Abstract
Purpose
The purpose is to assess the effect of ethnicity on surgical macular hole closure.
Methods
A retrospective cohort study was undertaken in five UK National Health Service Hospitals. We included all patients with known ethnicity undergoing vitrectomy, internal limiting membrane peel, and gas/oil tamponade for all stages of primary full-thickness macular hole (FTMH). The primary outcome was anatomic success, defined as FTMH closure with one operation. The secondary outcome was mean change in best-corrected visual acuity (BCVA) comparing baseline with final review.
Results
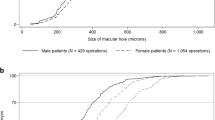
Of 334 operations, the ethnicity profile comprised 78.7% White patients, 11.7% Black patients, 8.1% Asian patients, and 1.5% in mixed/other ethnicities. Mean age was 69.7 years with 68.5% females. Overall, 280 (83.8%) had anatomic success. Anatomic failure occurred in 38.5% of Black patients versus 12.6% of White patients (relative risk: 1.788; 95% CI: 1.012 to 3.159; P = 0.045). Overall, baseline logarithm of the minimum angle of resolution BCVA improved by 0.34, from 0.95 (95% CI: 0.894 to 1.008) to 0.62 (95% CI: 0.556 to 0.676). Mean BCVA improved by 0.35 in White patients, 0.37 in Black patients, 0.23 in Asian patients, and 0.38 in mixed/other ethnicity (P = 0.689). Greater FTMH minimum linear diameter was associated with an increased risk of anatomic failure (relative risk: 1.004; 95% CI: 1.002 to 1.005; P < 0.0001), whereas better pre-operative BCVA (F [1,19] = 162.90; P < 0.0001) and anatomic success (F [1,19] = 97.69; P < 0.0001) were associated with greater BCVA improvement. Socio-economic status did not significantly influence anatomic success or BCVA change.
Conclusions
Black ethnicity is associated with an approximately twofold greater risk of failed FTMH surgery. The reasons for this difference warrant further study.


Similar content being viewed by others
References
McCannel CA, Ensminger JL, Diehl NN, Hodge DN (2009) Population-based incidence of macular holes. Ophthalmology 116(7):1366–1369
Madi HA, Masri I, Steel DH (2016) Optimal management of idiopathic macular holes. Clin Ophthalmol 10:97–116
Jackson TL, Donachie PH, Sparrow JM, Johnston RL (2013) United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 1; case mix, complications, and cataract. Eye (Lond) 27(5):644–651
Duker JS, Kaiser PK, Binder S et al (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120(12):2611–2619
Steel D, Lotery AJ (2013) Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye 27:S1–S21
Wilczyński T, Heinke A, Niedzielska-Krycia A, Jorg D, Michalska-Małecka K (2019) Optical coherence tomography angiography features in patients with idiopathic full-thickness macular hole, before and after surgical treatment. Clin Interv Aging 14:505–514
Singh AJ, Muqit MMK, Woon WH (2012) Is axial length a risk factor for idiopathic macular hole formation? Int Ophthalmol 32(4):393–396
Evans JR, Schwartz SD, McHugh JDA et al (1998) Systemic risk factors for idiopathic macular holes: a case-control study. Eye 12(2):256–259
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL (2013) United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 2, macular hole. Ophthalmol 120(3):629–634
Stalmans P, Benz MS, Gandorfer A et al (2012) MIVI-TRUST Study Group. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med 16 367(7):606–15
Singh R, Stone T (2018) Global Trends in Retina Survey: 13 Chicago, IL. American Society of Retina Specialists; 2018. www.asrs.org/content/documents/2018-global-trends-in-retina-survey-highlights-website.pdf Accessed July 30, 2021
Ezra E, Gregor ZJ (2004) Moorfields Macular Hole Study Group Report No. 1. Surgery for idiopathic full-thickness macular hole: two-year results of a randomized clinical trial comparing natural history, vitrectomy, and vitrectomy plus autologous serum: Moorfields Macular Hole Study Group Report no. 1. Arch Ophthalmol 122(2):224–36
Wakely L, Rahman R, Stephenson J (2012) A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes. Br J Ophthalmol 96(7):1003–1007
Steel DH, Donachie PHJ, Aylward GW, Laidlaw DA, Williamson TH, Yorston D (2021) BEAVRS Macular hole outcome group. Factors affecting anatomical and visual outcome after macular hole surgery: findings from a large prospective UK cohort. Eye 35(1):316–325
Gupta B, Laidlaw DA, Williamson TH, Shah SP, Wong R, Wren S (2009) Predicting visual success in macular hole surgery. Br J Ophthalmol 93(11):1488–1491
NHS Research authority. Medical Research Council. http://www.hra-decisiontools.org.uk/research/ Accessed July 30, 2021
Office for National Statistics. National Census Data. https://www.ons.gov.uk/census Accessed July 30, 2021
Murphy D, Al-Zubaidy M, Lois N, Scott N, Steel DH, Macular Hole Duration Study Group (2022) The effect of macular hole duration on surgical outcomes. An individual participant data study of randomized controlled trials. Ophthalmology. https://doi.org/10.1016/j.ophtha.2022.08.028
Sparrow JM, Taylor H, Qureshi K, Smith R, Birnie K, Johnston RL, UK EPR user group (2012) The Cataract National Dataset electronic multi-center audit of 55,567 operations: risk indicators for monocular visual acuity outcomes. Eye 26(6):821–826
Ministry of Housing, Communities & Local Government. English indices of deprivation 2019. http://imd-by-postcode.opendatacommunities.org/imd/2019. Accessed July 30, 2021
Wagner-Schuman M, Dubis AM, Nordgren RN et al (2011) Race- and sex-related differences in retinal thickness and foveal pit morphology. Invest Ophthalmol Vis Sci 52(1):625–634
Girkin CA, McGwin G Jr, Sinai MJ et al (2011) Variation in optic nerve and macular structure with age and race with spectral-domain optical coherence tomography. Ophthalmology 118(12):2403–2408
Zouache MA, Silvestri G, Amoaku WM et al (2020) Comparison of the morphology of the foveal pit between African and Caucasian populations. Transl Vis Sci Technol 9(5):24
Murphy DC, Melville HJR, George G et al (2021) The association between foveal floor measurements and macular hole size. Ophthalmol Retina 5(7):680–686
Chandra A, Lai M, Mitry D et al (2017) Ethnic variation in primary idiopathic macular hole surgery. Eye 31(5):708–712
Yorston D, Wickham L, Benson S, Bunce C, Sheard R, Charteris D (2008) Predictive clinical features and outcomes of vitrectomy for proliferative diabetic retinopathy. Br J Ophthalmol 92(3):365–368
Mastropasqua R, Luo YH, Cheah YS, Egan C, Lewis JJ, da Cruz L (2017) Black patients sustain vision loss while White and South Asian patients gain vision following delamination or segmentation surgery for tractional complications associated with proliferative diabetic retinopathy. Eye 31(10):1468–1474
Ho J, Williamson TH, Wong RS, Laidlaw DAH (2009) Beneficial visual outcome of vitrectomy and delamination surgery for tractional complications of diabetic retinopathy in a cohort of black patients. Eye 33(12):1884–1889
Hamm LM, Black J, Burn H et al (2020) Interventions to promote access to eye care for non-indigenous, non-dominant ethnic groups in high-income countries: a scoping review protocol. BMJ Open 10(6):e033775
Kirthi V, Reed KI, Gunawardena R, Alattar K, Bunce C, Jackson TL (2021) Do Black and Asian individuals wait longer for treatment? A survival analysis investigating the effect of ethnicity on time-to-clinic and time-to-treatment for diabetic eye disease. Diabetologia 64(4):749–757
Leamon S, Hayden C, Lee H et al (2014) Improving access to optometry services for people at risk of preventable sight loss: a qualitative study in five UK locations. J Public Health (Oxf) 36(4):667–673
Smiddy WE, Flynn HW Jr (2004) Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol 137(3):525–537
Ittarat M, Somkijrungroj T, Chansangpetch S, Pongsachareonnont P (2020) Literature review of surgical treatment in idiopathic full-thickness macular hole. Clin Ophthalmol 30(14):2171–2183
Fazio MA, Johnstone JK, Smith B, Wang L, Girkin CA (2016) Displacement of the lamina cribrosa in response to acute intraocular pressure elevation in normal individuals of African and European descent. Invest Ophthalmol Vis Sci 57(7):3331–3339
Fazio MA, Grytz R, Morris JS, Bruno L, Girkin CA, Downs JC (2014) Human scleral structural stiffness increases more rapidly with age in donors of African descent compared to donors of European descent. Invest Ophthalmol Vis Sci 55(11):7189–7198
Funding
AD acknowledges funding support from the National Institute for Health Research (NIHR), Applied Research Collaboration (ARC) South London at King’s College Hospital NHS Foundation Trust, the Royal College of Physicians, and the NIHR Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception were provided by TLJ, HL, and EP. Design of the work was provided by TLJ, HL, EP, LM, AD, HZ, TS, and DHS. Acquisition was done by HL, CB, LM, MR, ND, BZ, GKL, OT, HZ, TS, DHS, VK, CM, RZ, and GD. Analysis was done by HL and AD and interpretation of data for the work was done by HL, TLJ, and AD. Drafting the work or revising it critically for important intellectual content was done by all authors. Final approval of the version to be published was provided by all authors. Agreement to be accountable for all aspects of the work was provided by all authors.
Corresponding author
Ethics declarations
Ethical approval
The study used non-identifiable data collected during the course of routine clinical practice and was therefore determined to be an audit (audit registration: JBJEHX27C8) by the King’s College Hospital NHS Foundation Trust Research & Development and Audit teams. Accordingly, Research Ethics Committee approval was not required.
Informed Consent
The study used non-identifiable data collected during the course of routine clinical practice.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laviers, H., Papavasileiou, E., Bruce, C. et al. The effect of ethnicity on anatomic success following macular hole surgery: a multicentre cohort study. Graefes Arch Clin Exp Ophthalmol 261, 1535–1543 (2023). https://doi.org/10.1007/s00417-022-05950-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05950-w