Abstract
Purpose
To establish whether intraocular pressure (IOP) fluctuations contribute to the risk of developing glaucoma in patients with high-risk ocular hypertension.
Methods
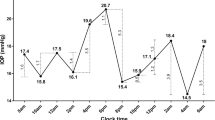
Ninety patients included in the Malmö Ocular Hypertension Study were examined every 3 months with office-hours diurnal tension curves and computerised perimetry. Patients were followed up prospectively for 10 years or until glaucomatous visual field loss could be demonstrated. Poststudy data were included in the analyses, extending maximum follow-up to 17 years.
Results
After 17 years, 37 patients had developed glaucomatous visual field defects. When applying univariate Cox regression analyses, mean IOP of all measurements during the prospective part of the study was a significant risk factor for developing glaucoma (95% confidence interval [CI] 1.08–1.39), while IOP fluctuations were almost significant (95% CI 0.98–1.93). When separating effects of mean IOP level and mean IOP fluctuation using Cox multiple regression analysis, only IOP level came out as significant (95% CI 1.09–1.38), and IOP fluctuations did not contribute to the risk (95% CI 0.80–1.60). IOP fluctuation depended linearly on IOP level (p<0.0001), i.e. IOP fluctuation was larger in eyes with higher IOP levels.
Conclusion
IOP fluctuations were not an independent risk factor for the incidence of glaucomatous visual field loss in subjects with ocular hypertension.

Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
AGIS investigators. The Advanced Glaucoma Intervention Study (AGIS) (2000) The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 130:429–440
Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K (2000) Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma 9:134–142
Bengtsson B, Heijl A (2001) Lack of long-term drift in timolol’s effectiveness in patients with ocular hypertension. Invest Ophthalmol Vis Sci 42:2839–2842
Bergeå B, Bodin L, Svedbergh B (1999) Impact of intraocular pressure regulation on visual fields in open-angle glaucoma. Ophthalmology 106:997–1005
Daugeliene L, Yamamoto T, Kitazawa Y (1999) Risk factors for visual field damage progression in normal-tension glaucoma eyes. Graefes Arch Clin Exp Ophthalmol 237:105–108
De Vivero C, O’Brien C, Lanigan L, Hitching R (1994) Diurnal intraocular pressure variation in low-tension glaucoma. Eye 8:521–523
Drance SM (1960) The significance of the diurnal tension variations in normal and glaucomatous eyes. Arch Ophthalmol 64:494–501
Drance SM (1963) Diurnal variation of intraocular pressure in treated glaucoma. Significance in patients with chronic simple glaucoma. Arch Ophthalmol 70:302–311
Duke Elder S (1952) The phasic variations in the ocular tension in primary glaucoma. Am J Ophthalmol 35:2–8
Gonzalez I, Pablo IE, Pueyo M, Ferrer B, Melcon E, Abecia E, Honrubia FM (1997) Assessment of diurnal tension curve in early glaucoma damage. Int Ophthalmol 20:113–115
Heijl A, Bengtsson B (2000) Long-term effects of timolol therapy in ocular hypertension a double-masked, randomised trial. Graefes Arch Clin Exp Ophthalmol 238:877–883
Heijl A, Drance SM (1981) A clinical comparison of three computerized automatic perimeters in the detection of glaucoma defects. Arch Ophthalmol 99:832–836
Heijl A, Drance SM, Douglas GR (1980) Automatic perimetry (Competer). Ability to detect early glaucomatous field defects. Arch Ophthalmol 98:1560–1563
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M (2002) Reduction of intraocular pressure and glaucoma progression. Results from the early manifest glaucoma trial. Arch Ophthalmol 120:1268–1279
Heijl A, Lindgren G, Olsson J (1986) A package for the statistical analysis of visual fields. Doc Ophthalmol Ser 49:153–168
Ishida K, Yamamoto T, Kitazawa Y (1998) Clinical factors associated with progression of normal-tension glaucoma. J Glaucoma 7:372–377
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK, Wilson MR, Gordon MO (2002) The ocular hypertension treatment study: a randomised trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 120:701–713
Katavisto M (1964) The diurnal variations of ocular tension in glaucoma. Acta Ophthalmol 46 [Suppl 78]:1–130
Langley D, Swanljung H (1951) Ocular tension in glaucoma simplex. Br J Ophthalmol 35:445–458
Liu JHK, Zhang X, Kripke DF, Weinreb RN (2003) twenty-four-hour intra ocular pressure pattern associated with early glaucomatous changes. Invest Ophthalmol Vis Sci 44:1586–1590
Maslenikow AZ (1904) Ueber Tagesschwankungen des intraokularen Druckes bei Glaukom. Augenheilk 11:564
Mills RP, Hopp RH, Drance SM (1986) Comparison of quantitative testing with the Octopus, Humphrey, and Tubingen perimeters. Am J Ophthalmol 102:496–504
Nouri-Mahdavi K, Hoffman D, Coleman AL, Liu G, Li G, Gaasterland D, Caprioli J (2004) Predictive factors for glaucomatous visual field progression in the Advanced Glaucoma Intervention Study. Ophthalmology 111:1627–1635
Saccà SC, Rolando M, Marletta A, Cerqueti P, Ciurlo G (1998) Fluctuations of intraocular pressure during day in open-angle glaucoma, normal-tension glaucoma and normal subjects. Ophthalmologica 212:115–119
Smith J (1985) Diurnal intraocular pressure. Correlation to automated perimetry. Ophthalmology 92:858–861
Wax MB, Camras CB, Fiscella RG, Girkin C, Singh K, Weinreb R (2002) Emerging perspectives in glaucoma: optimizing 24-hour control of intraocular pressure. Am J Ophthalmol 133 [Suppl]:S1–S10
Acknowledgements
This study was supported by grant K2002-74X-10426-10A from the Swedish Research Council, by the Järnhardt Foundation and by funds administered by Malmö University Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bengtsson, B., Heijl, A. Diurnal IOP fluctuation: not an independent risk factor for glaucomatous visual field loss in high-risk ocular hypertension. Graefe's Arch Clin Exp Ophthalmol 243, 513–518 (2005). https://doi.org/10.1007/s00417-004-1103-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-004-1103-8