Abstract
Purpose
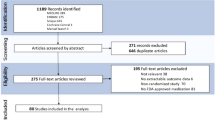
To evaluate long-term results of accelerated corneal cross-linking (ACXL) in patients with progressive keratoconus, seventy-four eyes of 53 patients with progressive keratoconus (documented Kmax progression > 1D/a) who underwent ACXL (18mW/cm2 for 5 min) were included in a retrospective observational clinical study. The investigation focused on tomographic and keratometric parameters, refractive data, and visual outcomes at 5 years follow-ups.
Methods
Corrected distance visual acuity (CDVA), slit lamp, and Pentacam® examinations were conducted, including assessments of thinnest corneal point (TP), minimum radius (Rmin), corneal astigmatism, and maximum anterior keratometry (Kmax). These examinations were performed two weeks before the surgery and, on average, 56 months after the surgery. In a subgroup of 24 eyes, Pentacam® examination data from an intermediate visit at 12 months until the final visit was evaluated to confirm continuous stability.
The ACXL protocol included corneal abrasion, hydroxypropylmethylcellulose (HPMC)-riboflavin eye drops administered every 5 min for a total duration of 30 min, and irradiation with 18mW/cm2 for 5 min using riboflavin eye drops applied every minute during the irradiation process. Intraoperatively, minimal corneal pachymetry of > 400 µm was ensured in every patient.
Results
After 56 months, all values exhibited statistically significant changes (paired t-test; CDVA p = 0.002; Kmax p < 0.001; Rmin p < 0.001; astigmatism p = 0.03; TP p < 0.001).
In the subgroup analysis of 24 eyes, which included tomographical and keratometric parameters, no statistically significant changes were observed during the last 12 months of observation (paired t-test; Kmax p = 0.72; Rmin p = 0.67; astigmatism p = 0.72).
Treatment failure was strictly defined as an increase in Kmax (> 1D) during the 5-year follow-up and was observed in only 3 eyes (4%).
Conclusions
ACXL is an effective and safe treatment for patients with progressive keratoconus. Our results demonstrate improvements in functional and tomographical outcomes even after high-energy ACXL (18mW/cm2 for 5 min) over a long-term period of 56 months. Our analysis indicates stable conditions in previously progressive keratoconus, particularly during the final year of the observation period. The treatment failure rate was 4%.

Similar content being viewed by others
Introduction
The group of ectatic diseases includes keratoconus, pellucid marginal degeneration, keratoglobus, and post-refractive surgery progressive corneal ectasia. The pathophysiology of keratoconus is multifactorial and involves genetic, environmental, biomechanical, and biochemical factors [1]. The mean age at diagnosis is reported to be 28 years, with an incidence of 1:7500 [2].
Disease-defining parameters of ectatic diseases include corneal thinning, posterior or combined posterior-anterior ectasia, and abnormal corneal thickness distribution [1, 3, 4]. These parameters are best diagnosed using tomographical examinations such as Scheimpflug or optical coherence tomography [4].
More recent corneal tomography techniques allow for the confirmation of corneal ectasia at a very early stage, enabling the diagnosis of even mild or subclinical keratoconus [4, 5]. This advancement enables ophthalmologists to initiate therapy before severe irregular astigmatism of the cornea, corneal scarring, or Descemet's membrane rupture can lead to impaired vision [3].
Classic and symptomatic treatment include refractive correction using gas-permeable contact lenses, special cone-design lenses, soft lenses, and even scleral and hybrid lenses [6].
The primary goal of interventional keratoconus therapy is to halt disease progression, making early treatment crucial for better long-term visual acuity [5]. However, in patients with good baseline visual acuity, a thorough risk–benefit analysis of interventional treatment is essential. Modified techniques of Corneal Crosslinking (CXL), known as accelerated Corneal Crosslinking (ACXL), have been developed to reduce the instantaneous complications associated with conventional CXL techniques, such as endothelial-related side effects and time-related discomfort. Consequently, the timing of intervention has gradually shifted to earlier disease stages [4, 7]. Nonetheless, there is an ongoing discussion regarding the efficacy of ACXL compared to traditional CXL.
The purpose of this monocentric exploratory study is to evaluate the long-term results of ACXL (18mW/cm2 for 5 min) in patients with progressive keratoconus.
Material and methods
The original Dresden protocol for corneal cross-linking (CXL) involves central corneal abrasion and the application of photosensitizing 0.1% riboflavin (10 mg riboflavin-5-phosphate in 10 ml Dextran-T-500 20% solution) eye drops. Once the riboflavin has completely penetrated the cornea, irradiation is initiated and continued for 30 min using UVA light at a power density of 3mW/cm2. During irradiation, riboflavin eye drops are applied every 5 min, resulting in a total dose of 5.4 J/cm2 [8].
The ACXL protocol investigated in this study involved sterile mechanical abrasion of the central corneal epithelium (epi-off CXL) after local anesthesia. Subsequently, riboflavin eye drops (0.1% riboflavin in hydroxypropyl-methylcellulose = HPMC; VibeX Rapid; Avedro Inc.) were applied every 4–5 min for 30 min. Prior to irradiation, minimal corneal pachymetry of > 400 µm was ensured in every patient by using a hypoosmolar solution (MedioCROSS® H, Avedro Inc.) to swell the cornea for 2 min every 20 s in case the corneal thickness was < 400 µm at the thinnest corneal point (TP) until a sufficient pachymetry > 400 µm was achieved. Corneal irradiation was performed using a power density of 18mW/cm2 (CCL 365 vario, Peschke, Meditrade, Huenenberg, Switzerland) for 5 min, resulting in a total dose of 5.4 J/cm2. During irradiation, iso-osmolar riboflavin eye drops were applied every minute, and the limbal region was excluded. Finally, a sterile contact lens was applied in combination with levofloxacin eye drops.
A total of 74 eyes from 53 patients with documented progressive keratoconus were included in a retrospective observational clinical study. Progressive keratoconus was defined as the annual progression of the steepest radius of curvature of the anterior corneal surface (maximum anterior keratometry = Kmax) exceeding 1 diopter (D) [9]. The patients underwent accelerated corneal cross-linking (ACXL) at the Department of Ophthalmology, Klinikum rechts der Isar, Technical University of Munich (TUM), between February 2013 and June 2017. The ACXL procedure involved UVA radiation (365 nm, CCL-365 vario, Peschke Meditrade, Huenenberg, Switzerland) at a power density of 18mW/cm2 for a duration of 5 min.
Exclusion criteria were defined as TP < 400 µm, post-LASIK ectasia, pellucid marginal degeneration, corneal infection, corneal scars that could interfere with tomographical examination, prior corneal surgery, prior penetrating trauma, prior rupture of the Descemet’s membrane, additional diseases such as glaucoma or aphakia, pregnancy, and breastfeeding [10].
Written consent according to the principles of the Declaration of Helsinki was received by all patients.
The investigation focused on tomographical and keratometric parameters, refractive data, and visual outcomes during the 5-year follow-up period. Demographic values including gender, age, localization, and bilateralism were collected pre-interventionally. Corrected distance visual acuity (CDVA), slit lamp exams, and tomographical examinations were performed two weeks before and on average 56 months after surgery. Tomographical examination, using a Scheimpflug device (Pentacam® HR 70700, Oculus, Wetzler, Germany) included the thinnest corneal point (TP), minimum anterior radius (Rmin), corneal astigmatism and maximum anterior keratometry (Kmax). Pentacam® examination data from an intermediate visit conducted 12 months before the patient's final visit were evaluated in a subgroup of 24 eyes. This analysis aimed to confirm the continuous stability of the parameters, both overall and towards the end of the observed time span. All values were tabulated using Microsoft Excel (Microsoft Corporation, Redmond, Washington, USA).
For patients using rigid gas-permeable contact lenses, it was advised that they refrain from wearing their lenses for a minimum of 4 weeks before the tomographical examination. In the case of patients wearing soft contact lenses, they were requested to abstain from wearing them for at least 2 weeks prior to the examination.
To evaluate the postoperative development of CDVA, TP, Rmin, corneal astigmatism, and Kmax, paired t-test was performed, using the statistical software of IBM®-SPSS (International Business Machines Corporation, Armonk, New York, USA). The level of significance was set at 5%.
Results
The gender distribution of the study population consisted of 41 male and 12 female patients, with an average age of 33 years (minimum = 19 years, maximum = 59 years). A total of 74 eyes were examined, with 35 being right eyes and 39 being left eyes. Among the patients, 21 individuals received treatment in both eyes.
The average time to final postoperative visit was 56 months (minimum = 28 months; maximum = 81 months). At an intermediate visit on average 12 months (minimum = 8 months, maximum = 17 months) prior to the most recent postoperative visit, the tomographical examination was performed in 24 eyes (9 right eyes, 15 left eyes) of 19 patients.
Preoperative CDVA was 0.23 logMAR (SD = 0.22), preoperative Rmin was 6.2 mm (SD = 0.7 mm), preoperative corneal astigmatism was 3.5D (SD = 2.0D), preoperative Kmax was 54.9D (SD = 6.4D) and preoperative TP was 463.1 µm (SD = 37.3 µm).
Postoperatively 53 (= 72%) eyes showed an improvement of visual acuity and 21 (= 28%) eyes showed a deterioration of visual acuity, whereas 16 (= 76%) eyes showed a deterioration of + 0.1 logMAR or less. In 3 (= 14%) eyes a deterioration of + 0.15 logMAR was observed, in 1 eye (= 5%) + 0.2 logMAR and in 1 eye (= 5%) + 0.3 logMAR.
All of the following values improved statistically significantly after 56 months (paired t-test): postoperative CDVA was 0.15 (SD = 0.10; p = 0.001) (Fig. 1), postoperative Rmin was 6.3 mm (SD = 0.7 mm; p < 0.001) (Fig. 2), postoperative corneal astigmatism was 3.3D (SD = 1.7D; p = 0.03) (Fig. 3) and postoperative Kmax was 53.9D (SD = 6.0D; p < 0.001) (Fig. 4). Postoperative TP decreased by 7.1 µm (SD = 38.3 µm; p < 0.001) (Fig. 5). All values are shown in Table 1.
The subgroup analysis of 24 eyes from 19 patients, who underwent an examination 12 months prior to their postoperative visit, revealed no statistically significant changes in tomographical values compared to their final postoperative data. The paired t-test analysis showed p-values of 0.27 for TP (thinnest corneal point), 0.67 for Rmin (minimum radius), 0.72 for corneal astigmatism, and 0.72 for Kmax (maximum anterior keratometry).
Treatment failure was rigorously defined by a total increase of Kmax > 1.0D during the complete postoperative follow-up and occurred only in 3 eyes (= 4%). All three cases had initial Kmax < 55D. Progression of Kmax was still < 2D (1.5D, 1.1D, and 1.4D). The age of these three patients ranged between 23 and 30 years.
Discussion
According to the Bunsen-Roscoe law, the photochemical effect on a tissue is determined by the product of the physical intensity of the flash and its duration. However, it should be noted that this law may not be entirely applicable to corneal tissue due to the limited number of crosslinking points within the cornea and the capacity for oxygen diffusion within the stroma [11, 12].
In ex vivo studies, it has been demonstrated that adequate corneal stiffness can be achieved even with irradiation levels as high as 45mW/cm2 for 2 min [13]. Shorter treatment durations offer increased patient comfort and allow for higher patient throughput. Importantly, the incidence of early negative effects, such as sterile infiltrates (7%), delayed epithelial healing (6%), bacterial infection (3%), and stromal scars (2%), does not appear to be higher when compared to conventional CXL following the Dresden protocol [10, 14].
Previous studies have proven similar efficacy of ACXL (18mW/cm2 for 5 min) compared to CXL following Dresden protocol after a follow-up time of six months to two years [15,16,17,18,19]. Further studies investigated very high-energy ACXL with irradiation of 30mW or more [20, 21]. Numerous long-term observations have been reported investigating ACXL with irradiation of 9mW/cm2 for 10 min [22,23,24,25,26]. By increasing the irradiation energy and thus lowering exposure time a more anterior demarcation line in OCT has been shown, raising the debate of less effective crosslinking, especially since a faster depletion of available oxygen molecules due to the increased irradiation is suspected [27, 28]. Recent research has been going into improving accelerated crosslinking efficacy by modifying the amount of available oxygen to compensate for these effects [29]. It is therefore of ongoing importance to prove the real-life efficacy of the different high-energy ACXL settings in stabilizing Keratoconus over prolonged observation times.
To the best of our knowledge, the present work is the first one to show the efficacy of HPMC-riboflavin ACXL with irradiation of 18mW/cm2 for 5 min after a long-term follow-up of 56 months. Hashemi et al. evaluated long-term follow-up after Dextran-riboflavin ACXL (18mW/cm2) showing a reduction of Kmax of 0.36D to 0.37D. Our results show a reduction of Kmax of 1D after 56 months. Hashemi et al. used Dextran-solution eye drops instead of HPMC-solution eye drops to apply riboflavin [30].
As mentioned earlier, accelerated corneal crosslinking (ACXL) has been associated with a shallower demarcation line compared to the conventional crosslinking protocol [31]. However, the use of hydroxypropylmethylcellulose (HPMC) solution in ACXL allows for faster intrastromal diffusion of riboflavin, resulting in a deeper demarcation line. This deeper demarcation line has been shown to lead to greater topographic flattening compared to ACXL with dextran solution [27, 32]. Studies have also reported greater topographic flattening after ACXL in patients with initially steeper corneas (Kmax 54.0D or more) [28, 33, 34]. Additionally, ACXL appears to be more effective in preventing progression in patients with advanced keratoconus [35]. However, concerns have been raised about the reduced total amount of generated crosslinks in ACXL, leading to suspicion of reduced long-term stability.
Our study is limited by the retrospective design with a lack of randomization and the absence of a control group due to the fact that our center switched over to ACXL early and completely, never providing conventional CXL and ACXL at the same time.
Our study findings indicate a statistically significant improvement in both functional and tomographical outcomes following high-energy ACXL (18mW/cm2 for 5 min) even after a long-term follow-up period of 56 months. Moreover, we observed stable conditions in patients with previously progressive keratoconus, including during the final year of the observation period. The treatment failure rate, defined as an increase in Kmax greater than 1D during the 5-year follow-up, was 4%. It is important to note that the limitations of our study, including the retrospective design and absence of a randomized control group, should be taken into consideration when interpreting these findings.
HPMC-riboflavin ACXL with irradiation of 18mW/cm2 for 5 min is an effective and safe treatment in patients with progressive keratoconus with no signs of fading stability for at least 4–5 years after surgery.
References
Krachmer JH, Feder RS, Belin MW (1984) Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol 28(4):293–322. https://doi.org/10.1016/0039-6257(84)90094-8
Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP (2017) Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol 175:169–172. https://doi.org/10.1016/j.ajo.2016.12.015
Romero-Jiménez M, Santodomingo-Rubido J, Wolffsohn JS (2010) Keratoconus: a review. Contact Lens Anterior Eye: J Br Contact Lens Assoc 33(4):157–66. https://doi.org/10.1016/j.clae.2010.04.006. (quiz 205)
Gomes JA, Tan D, Rapuano CJ et al (2015) Global consensus on keratoconus and ectatic diseases. Cornea 34(4):359–369. https://doi.org/10.1097/ico.0000000000000408
Belin MW, Villavicencio OF, Ambrósio RR Jr (2014) Tomographic parameters for the detection of keratoconus: suggestions for screening and treatment parameters. Eye Contact Lens 40(6):326–330. https://doi.org/10.1097/icl.0000000000000077
Lim L, Lim EWL (2020) Current perspectives in the management of keratoconus with contact lenses. Eye (London, England) 34(12):2175–2196. https://doi.org/10.1038/s41433-020-1065-z
Subasinghe SK, Ogbuehi KC, Dias GJ (2018) Current perspectives on corneal collagen crosslinking (CXL). Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 256(8):1363–84. https://doi.org/10.1007/s00417-018-3966-0
Wollensak G, Spoerl E, Seiler T (2003) Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 135(5):620–627. https://doi.org/10.1016/s0002-9394(02)02220-1
Koller T, Iseli HP, Hafezi F, Vinciguerra P, Seiler T (2009) Scheimpflug imaging of corneas after collagen cross-linking. Cornea 28(5):510–515. https://doi.org/10.1097/ICO.0b013e3181915943
Fischinger I, Seiler TG, Santhirasegaram K, Pettenkofer M, Lohmann CP, Zapp D (2018) Corneal crosslinking (CXL) with 18-mW/cm(2) irradiance and 5.4-J/cm(2) radiant exposure-early postoperative safety. Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 256(8):1521–5. https://doi.org/10.1007/s00417-018-3978-9
Bao F, Zheng Y, Liu C et al (2018) Changes in corneal biomechanical properties with different corneal cross-linking irradiances. J Refract Surg (Thorofare, NJ : 1995) 34(1):51–8. https://doi.org/10.3928/1081597x-20171025-01
Hammer A, Richoz O, Arba Mosquera S, Tabibian D, Hoogewoud F, Hafezi F (2014) Corneal biomechanical properties at different corneal cross-linking (CXL) irradiances. Invest Ophthalmol Vis Sci 55(5):2881–2884. https://doi.org/10.1167/iovs.13-13748
Wernli J, Schumacher S, Spoerl E, Mrochen M (2013) The efficacy of corneal cross-linking shows a sudden decrease with very high intensity UV light and short treatment time. Invest Ophthalmol Vis Sci 54(2):1176–1180. https://doi.org/10.1167/iovs.12-11409
Koller T, Mrochen M, Seiler T (2009) Complication and failure rates after corneal crosslinking. J Cataract Refract Surg 35(8):1358–1362. https://doi.org/10.1016/j.jcrs.2009.03.035
Hashemi H, Fotouhi A, Miraftab M et al (2015) Short-term comparison of accelerated and standard methods of corneal collagen crosslinking. J Cataract Refract Surg 41(3):533–540. https://doi.org/10.1016/j.jcrs.2014.07.030
Chow VW, Chan TC, Yu M, Wong VW, Jhanji V (2015) One-year outcomes of conventional and accelerated collagen crosslinking in progressive keratoconus. Sci Rep 5:14425. https://doi.org/10.1038/srep14425
Mesen A, Bozkurt B, Kamis U, Okudan S (2018) Correlation of demarcation line depth with medium-term efficacy of different corneal collagen cross-linking protocols in keratoconus. Cornea 37(12):1511–1516. https://doi.org/10.1097/ico.0000000000001733
Hashemian H, Jabbarvand M, Khodaparast M, Ameli K (2014) Evaluation of corneal changes after conventional versus accelerated corneal cross-linking: a randomized controlled trial. J Refract Surg (Thorofare, NJ : 1995) 30(12):837–42. https://doi.org/10.3928/1081597x-20141117-02
Shetty R, Pahuja NK, Nuijts RM et al (2015) Current protocols of corneal collagen cross-linking: visual, refractive, and tomographic outcomes. Am J Ophthalmol 160(2):243–249. https://doi.org/10.1016/j.ajo.2015.05.019
Marafon SB, Kwitko S, Marinho DR (2020) Long-term results of accelerated and conventional corneal cross-linking. Int Ophthalmol 40(10):2751–2761. https://doi.org/10.1007/s10792-020-01462-w
Zhang X, Sun L, Tian M et al (2020) Accelerated (45 mW/cm(2)) transepithelial corneal cross-linking for progressive keratoconus patients: long-term topographical and clinical outcomes. Front Med 7:283. https://doi.org/10.3389/fmed.2020.00283
Nicula CA, Rednik AM, Nicula AP, Bulboaca AE, Nicula D, Horvath KU (2021) Comparative results between “Epi-Off” accelerated and “Epi-Off” standard corneal collagen crosslinking-UVA in progressive keratoconus - 7 years of follow-up. Ther Clin Risk Manag 17:975–988. https://doi.org/10.2147/tcrm.S321410
Mazzotta C, Raiskup F, Hafezi F et al (2021) Long term results of accelerated 9 mW corneal crosslinking for early progressive keratoconus: the Siena eye-cross study 2. Eye Vision (London, England) 8(1):16. https://doi.org/10.1186/s40662-021-00240-8
Nicula CA, Nicula D, Rednik AM, Bulboacă AE (2020) Comparative results of “Epi-Off” conventional versus “Epi-Off” accelerated cross-linking procedure at 5-year follow-up. J Ophthalmol 2020:4745101. https://doi.org/10.1155/2020/4745101
Vounotrypidis E, Athanasiou A, Kortüm K et al (2018) Long-term database analysis of conventional and accelerated crosslinked keratoconic mid-European eyes. Graefe’s Arch Clin Exp Ophthalmol = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie 256(6):1165–72. https://doi.org/10.1007/s00417-018-3955-3
Godefrooij DA, Soeters N, Imhof SM, Wisse RP (2016) Corneal cross-linking for pediatric keratoconus: long-term results. Cornea 35(7):954–958. https://doi.org/10.1097/ico.0000000000000819
Hagem AM, Thorsrud A, Sandvik GF, Drolsum L (2019) Randomized study of collagen cross-linking with conventional versus accelerated UVA irradiation using riboflavin with hydroxypropyl methylcellulose: two-year results. Cornea 38(2):203–209. https://doi.org/10.1097/ico.0000000000001791
Choi M, Kim J, Kim EK, Seo KY, Kim TI (2017) Comparison of the conventional Dresden protocol and accelerated protocol with higher ultraviolet intensity in corneal collagen cross-linking for keratoconus. Cornea 36(5):523–529. https://doi.org/10.1097/ico.0000000000001165
Seiler TG, Komninou MA, Nambiar MH, Schuerch K, Frueh BE, Büchler P (2021) Oxygen kinetics during corneal cross-linking with and without supplementary oxygen. Am J Ophthalmol 223:368–376. https://doi.org/10.1016/j.ajo.2020.11.001
Hashemi H, Mohebbi M, Asgari S (2020) Standard and accelerated corneal cross-linking long-term results: A randomized clinical trial. Eur J Ophthalmol 30(4):650–657. https://doi.org/10.1177/1120672119839927
Kymionis GD, Tsoulnaras KI, Grentzelos MA et al (2014) Corneal stroma demarcation line after standard and high-intensity collagen crosslinking determined with anterior segment optical coherence tomography. J Cataract Refract Surg 40(5):736–740. https://doi.org/10.1016/j.jcrs.2013.10.029
Ehmke T, Seiler TG, Fischinger I, Ripken T, Heisterkamp A, Frueh BE (2016) Comparison of corneal riboflavin gradients using dextran and HPMC solutions. J Refract Surg 32(12):798–802. https://doi.org/10.3928/1081597x-20160920-03
Greenstein SA, Hersh PS (2013) Characteristics influencing outcomes of corneal collagen crosslinking for keratoconus and ectasia: implications for patient selection. J Cataract Refract Surg 39(8):1133–1140. https://doi.org/10.1016/j.jcrs.2013.06.007
Koller T, Pajic B, Vinciguerra P, Seiler T (2011) Flattening of the cornea after collagen crosslinking for keratoconus. J Cataract Refract Surg 37(8):1488–1492. https://doi.org/10.1016/j.jcrs.2011.03.041
Chan TC, Chow VW, Jhanji V, Wong VW (2015) Different topographic response between mild to moderate and advanced keratoconus after accelerated collagen cross-linking. Cornea 34(8):922–927. https://doi.org/10.1097/ico.0000000000000483
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethical research committee of the Technical University of Munich (TUM) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speaker’s bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Friedrich, J., Sandner, A., Nasseri, A. et al. Accelerated corneal cross-linking (18mW/cm2 for 5 min) with HPMC-riboflavin in progressive keratoconus – 5 years follow-up. Graefes Arch Clin Exp Ophthalmol 262, 871–877 (2024). https://doi.org/10.1007/s00417-023-06225-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06225-8