Abstract
Purpose
To investigate the predictive role of serum angiopoietin-1 and angiopoietin-2 (Ang-1/Ang-2) in evaluating the severity of diabetic retinopathy (DR).
Methods
A total of 101 outpatients with type 2 diabetes mellitus (T2DM) were recruited and were further divided into the following five groups: T2DM without DR (non-DR), mild non-proliferative DR (NPDR), moderate NPDR, severe NPDR and proliferative DR (PDR) in accordance with the International Clinical Diabetic Retinopathy Guidelines. Furthermore, 101 serum samples were included in the further analysis using enzyme-linked immunosorbent assays. A receiver operating characteristic (ROC) curve was plotted to evaluate the diagnostic value of each index.
Results
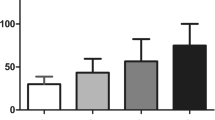
The expression of Ang-1 in the PDR group was significantly lower than that in the non-DR group, while Ang-2 showed an opposite upward trend (p < 0.05). The Ang-1/Ang-2 ratio of the non-DR group was significantly lower than that of the moderate NPDR, severe NPDR and PDR (p < 0.05, p < 0.01 and p < 0.01, respectively). Differences in the Ang-1/Ang-2 ratio were observed earlier than those in the individual Ang-1 and Ang-2 measurements. The maximal Youden index was 0.512 with a calculated area under the curve (AUC) value of 0.734 (p < 0.01).
Conclusions
The Ang-1/Ang-2 ratio was helpful in assessing the severity of DR and may provide potential clinical benefits as a biomarker and early warning signs for DR diagnosis.




Similar content being viewed by others
References
Saeedi P, Petersohn I, Salpea P et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 157:107843
Cho NH, Shaw JE, Karuranga S et al (2018) IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281
Ehrlich R, Harris A, Ciulla TA et al (2010) Diabetic macular oedema: physical, physiological and molecular factors contribute to this pathological process. Acta Ophthalmol 88:279–291
Cheung N, Mitchell P, Wong TY (2010) Diabetic retinopathy. Lancet (London, England) 376:124–136
Thomas RL, Dunstan FD, Luzio SD et al (2015) Prevalence of diabetic retinopathy within a national diabetic retinopathy screening service. Br J Ophthalmol 99:64–68
Yau JW, Rogers SL, Kawasaki R et al (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35:556–564
Thomas RL, Halim S, Gurudas S, Sivaprasad S, Owens DR (2019) IDF Diabetes Atlas: a review of studies utilising retinal photography on the global prevalence of diabetes related retinopathy between 2015 and 2018. Diabetes Res Clin Pract 157:107840
Jin G, Xiao W, Ding X et al (2018) Prevalence of and risk factors for diabetic retinopathy in a rural Chinese population: the Yangxi Eye Study. Invest Ophthalmol Vis Sci 59:5067–5073
Song P, Yu J, Chan KY, Theodoratou E, Rudan I (2018) Prevalence, risk factors and burden of diabetic retinopathy in China: a systematic review and meta-analysis. J Glob Health 8:010803
Wong TY, Cheung CM, Larsen M, Sharma S, Simó R (2016) Diabetic retinopathy Nature reviews Disease primers 2:16012
Polack S, Yorston D, López-Ramos A et al (2012) Rapid assessment of avoidable blindness and diabetic retinopathy in Chiapas, Mexico. Ophthalmology 119:1033–1040
Felcht M, Luck R, Schering A et al (2012) Angiopoietin-2 differentially regulates angiogenesis through TIE2 and integrin signaling. J Clin Invest 122:1991–2005
Lee SJ, Lee CK, Kang S et al (2018) Angiopoietin-2 exacerbates cardiac hypoxia and inflammation after myocardial infarction. J Clin Invest 128:5018–5033
Eklund L, Saharinen P (2013) Angiopoietin signaling in the vasculature. Exp Cell Res 319:1271–1280
Isidori AM, Venneri MA, Fiore D (2016) Angiopoietin-1 and Angiopoietin-2 in metabolic disorders: therapeutic strategies to restore the highs and lows of angiogenesis in diabetes. J Endocrinol Invest 39:1235–1246
Wilkinson CP, Ferris FL 3rd, Klein RE et al (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110:1677–1682
Yuan HT, Khankin EV, Karumanchi SA, Parikh SM (2009) Angiopoietin 2 is a partial agonist/antagonist of Tie2 signaling in the endothelium. Mol Cell Biol 29:2011–2022
Hackett SF, Ozaki H, Strauss RW et al (2000) Angiopoietin 2 expression in the retina: upregulation during physiologic and pathologic neovascularization. J Cell Physiol 184:275–284
Hammes HP, Lin J, Wagner P et al (2004) Angiopoietin-2 causes pericyte dropout in the normal retina: evidence for involvement in diabetic retinopathy. Diabetes 53:1104–1110
Daly C, Eichten A, Castanaro C et al (2013) Angiopoietin-2 functions as a Tie2 agonist in tumor models, where it limits the effects of VEGF inhibition. Can Res 73:108–118
Wada T, Jesmin S, Gando S et al (2013) The role of angiogenic factors and their soluble receptors in acute lung injury (ALI)/ acute respiratory distress syndrome (ARDS) associated with critical illness. Journal of inflammation (London, England) 10:6
Lim HS, Lip GY, Blann AD (2005) Angiopoietin-1 and angiopoietin-2 in diabetes mellitus: relationship to VEGF, glycaemic control, endothelial damage/dysfunction and atherosclerosis. Atherosclerosis 180:113–118
Rasul S, Reiter MH, Ilhan A et al (2011) Circulating angiopoietin-2 and soluble Tie-2 in type 2 diabetes mellitus: a cross-sectional study. Cardiovasc Diabetol 10:55
Chen C, Chen X, Huang H et al (2019) Elevated plasma and vitreous levels of leucine-rich-α2-glycoprotein are associated with diabetic retinopathy progression. Acta Ophthalmol 97:260–264
Pfister F, Wang Y, Schreiter K et al (2010) Retinal overexpression of angiopoietin-2 mimics diabetic retinopathy and enhances vascular damages in hyperglycemia. Acta Diabetol 47:59–64
Li L, Qian L, Yu ZQ (2015) Serum angiopoietin-2 is associated with angiopathy in type 2 diabetes mellitus. J Diabetes Complications 29:568–571
Khalaf N, Helmy H, Labib H et al (2017) Role of angiopoietins and Tie-2 in diabetic retinopathy. Electron Physician 9:5031–5035
You QY, Zhuge FY, Zhu QQ, Si XW (2014) Effects of laser photocoagulation on serum angiopoietin-1, angiopoietin-2, angiopoietin-1/angiopoietin-2 ratio, and soluble angiopoietin receptor Tie-2 levels in type 2 diabetic patients with proliferative diabetic retinopathy. Int J Ophthalmol 7:648–653
Wykoff CC, Abreu F, Adamis AP et al (2022) Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): two randomised, double-masked, phase 3 trials. Lancet (London, England) 399:741–755
Funding
This study was supported by National Natural Science Foundation of China (81870667, 81800835), National Key R&D Program of China (2019YFC0840607), Program of Shanghai Academic/Technology Research Leader (21XD1402700) and Shanghai Talent Development Fund (2020084).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethic approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Medical Ethics Committee of the Shanghai General Hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Fang, J., Niu, T. et al. Serum Ang-1/Ang-2 ratio may be a promising biomarker for evaluating severity of diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 261, 49–55 (2023). https://doi.org/10.1007/s00417-022-05745-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05745-z