Abstract
Purpose
To determine the association between anterior corneal curvature and optical zone centration as well as its impact on aberration profiles in small-incision lenticule extraction (SMILE) and laser in situ keratomileusis (LASIK).
Methods
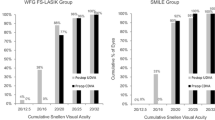
Seventy-eight eyes of 78 patients treated with SMILE (45 eyes) and LASIK (33 eyes) were included. The centration of the optical zone was evaluated on the instantaneous curvature difference map between the preoperative and 3-month postoperative scans using a superimposed set of concentric circles. The correlation between optical zone decentration and anterior keratometry values was evaluated. The effect of optical zone decentration on vector components of astigmatic correction and induction of higher-order aberrations (HOA) was assessed.
Results
The mean decentration distance was 0.21 ± 0.11 mm for SMILE and 0.20 ± 0.09 mm for LASIK (p = 0.808). There was a significant correlation between anterior keratometric astigmatism and decentration distance (r = 0.653, p < 0.001) for SMILE but not for LASIK (r = − 0.264, p = 0.138). Astigmatic correction was performed in 67 eyes. Optical zone decentration and the vector components of astigmatic correction were not correlated (p ≥ 0.420). Significant correlation was demonstrated between the decentration distance and the induced total coma (SMILE: r = 0.384, p = 0.009; LASIK: r = 0.553, p = 0.001) as well as the induced total HOA (SMILE: r = 0.498, p = 0.001; LASIK: r = 0.555, p = 0.001).
Conclusion
Anterior cornea astigmatism affected the treatment centration in SMILE but not LASIK. Subclinical decentration was associated with the induction of total coma and total HOA, but it did not affect the lower-order astigmatic correction.



Similar content being viewed by others
References
Bueeler M, Mrochen M, Seiler T (2003) Maximum permissible lateral decentration in aberration-sensing and wavefront-guided corneal ablation. J Cataract Refract Surg 29:257–263
Mrochen M, Kaemmerer M, Mierdel P, Seiler T (2001) Increased higher-order optical aberrations after laser refractive surgery: a problem of subclinical decentration. J Cataract Refract Surg 27:362–369
Prakash G, Agarwal A, Ashok Kumar D, Jacob S (2011) Comparison of laser in situ keratomileusis for myopic astigmatism without iris registration, with iris registration, and with iris registration-assisted dynamic rotational eye tracking. J Cataract Refract Surg 37:574–581. https://doi.org/10.1016/j.jcrs.2010.11.025
Chan TCY, Ng ALK, Cheng GPM, Woo VCP, Zhang J, Wang Y, Jhanji V (2017) Effect of the learning curve on visual and refractive outcomes of small-incision lenticule extraction. Cornea 36:1044–1050. https://doi.org/10.1097/ICO.0000000000001246
Liu M, Sun Y, Wang D, Zhang T, Zhou Y, Zheng H, Liu Q (2015) Decentration of optical zone center and its impact on visual outcomes following SMILE. Cornea 34:392–397. https://doi.org/10.1097/ICO.0000000000000383
Yu Y, Zhang W, Cheng X, Cai J, Chen H (2017) Impact of treatment decentration on higher-order aberrations after SMILE. J Ophthalmol 2017:9575723. https://doi.org/10.1155/2017/9575723
Li M, Zhao J, Miao H, Shen Y, Sun L, Tian M, Wadium E, Zhou X (2014) Mild decentration measured by a Scheimpflug camera and its impact on visual quality following SMILE in the early learning curve. Invest Ophthalmol Vis Sci 55:3886–3892. https://doi.org/10.1167/iovs.13-13714
Wong JX, Wong EP, Htoon HM, Mehta JS (2017) Intraoperative centration during small incision lenticule extraction (SMILE). Medicine (Baltimore) 96:e6076. https://doi.org/10.1097/MD.0000000000006076
Shah R, Shah S, Sengupta S (2011) Results of small incision lenticule extraction: all-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 37:127–137. https://doi.org/10.1016/j.jcrs.2010.07.033
Reinstein DZ, Gobbe M, Gobbe L, Archer TJ, Carp GI (2015) Optical zone centration accuracy using corneal fixation-based SMILE compared to eye tracker-based femtosecond laser-assisted LASIK for myopia. J Refract Surg 31:586–592. https://doi.org/10.3928/1081597X-20150820-03
Alpins N (2001) Astigmatism analysis by the Alpins method. J Cataract Refract Surg 27:31–49
Güell JL, Verdaguer P, Gris O, Manero F, Elies D (2013) Laser corneal refractive surgery: an update. In: Güell JL (ed) Cataract. ESASO course series, vol 3. Karger, Basel, pp 116–128
Osman IM, Awad R, Shi W, Abou Shousha M (2016) Suction loss during femtosecond laser-assisted small-incision lenticule extraction: incidence and analysis of risk factors. J Cataract Refract Surg 42:246–250. https://doi.org/10.1016/j.jcrs.2015.10.067
Lazaridis A, Droutsas K, Sekundo W (2014) Topographic analysis of the centration of the treatment zone after SMILE for myopia and comparison to FS-LASIK: subjective versus objective alignment. J Refract Surg 30:680–686. https://doi.org/10.3928/1081597x-20140903-04
Zhang J, Wang Y, Chen X (2016) Comparison of moderate- to high-astigmatism corrections using wavefront-guided laser in situ keratomileusis and small-incision lenticule extraction. Cornea 35:523–530. https://doi.org/10.1097/ICO.0000000000000782
Pedersen IB, Ivarsen A, Hjortdal J (2017) Changes in astigmatism, densitometry, and aberrations after SMILE for low to high myopic astigmatism: a 12-month prospective study. J Refract Surg 33:11–17. https://doi.org/10.3928/1081597X-20161006-04
Ganesh S, Brar S, Pawar A (2017) Results of intraoperative manual cyclotorsion compensation for myopic astigmatism in patients undergoing small incision lenticule extraction (SMILE). J Refract Surg 33:506–512. https://doi.org/10.3928/1081597X-20170328-01
Wang L, Koch DD (2008) Residual higher-order aberrations caused by clinically measured cyclotorsional misalignment or decentration during wavefront-guided excimer laser corneal ablation. J Cataract Refract Surg 34:2057–2062. https://doi.org/10.1016/j.jcrs.2008.08.015
Buhren J, Yoon G, Kenner S, MacRae S, Huxlin K (2007) The effect of optical zone decentration on lower- and higher-order aberrations after photorefractive keratectomy in a cat model. Invest Ophthalmol Vis Sci 48:5806–5814. https://doi.org/10.1167/iovs.07-0661
Ivarsen A, Asp S, Hjortdal J (2014) Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology 121:822–828. https://doi.org/10.1016/j.ophtha.2013.11.006
Lieberman DM, Grierson JW (2000) The lids influence on corneal shape. Cornea 19:336–342
Qu J, Lu F, Wu J, Wang Q, Xu C, Zhou X, He JC (2007) Wavefront aberration and its association with intraocular pressure and central corneal thickness in myopic eyes. J Cataract Refract Surg 33:1447–1454. https://doi.org/10.1016/j.jcrs.2007.04.012
Mosquera SA, Verma S, McAlinden C (2015) Centration axis in refractive surgery. Eye Vision 2:4. https://doi.org/10.1186/s40662-015-0014-6
Liu M, Zhang T, Zhou Y, Sun Y, Wang D, Zheng H, Liu Q (2015) Corneal regeneration after femtosecond laser small-incision lenticule extraction: a prospective study. Graefes Arch Clin Exp Ophthalmol 253:1035–1042. https://doi.org/10.1007/s00417-015-2971-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chan, T.C.Y., Wan, K.H., Kang, D.S.Y. et al. Effect of corneal curvature on optical zone decentration and its impact on astigmatism and higher-order aberrations in SMILE and LASIK. Graefes Arch Clin Exp Ophthalmol 257, 233–240 (2019). https://doi.org/10.1007/s00417-018-4165-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4165-8