000353
Levesque S et al (2011) Diesel exhaust activates and primes microglia: air pollution, neuroinflammation, and regulation of dopaminergic neurotoxicity. Environ Health Perspect 119(8):1149–1155
Liang Z et al (2019) The association between short-term ambient air pollution and daily outpatient visits for schizophrenia: a hospital-based study. Environ Pollut 244:102–108
Mohammadi A, Amooeian VG, Rashidi E (2018) Dysfunction in brain-derived neurotrophic factor signaling pathway and susceptibility to schizophrenia, Parkinson’s and Alzheimer’s diseases. Curr Gene Ther 18(1):45–63
Momtazmanesh S, Zare-Shahabadi A, Rezaei N (2019) Cytokine alterations in schizophrenia: an updated review. Front Psychiatry. 10:892
Mutlu EA (2011) Particulate matter air pollution causes oxidantmediated increase in gut permeability in mice. Part Fibre Toxicol 8:19
Organization, World Health 2016 World Health Organization WHO releases country estimates on air pollution exposure and health impact . https://www.who.int/mediacentre/news/releases/2016/air-pollution-estimates/en/.
Oudin A et al (2016) Association between neighbourhood air pollution concentrations and dispensed medication for psychiatric disorders in a large longitudinal cohort of Swedish children and adolescents. BMJ Open 6(6):e010004
Peters R et al (2019) Air pollution and dementia: a systematic review. J Alzheimers Dis 70(s1):S145–S163
Qing Y et al (2016) Dysregulated 14-3-3 family in peripheral blood leukocytes of patients with schizophrenia. Sci Rep 6:23791
Russ TC, Reis S, van Tongeren M (2019) Air pollution and brain health: defining the research agenda. Curr Opin Psychiatry 32(2):97–104
Schizophrenia Working Group of the Psychiatric Genomics, Consortium (2014) Biological insights from 108 schizophrenia-associated genetic loci. Nature 511(7510):421–427
Song J et al (2018) Acute effects of ambient particulate matter pollution on hospital admissions for mental and behavioral disorders: a time-series study in Shijiazhuang, China. Sci Total Environ 636:205–211
Su L et al (2014) Association between the NOTCH4 gene rs3131296 polymorphism with schizophrenia risk in the Chinese Zhuang population and Chinese Han population. Acta Neuropsychiatr 26(4):240–245
Su Y et al (2021) The interaction of ASAH1 and NGF gene involving in neurotrophin signaling pathway contributes to schizophrenia susceptibility and psychopathology. Prog Neuropsychopharmacol Biol Psychiatry 104:110015
Thirthalli J et al (2010) Do antipsychotics limit disability in schizophrenia? A naturalistic comparative study in the community. Indian J Psychiatry 52(1):37–41
Wang G et al (2013) Effects of ozone and fine particulate matter (PM(2.5)) on rat system inflammation and cardiac function. Toxicol Lett 217(1):23–33
Whiteford HA et al (2013) Global burden of disease attributable to mental and substance use disorders: findings from the global burden of disease study 2010. The Lancet 382(9904):1575–1586
Woodward NC et al (2018) Prenatal and early life exposure to air pollution induced hippocampal vascular leakage and impaired neurogenesis in association with behavioral deficits. Transl Psychiatry 8(1):261
Worthington MA et al (2020) Air pollution and hippocampal atrophy in first episode schizophrenia. Schizophr Res 218:63–69
Xiao J et al (2015) High relapse rate and poor medication adherence in the Chinese population with schizophrenia: results from an observational survey in the People’s Republic of China. Neuropsychiatr Dis Treat 11:1161–1167
Yang J et al (2019a) Rs7219 regulates the expression of GRB2 by affecting miR-1288-mediated inhibition and contributes to the risk of schizophrenia in the Chinese Han population. Cell Mol Neurobiol 39(1):137–147
Yang J et al (2019b) TP53 polymorphism contributes to the susceptibility to bipolar disorder but not to schizophrenia in the Chinese Han population. J Mol Neurosci 68(4):679–687
Yi W et al (2021) Does the gut microbiome partially mediate the impact of air pollutants exposure on liver function? Evidence based on schizophrenia patients. Environ Pollut 291:118135
Zamanpoor M (2020) Schizophrenia in a genomic era: a review from the pathogenesis, genetic and environmental etiology to diagnosis and treatment insights. Psychiatr Genet 30(1):1–9
Acknowledgements
We thank the Guangxi Zhuang Autonomous Region Brain Hospital for providing critical technical support.
Funding
This work was supported by the Natural Science Foundation of China (81874395).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
All participants were informed of the process and purpose of this research and signed informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lei, Q., Huang, X., Li, T. et al. Effects of PM2.5 pollution and single nucleotide polymorphisms of neurotrophin signaling pathway genes acting together on schizophrenia relapse. Int Arch Occup Environ Health 96, 629–637 (2023). https://doi.org/10.1007/s00420-023-01958-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-023-01958-9