Abstract
Purpose
To evaluate the limbal ischemia objectively in ocular surface chemical injuries by using anterior segment optical coherence tomography angiography (AS-OCTA).
Methods
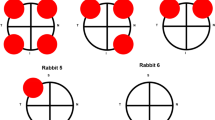
In this cross-sectional study, acute ocular surface chemical injury patients with less than 1 week injury history were enrolled. Demographic data of the patients were noted, and detailed ophthalmological examination with Dua classification was performed. AS photographs and AS-OCTA images were obtained and used for the assessment of limbal ischemia. To visualize the limbal vasculature, the device was focused manually to get a sharp image for all 4 quadrants of the limbus. The absence of vasculature was regarded as “ischemia,” and the amount of the ischemia was defined in clock hours. The limbal ischemia detected in clinical evaluation with biomicroscopy was compared with the AS-OCTA detected ischemia amount to make a conclusion for the correlation.
Results
Nineteen eyes of 18 patients with acute ocular surface chemical injury were enrolled to the study (2 female, 16 male). The mean age was 35.1 ± 10 (18–55), and the mean best corrected visual acuity was 0.75 ± 1 (0.1–3.1) LogMAR. The causative agents were acid in 6 and alkaline in 12 patients. Limbal ischemia detected by using AS-OCTA was greater ((5.8 ± 2.6 (2–10) clock hours) than that detected in biomicroscopy (4.8 ± 2.4 (2–12) clock hours). The difference was statistically significant (p < 0.0005).
Conclusion
AS-OCTA has a significant importance on limbal vascularity visualization; therefore, its use for more objective and sensitive evaluation of limbal ischemia in ocular surface chemical injuries seems to have a crucial impact. AS-OCTA images may reveal the extension of limbal ischemia more precisely than clinical evaluation with biomicroscopy. However, future studies with higher number of patients are needed to come to a specific conclusion.


Similar content being viewed by others
References
Baradaran-Rafii A, Eslani M, Haq Z, Shirzadeh E, Huvard MJ, Djalilian AR (2017) Current and upcoming therapies for ocular surface chemical injuries. Ocul Surf 15:48–64. https://doi.org/10.1016/j.jtos.2016.09.002
Eslani M, Baradaran-Rafii A, Movahedan A, Djalilian AR (2014) The ocular surface chemical burns. J Ophthalmol 2014:196827. https://doi.org/10.1155/2014/196827
Dua HS, King AJ, Joseph A (2001) A new classification of ocular surface burns. J Br J Ophthalmol 85:1379–1383. https://doi.org/10.1136/bjo.85.11.1379
Roper-Hall MJ (1965) Thermal and chemical burns. Trans Ophthalmol Soc U K 85:631–653
Gupta N, Kalaivani M, Tandon R (2011) Comparison of prognostic value of Roper Hall and Dua classification systems in acute ocular burns. Br J Ophthalmol 95:194–198. https://doi.org/10.1136/bjo.2009.173724
Ang M, Sim DA, Keane PA, Sng CC, Egan CA, Tufail A, Wilkins MR (2015) Optical coherence tomography angiography for anterior segment vasculature imaging. Ophthalmology 122:1740–1747
Laíns I, Wang JC, Cui Y, Katz R, Vingopoulos F, Staurenghi G, Vavvas DG, Miller JW, Miller JB (2021) Retinal applications of swept source optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA). Prog Retin Eye Res 84:100951
Grieve K, Ghoubay D, Georgeon C, Thouvenin O, Bouheraoua N, Paques M, Borderie VM (2015) Three-dimensional structure of the mammalian limbal stem cell niche. Exp Eye Res 140:75–84. https://doi.org/10.1016/j.exer.2015.08.003
Akagi T, Uji A, Huang AS, Weinreb RN, Yamada T, Miyata M, Kameda T, Ikeda HO, Tsujikawa A (2018) Conjunctival and intrascleral vasculatures assessed using anterior segment optical coherence tomography angiography in normal eyes. Am J Ophthalmol 196:1–9. https://doi.org/10.1016/j.ajo.2018.08.009
Dua HS, Saini JS, Azuara-Blanco A, Gupta P (2000) Limbal stem cell deficiency: concept, aetiology, clinical presentation, diagnosis and management. Indian J Ophthalmol 48:83–92
Korkmaz I, Palamar M, Egrilmez S, Gurdal M, Yagci A, Barut Selver O (2022) Evaluation of limbal stem cell transplant success in ocular chemical injury. Exp Clin Transplant. https://doi.org/10.6002/ect.2021.0393
Kam KW, Patel CN, Nikpoor N, Yu M, Basu S (2019) Limbal ischemia: reliability of clinical assessment and implications in the management of ocular burns. Indian J Ophthalmol 67:32–36. https://doi.org/10.4103/ijo.IJO_945_18
Easty DL, Bron AJ (1971) Fluorescein angiography of the anterior segment. Its value in corneal disease. Br J Ophthalmol 55:671–682. https://doi.org/10.1136/bjo.55.10.671
Lee WD, Devarajan K, Chua J, Schmetterer L, Mehta JS, Ang M (2019) Optical coherence tomography angiography for the anterior segment. Eye Vis 6:1–9
Kuckelkorn R, Remky A, Wolf S, Reim M, Redbrake C (1997) Video fluorescein angiography of the anterior eye segment in severe eye burns. Acta Ophthalmol Scand 75:675–680. https://doi.org/10.1111/j.1600-0420.1997.tb00629.x
Tey KY, Gan J, Foo V, Tan B, Ke MY, Schmetterer L, Mehta JS, Ang M (2021) Role of anterior segment optical coherence tomography angiography in the assessment of acute chemical ocular injury: a pilot animal model study. Sci Rep 11:16625. https://doi.org/10.1038/s41598-021-96086-0
Fung SSM, Stewart RMK, Dhallu SK, Sim DA, Keane PA, Wilkins MR, Tuft SJ (2019) Anterior segment optical coherence tomographic angiography assessment of acute chemical injury. Am J Ophthalmol 205:165–174. https://doi.org/10.1016/j.ajo.2019.04.021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ege University Committee of Ethics and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere.
Rights and permissions
About this article
Cite this article
Furundaoturan, O., Palamar, M. & Barut Selver, O. Precision of limbal ischemia evaluation in ocular chemical injuries with anterior segment optical coherence tomography angiography. Graefes Arch Clin Exp Ophthalmol 261, 155–159 (2023). https://doi.org/10.1007/s00417-022-05735-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05735-1