Abstract
Purpose
Corneal collagen crosslinking (CXL) is the primary treatment for progressive keratoconus which has a significant impact on vision and quality of life. Our study aimed to compare the efficacy and safety of epithelium-on versus epithelium-off CXL to treat keratoconus.
Methods
We searched PubMed, Medline, Embase, Web of Science, and Scopus databases. We included studies that compared standard epithelium-off with epithelium-on CXL. The primary outcome measures were changes in corrected distance visual acuity (CDVA) and maximum keratometry (Kmax), and the secondary outcomes were uncorrected distance visual acuity (UDVA), central corneal thickness (CCT), and adverse events. A meta-analysis was performed on the primary and secondary outcomes based on the weighted mean differences between baseline to 12-month follow-up.
Results
The search retrieved 887 publications with 27 included in the systematic review. A total of 1622 eyes (1399 patients; age 25.51 ± 4.02 years) were included in comparisons of epithelium-off to epithelium-on CXL in keratoconus. Epithelium-off CXL treated 800 eyes and epithelium-on CXL for 822 eyes. At 12-month follow-up, CDVA and Kmax showed no significant difference between the epithelium-off and epithelium-on CXL. The secondary outcomes showed that UDVA was better in epithelium-off CXL (− 0.11D, 95% CI − 0.12, − 0.1; p < 0.001) and there was more thinning in CCT in epithelium-off CXL (− 3.23 μm, 95% CI − 4.64, − 1.81; p <0.001).
Conclusion
Epithelium-off and epithelium-on CXL were both effective to treat progressive keratoconus. Further research is needed to compare the long-term outcomes and safety of both CXL protocols for adaptation into clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Keratoconus derives from the Greek words ‘kéras,’ meaning cornea and ‘cõnus’ meaning cone, which together gives ‘cone-shaped’ cornea [1]. It is a bilateral asymmetric condition causing progressive corneal thinning and steepening and leading to irregular astigmatism and decreased visual acuity [2]. Epidemiological studies estimate keratoconus prevalence to be between 0.2 and 4790 people per 100,000 with an incidence from 1.5 to 25 per 100,000 people each year [3,4,5,6]. Keratoconus and crosslinking have a significant impact on quality of life [7, 8].
The primary treatment of progressive keratoconus is corneal collagen crosslinking (CXL) [9,10,11]. The CXL procedure aims to stabilize and prevent progression by enhancing the mechanical stability of the cornea [12]. In CXL, riboflavin acts as a photosensitizer to ultraviolet radiation to strengthen the collagen bonds in the cornea [13]. Typically, the CXL procedure involves removal of the epithelium (epithelium-off CXL) to enhance riboflavin penetration although this has been adapted over time [14, 15]. Crosslinking can also be performed with an intact epithelium (epithelium-on CXL) in an effort to decrease the risks associated with removal of the epithelium including microbial keratitis, delayed re-epithelisation, discomfort, haze, corneal edema, and thinning of the cornea [16,17,18]. However, the corneal epithelium acts as a barrier for riboflavin diffusion which may hinder the CXL photochemical reaction and thus may compromise efficacy of the procedure [19].
A Cochrane meta-analysis of 6 studies reported that there was no evidence of a difference in maximum keratometry (Kmax) and corrected distance visual acuity (CDVA) at 12-month follow-up [20]. There have been a further three meta-analyses which also showed no convincing suggestion for the superiority of epithelium-off or epithelium-on CXL [21,22,23]. To our knowledge, our study has the largest number of included studies compared to previous studies. Patients having CXL are seeking answers from clinicians as to whether they should have epithelium-off or epithelium-on CXL and clinicians are awaiting the highest level of evidence to inform patients on the efficacy and safety of the procedures. We performed this study to add to the evidence base to answer these questions.
The aim of this study was using available evidence to assess the efficacy and safety of epithelium-off with epithelium-on CXL.
Method
A systematic review and meta-analysis of studies comparing epithelium-off to epithelium-on CXL in patients with keratoconus was performed with reference to the Cochrane and Centre for Reviews and Dissemination. The review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) guidelines [24].
Search strategy
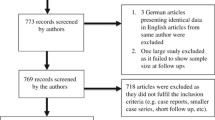
A systematic literature search was conducted in Medline, Embase, PubMed, Scopus, and Web of Science databases to May 2022. The search strategy is outlined in emental Digital Content 1. The main search concepts were the population (patients with keratoconus), treatment (crosslinking), and specific surgical technique (epithelium off and on). The search was restricted to studies within the last 10 years and in English. A search in the grey literature was performed in OpenGrey. The reference lists were hand-searched to identify additional studies. Fig. 1 is a flowchart based on PRISMA for the study.
Study selection, screening, and data extraction
We included studies that compared outcomes on the efficacy and safety of epithelium-off to epithelium-on CXL in patients with keratoconus. Patients were included in meta-analysis if the CDVA and Kmax at 12 months were compared. The population was restricted to adult patients and non-human studies were excluded.
The publications were screened by two authors (GB and HK) and discrepancies resolved by consensus (GB, HK, and SW). All retrieved articles were exported to Covidence to remove duplicates, screen titles, and abstracts and for a full-text review. The data of interest included: study data (author, year of publication), country in which the study was country, patient demographics, study characteristics, CDVA, uncorrected distance visual acuity (UDVA), corneal parameters (K2, Kmax), central corneal thickness (CCT), and adverse events.
Risk of bias
The risk of bias was determined for each study using the National Health and Medical Research Council guidelines [25]. The risk of bias for the randomized control trials (RCTs) was evaluated by the Cochrane RoB 2.0 tool and the studies that were non-randomized prospective studies were assessed by ROBINS-I [26,27,28]. This risk of bias assessment was conducted by two reviewers (GB and HK) independently and disagreements were resolved through discussion with the third reviewer (SW). The risk of bias figures were generated using the Risk-of-bias Visualisation (Robvis) tool which uses an R package and Shiny web app to visualize the risk of bias assessment (Supplemental Digital Content 4 and Supplemental Digital Content 5) [29].
Outcome measures
The primary outcomes were the mean difference in CDVA and Kmax from baseline to 12-month follow-up. This timeframe was assessed since 12 months was the most consistently reported in the included studies. Secondary outcomes included uncorrected distance visual acuity (UDVA), central corneal thickness (CCT), and adverse events.
Statistical analysis
A meta-analysis was performed using a random-effects model to determine the weighted effect estimation. Possible heterogeneity between studies was measured with the I2 statistic. Statistical analysis and meta-analysis were performed using Review Manager (open-source desktop v5.4) developed by Cochrane Collaborations. A p-value less than 0.05 was considered statistically significant.
Results
Study selection
The search yielded 887 publications after duplicates were removed. The search results were screened with 88 full texts assessed for eligibility, leaving 27 included studies for the systematic review (Fig. 1). A meta-analysis was performed on various subsets based on matching the variables and follow-up time periods. Records were excluded for several reasons including wrong intervention, study design, comparator, outcomes, and population.
The patient demographics for each study are shown in Table 1. The included studies contained a total of 1399 patients with keratoconus with 1622 eyes either treated with epithelium-off or epithelium-on CXL. The overall mean age was 25.5 (SD 4.02) years with follow up ranging from 1 week to 5 years. There were 49.3% of all eyes had epithelium-off CXL.
Primary outcomes
The corrected distance visual acuity (CDVA) improved from baseline to 12-month follow-up in both epithelium-off and epithelium-on CXL (Fig. 2A). The adjusted mean difference of CDVA between epithelium-off and epithelium-on CXL at 12-month follow-up was − 0.02 logMAR (95% CI − 0.06, 0.02; p = 0.31). The Kmax decreased in both epithelium-off and epithelium-on CXL from baseline to 12-month follow-up (Fig. 2B). However, the Kmax mean difference was not significant between the epithelium-off and epithelium-on CXL at 12-month follow-up which was − 0.59D (95% CI − 2.26, 1.08; p = 0.49). Heterogeneity between studies was high (I2 = 100%; p <0.01).
Secondary outcomes
The uncorrected distance visual acuity (UDVA) significantly improved in the epithelium-off compared to the epithelium-on group CXL (Fig. 3A). The UDVA adjusted mean difference was − 0.11 logMAR (95% CI − 0.12, − 0.1; p <0.001). Heterogeneity between studies was high (I2 = 96%; p <0.01). The reduction in mean central corneal thickness (CCT) was significantly higher in the epithelium-off group compared to the epithelium-on CXL group (Fig. 3B). The adjusted mean difference in CCT between the CXL protocols was − 3.23μm (95% CI − 4.64, − 1.81; p <0.001). Heterogeneity between studies was high (I2 = 86%; p <0.01).
Adverse events were not reported in 20 studies out of the total 27 studies included in the systematic review. There were 7 studies that described complications or adverse events, and each varied in reporting, follow up, and management (Table 2). Overall, there were more adverse events described in the epithelium-off CXL group compared to the epithelium-on CXL group. In the epithelium-on CXL group, there was no adverse events reported except in Salah 2019 [49] and Badawi 2021 [35] with mild corneal haze.
Adverse events included corneal haze, scarring, sterile infiltrates, epithelial defect, and herpes keratitis. Corneal haze was the most common of the adverse events reported in the epithelium-off CXL group. Badawi et al. [35] measured corneal haze both subjectively and objectively at 3-, 6-, and 12-month follow-up. It was found that the epithelium-on CXL group had a lower corneal haze incidence, with a better and quicker recovery. It was observed that there was one case of an epithelial defect which resolved and completely closed by the third postoperative day. There was one case of delayed epithelial healing which resulted at 3 months in a stromal haze and at 6 months deep stroma haze.
Discussion
This systematic review and meta-analysis compared the efficacy and safety of epithelium-off versus epithelium-on CXL in the treatment of keratoconus. Both techniques were effective at improving the visual acuity and keratometry outcomes. However, the primary outcomes showed no significant difference between epithelium-off and epithelium-on CXL after 12 months based on CDVA or Kmax. The UDVA improved more in the epithelium-off CXL (mean difference in gain of − 0.11D 95% CI − 0.12, − 0.1; p < 0.001) and CCT reduction was higher in the epithelium-off CXL (mean difference between the protocols − 3.23 μm, 95% CI − 4.64, − 1.81; p <0.001). Adverse events were reported in an average of 26.7% in epithelium-off and 3.3% in epithelium-on CXL (p < 0.05). The study findings support both CXL techniques as safe and effective for patients with keratoconus at 12 months.
Our findings comparing epithelium-off and epithelium-on CXL are representative of and consistent with previously reported studies. A Cochrane systematic review and meta-analysis showed no difference in Kmax and demonstrated epithelium-off had more adverse events [20]. A meta-analysis by Zhang et al. demonstrated no significant difference in CDVA or Kmax but also showed a significant difference in CCT (mean difference in change 4.53; 95% CI 0.42, 8.64; p = 0.03) to a similar effect size evaluated in our study [56]. Meanwhile, D’Oria et al. demonstrated a CDVA mean difference between epithelium-off and epithelium-on CXL of 0.07logMAR (CI 0.04, 0.1; p < 0.001). Epithelium-on CXL was shown to have significant less risk of delay in epithelial healing (p = 0.035) and persistent stromal haze (p = 0.026). Although no significant differences in UDVA, Kmax, and CCT [57]. Most studies did not include adverse events although those that did reported a higher incidence in epithelium-off CXL compared to epithelium-on CXL. The lack of reported adverse events highlights an area for further research.
While the method of epithelium-off CXL followed the Dresden protocol, there was variation in the epithelium-on CXL protocol methodology. For example, there was variation in the methods used to increase epithelial permeability of riboflavin in the epithelium-on CXL group for example Al Fayez et al. [33] used benzalkonium chloride, Soeteres et al. [50] used Ricrolin TE solution, and Rush et al. [48] used benzalkonium chloride and hydroxypropyl methylcellulose. There was considerable heterogeneity within the primary and secondary outcomes in comparing epithelium-on and epithelium-off CXL. Adverse events were only reported in 7 out of 19 included studies. This suggests that there is a lack of reporting standards in the literature. In the studies describing adverse events, there was discrepancies in the follow-up and treatment.
The rationale for epithelial removal during CXL has been to facilitate the diffusion of riboflavin into the corneal stroma. It has been suggested that the corneal biomechanical rigidity in rabbits’ eyes following epithelium-on CXL is one-fifth of that following epithelium-off CXL [58]. Leaving the epithelium intact may decrease the risks of microbial keratitis, delayed re-epithelialisation, discomfort, haze, corneal edema, glare, and thinning of the cornea [16, 17]. In studies evaluating epithelium-on CXL, minimal haze has been reported. In standard epithelium-off CXL haze occurs frequently as the epithelium is removed triggering keratocyte apoptosis and proliferation of myofibroblasts [37]. There have been concerns as to the effectiveness of epithelium-on CXL as the epithelium acts as a barrier to diffusion of riboflavin. Methods including iontophoresis or ways to enhance the chemical permeability, for example, using benzalkonium chloride have been trialled to overcome the barriers to riboflavin diffusion with an intact epithelium [59].
The strength of our study was that, to our knowledge, it is the most comprehensive systematic review and meta-analysis that compares epithelium-off to epithelium-on CXL in keratoconus. The natural course of keratoconus is life long and this systematic review and meta-analysis focused on 12-month follow-up. It has been demonstrated that outcomes can continue to change over time in CXL such that future studies should include medium to long-term outcomes. Recently, the five-year CXL outcomes were published from the Save Sight Keratoconus Registry which showed CXL was effective in stabilizing keratoconus up to 5 years in most patients [60]. This systematic review and meta-analysis were limited by the quality of the studies included, heterogeneity, biases, small sample size, and short-term follow-up. Our study was also limited by the heterogeneity of the included studies. There have been very few studies that have investigated the adverse events of epithelium-off and epithelium-on CXL with limited data reported on the adverse event described, along with variable follow-up times and different approaches in management. The complete picture of the safety and efficacy of epithelium-off vs. epithelium-on CXL is still emerging. Our findings may provide a foundation for future studies of epithelium off vs. on CXL.
Conclusion
In summary, both epithelium-off and epithelium-on CXL groups were effective in improving visual and keratometry outcomes. The primary purpose of CXL is to stop or slow the progression and stabilize keratoconus which both techniques effectively achieved. There was no difference at 12-month follow-up in terms of CDVA and Kmax. Further research is needed to compare the long-term safety and efficacy between the two techniques.
References
Espandar L, Meyer J (2010) Keratoconus: overview and update on treatment. Middle East Afr J Ophthalmol 17:15–20. https://doi.org/10.4103/0974-9233.61212
Mohammad N, Mohammad Taher R, Parviz Z (2017) Intereye asymmetry in bilateral keratoconus, keratoconus suspect and normal eyes and its relationship with disease severity. Br J Ophthalmol 101:1475. https://doi.org/10.1136/bjophthalmol-2016-309841
Santodomingo-Rubido J, Carracedo G, Suzaki A, Villa-Collar C, Vincent SJ, Wolffsohn JS (2022) Keratoconus: an updated review. Cont Lens Anterior Eye 45:101559. https://doi.org/10.1016/j.clae.2021.101559
Gorskova EN, Sevost'ianov EN (1998) Epidemiology of keratoconus in the Urals. Vestn oftalmol 114:38–40
Jonas JB, Nangia V, Matin A, Kulkarni M, Bhojwani K (2009) Prevalence and associations of keratoconus in rural Maharashtra in Central India: the Central India eye and medical study. Am J Ophthalmol 148:760–765. https://doi.org/10.1016/j.ajo.2009.06.024
Hwang S, Lim DH, Chung T-Y (2018) Prevalence and incidence of keratoconus in south korea: a nationwide population-based study. Am J Ophthalmol 192:56–64. https://doi.org/10.1016/j.ajo.2018.04.027
Kandel H, Pesudovs K, Watson SL (2020) Measurement of quality of life in keratoconus. Cornea 39. https://doi.org/10.1097/ICO.0000000000002170
Kandel H, Chen JY, Sahebjada S, Chong EW, Wiffen S, Watson SL (2022) Cross-linking improves the quality of life of people with keratoconus: a cross-sectional and longitudinal study from the Save Sight Keratoconus Registry. Cornea. https://doi.org/10.1097/ICO.0000000000003185
Garcia-Ferrer FJ, Akpek EK, Amescua G, Farid M, Lin A, Rhee MK, Varu DM, Musch DC, Mah FS, Dunn SP (2019) Corneal ectasia preferred practice pattern®. Ophthalmology 126:P170–P215. https://doi.org/10.1016/j.ophtha.2018.10.021
Hersh PS, Greenstein SA, Fry KL (2011) Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg 37. https://doi.org/10.1016/j.jcrs.2010.07.030
Kandel H, Abbondanza M, Gupta A, Mills R, Watson AS, Petsoglou C, Kerdraon Y, Watson SL (2023) Comparison of standard versus accelerated corneal collagen cross-linking for keratoconus: 5-year outcomes from the Save Sight Keratoconus Registry. Eye. https://doi.org/10.1038/s41433-023-02641-6
Vohra V, Tuteja S, Gurnani B, Chawla H (2023) Collagen cross linking for keratoconus. StatPearls Publishing
Arbelaez MC, Sekito MB, Vidal C, Choudhury SR (2009) Collagen cross-linking with riboflavin and ultraviolet-A light in keratoconus: one-year results. Oman J Ophthalmol 2:33–38. https://doi.org/10.4103/0974-620x.48420
Ng SM, Ren M, Hawkins BS, Kuo IC (2021) Transepithelial Versus epithelium-off corneal crosslinking for progressive keratoconus. Cochrane Database Syst Rev. https://doi.org/10.1016/j.ajo.2021.05.009
Borchert GA, Watson SL, Kandel H (2022) Oxygen in corneal collagen crosslinking to treat keratoconus: a systematic review and meta-analysis. Asia Pac J Ophthalmol (Phila) 11. https://doi.org/10.1097/APO.0000000000000555
Razmjoo H, Rahimi B, Kharraji M, Koosha N, Peyman A (2014) Corneal haze and visual outcome after collagen crosslinking for keratoconus: a comparison between total epithelium off and partial epithelial removal methods. Adv Biomed Res 3:221–221. https://doi.org/10.4103/2277-9175.145677
Arance-Gil Á, Villa-Collar C, Pérez-Sanchez B, Carracedo G, Gutiérrez-Ortega R (2021) Epithelium-Off vs. transepithelial corneal collagen crosslinking in progressive keratoconus: 3 years of follow-up. J Opt 14:189–198. https://doi.org/10.1016/j.optom.2020.07.005
Khoo P, Cabrera-Aguas M, Watson SL (2021) Microbial keratitis after corneal collagen cross-linking for corneal ectasia. Asia Pac J Ophthalmol (Phila) 10. https://doi.org/10.1097/APO.0000000000000379
Spoerl E, Hoyer A, Pillunat LE, Raiskup F (2011) Corneal cross-linking and safety issues. Open Ophthalmol J 5:14–16. https://doi.org/10.2174/1874364101105010014
Ng SM, Ren M, Lindsley KB, Hawkins BS, Kuo IC (2021) Transepithelial versus epithelium-off corneal crosslinking for progressive keratoconus. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD013512.pub2
Kobashi H, Rong SS, Ciolino JB (2018) Transepithelial versus epithelium-off corneal crosslinking for corneal ectasia. J Cataract Refract Surg 44:1507–1516. https://doi.org/10.1016/j.jcrs.2018.08.021
Li W, Wang B (2017) Efficacy and safety of transepithelial corneal collagen crosslinking surgery versus standard corneal collagen crosslinking surgery for keratoconus: a meta-analysis of randomized controlled trials. BMC Ophthalmol 17:262. https://doi.org/10.1186/s12886-017-0657-2
Wen D, Song B, Li Q, Tu R, Huang Y, Wang Q, McAlinden C, O’Brart D, Huang J (2018) Comparison of epithelium-off versus transepithelial corneal collagen cross-linking for keratoconus: a systematic review and meta-analysis. Cornea 37:1018-1024. https://doi.org/10.1097/ICO.0000000000001632
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
NHMRC (2019) Guidelines for guidelines: assessing risk of bias. Australian Government
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan A-W, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
McGuinness LA, Higgins JPT (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12:55–61. https://doi.org/10.1002/jrsm.1411
Hamida Abdelkader SM, Fernández J, Rodríguez-Vallejo M, Sánchez-García A, Piñero DP (2021) Comparison of different methods of corneal collagen crosslinking: a systematic review. Semin Ophthalmol 36:67–74. https://doi.org/10.1080/08820538.2021.1890784
Abdel-Radi M, Eldaly Z, Abdelmotaal H, Abdelrahman R, Sayed M, Soliman K (2020) Correlation between corneal demarcation line depth in epithelium-off and trans-epithelium accelerated corneal cross linking and keratoconus progression. Int J Ophthalmol 13:907–912. https://doi.org/10.18240/ijo.2020.06.08
Akbar B, Intisar-Ul-Haq R, Ishaq M, Arzoo S, Siddique K (2017) Transepithelial corneal crosslinking in treatment of progressive keratoconus: 12 months’ clinical results. Pak J Med Sci 33:570–575. https://doi.org/10.12669/pjms.333.11907
Al Fayez MF, Alfayez S, Alfayez Y (2015) Transepithelial versus epithelium-off corneal collagen cross-linking for progressive keratoconus: a prospective randomized controlled trial. Cornea 34. https://doi.org/10.1097/ICO.0000000000000547
Al Zubi K, Albakar Y, Nasser R (2019) Transepithelial epithelium off crosslinking for treating keratoconus among Jordanians. Open J Ophthalmol 13. https://doi.org/10.2174/1874364101913010008
Badawi AE (2021) Corneal haze and densitometry in keratoconus after collagen cross-linking by three different protocols. J Curr Ophthalmol 33:422–430. https://doi.org/10.4103/joco.joco_145_21
Çerman E, Özcan DÖ, Toker E (2017) Sterile corneal infiltrates after corneal collagen cross-linking: evaluation of risk factors. Acta Ophthalmol 95:199–204. https://doi.org/10.1111/aos.13218
Cifariello F, Minicucci M, Di Renzo F, Di Taranto D, Coclite G, Zaccaria S, De Turris S, Costagliola C (2018) Epi-off versus epi-on corneal collagen cross-linking in keratoconus patients: a comparative study through 2-year follow-up. J Ophthalmol 2018:4947983. https://doi.org/10.1155/2018/4947983
Godefrooij DA, Boom K, Soeters N, Imhof SM, Wisse RPL (2017) Predictors for treatment outcomes after corneal crosslinking for keratoconus: a validation study. Int Ophthalmol 37:341–348. https://doi.org/10.1007/s10792-016-0262-z
Huang JR, Liao HF, Wan CH, Gong LM, He LF, Jiang HJ, Li B, Shao Y (2020) Three-year clinical observation of the outcomes of transepithelial and epithelial-off accelerated corneal collagen crosslinking treatment for different types of progressive keratoconus. Exp Ther Med 20:786–795. https://doi.org/10.3892/etm.2020.8741
Kocak I, Aydin A, Kaya F, Koc H (2014) Comparison of transepithelial corneal collagen crosslinking with epithelium-off crosslinking in progressive keratoconus. J Fr Ophtalmol 37:371–376. https://doi.org/10.1016/j.jfo.2013.11.012
Madeira C, Vasques A, Beato J, Godinho G, Torrão L, Falcão M, Falcão-Reis F, Pinheiro-Costa J (2019) Transepithelial accelerated versus conventional corneal collagen crosslinking in patients with keratoconus: a comparative study. Clin Ophthalmol 13:445–452. https://doi.org/10.2147/opth.S189183
Nawaz S, Gupta S, Gogia V, Sasikala NK, Panda A (2015) Trans-epithelial versus conventional corneal collagen crosslinking: a randomized trial in keratoconus. Oman J Ophthalmol 8:9–13. https://doi.org/10.4103/0974-620x.149855
Nicula CA, Rednik AM, Bulboacă AE, Nicula D (2019) Comparative results between “epi-off” conventional and accelerated corneal collagen crosslinking for progressive keratoconus in pediatric patients. Ther Clin Risk Manag 15:1483–1490. https://doi.org/10.2147/tcrm.S224533
Niyazmand H, McKelvie J, Li Y, McLintock C (2021) Comparison of visual and tomographic outcomes of epithelium-on and epithelium-off accelerated corneal crosslinking: a longitudinal study. Cornea 40. https://doi.org/10.1097/ICO.0000000000002567
Ouyang BW, Ding H, Wang H, Yang ZD, Zhong T, Fan HM, Zhong XW (2021) Comparison of corneal biological parameters between transepithelial and epithelium-off corneal cross-linking in keratoconus. Int J Ophthalmol 14:998–1005. https://doi.org/10.18240/ijo.2021.07.06
Rossi S, Orrico A, Santamaria C, Romano V, De Rosa L, Simonelli F, De Rosa G (2015) Standard versus trans-epithelial collagen cross-linking in keratoconus patients suitable for standard collagen cross-linking. Clin Ophthalmol 9:503–509. https://doi.org/10.2147/opth.S73991
Rossi S, Santamaria C, Boccia R, De Rosa L, D’Alterio FM, Simonelli F, De Rosa G (2018) Standard, transepithelial and iontophoresis corneal cross-linking: clinical analysis of three surgical techniques. Int Ophthalmol 38:2585–2592. https://doi.org/10.1007/s10792-017-0772-3
Sloan WR, Ryan BR (2017) Epithelium-off versus transepithelial corneal collagen crosslinking for progressive corneal ectasia: a randomised and controlled trial. Br J Ophthalmol 101:503. https://doi.org/10.1136/bjophthalmol-2016-308914
Salah Y, Omar K, Sherif A, Azzam S (2019) Study of demarcation line depth in transepithelial versus epithelium-off accelerated cross-linking (AXL) in keratoconus. J Ophthalmol 2019:3904565. https://doi.org/10.1155/2019/3904565
Soeters N, Wisse RPL, Godefrooij DA, Imhof SM, Tahzib NG (2015) Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial. Am J Ophthalmol 159:821–828.e823. https://doi.org/10.1016/j.ajo.2015.02.005
Spadea L, Salvatore S, Paroli MP, Vingolo EM (2015) Recovery of corneal sensitivity after collagen crosslinking with and without epithelial debridement in eyes with keratoconus. J Cataract Refract Surg 41. https://doi.org/10.1016/j.jcrs.2014.06.030
Spadea L, Di Genova L, Tonti E (2018) Corneal stromal demarcation line after 4 protocols of corneal crosslinking in keratoconus determined with anterior segment optical coherence tomography. J Cataract Refract Surg 44
Stojanovic A, Zhou W, Utheim TP (2014) Corneal collagen cross-linking with and without epithelial removal: a contralateral study with 0.5% hypotonic riboflavin solution. BioMed Research International 2014: 619398. https://doi.org/10.1155/2014/619398
Yuksel E, Bektas C, Bilgihan K (2015) Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial. Am J Ophthalmol 160:399–400. https://doi.org/10.1016/j.ajo.2015.05.022
Yuksel E, Cubuk MO, Yalcin NG (2020) Accelerated epithelium-on or accelerated epithelium-off corneal collagen cross-linking: contralateral comparison study. Taiwan J Ophthalmol 10. https://doi.org/10.4103/tjo.tjo_11_19
Zhang X, Zhao J, Li M, Tian M, Shen Y, Zhou X (2018) Conventional and transepithelial corneal cross-linking for patients with keratoconus. PLoS One 13:e0195105. https://doi.org/10.1371/journal.pone.0195105
D’Oria F, Palazón A, Alio JL (2021) Corneal collagen cross-linking epithelium-on vs. epithelium-off: a systematic review and meta-analysis. Eye Vis (Lond) 8:34. https://doi.org/10.1186/s40662-021-00256-0
Wollensak G, Hammer CM, Spörl E, Klenke J, Skerl K, Zhang Y, Sel S (2014) Biomechanical efficacy of collagen crosslinking in porcine cornea using a femtosecond laser pocket. Cornea 33. https://doi.org/10.1097/ICO.0000000000000059
Conde Penedo A, Díaz Tomé V, Fernández Ferreiro A, González Barcia M, Otero Espinar FJ (2021) Enhancement in corneal permeability of riboflavin using cyclodextrin derivates complexes as a previous step to transepithelial cross-linking. Eur J Pharm Biopharm 162:12–22. https://doi.org/10.1016/j.ejpb.2021.02.012
Ferdi AC, Kandel H, Nguyen V, Tan J, Arnalich-Montiel F, Abbondanza M, Watson SL (2023) Five-year corneal cross-linking outcomes: a Save Sight Keratoconus Registry Study. Clin Exp Ophthalmol 51:9–18. https://doi.org/10.1111/ceo.14177
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions H Kandel is supported by the Kornhauser Research Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Grace A. Borchert and Himal Kandel are joint first authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borchert, G.A., Kandel, H. & Watson, S.L. Epithelium-on versus epithelium-off corneal collagen crosslinking for keratoconus: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 262, 1683–1692 (2024). https://doi.org/10.1007/s00417-023-06287-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06287-8