Abstract
Background
The pathogenesis of PD has not been fully elucidated, but recent studies have shown that the adaptive immune system may play a role in the pathology of PD. However, there is a lack of longitudinal studies exploring the relationship between peripheral adaptive immune indicators and the rate of disease progression in PD.
Methods
We included early PD patients with disease duration < 3 years and assessed the severity of clinical symptoms and peripheral adaptive immune system indicators (CD3+, CD4+, CD8+ T lymphocyte subsets, CD4+:CD8+ ratio, IgG, IgM, IgA, C3, C4) at baseline. Clinical symptoms were followed up every year. We used the Unified Parkinson's Disease Rating Scale (UPDRS) to assess the disease severity and the Montreal Cognitive Assessment (MoCA) to assess global cognitive function.
Result
A total of 152 PD patients were eventually included. The linear mixed model showed no significant association between baseline peripheral blood adaptive immune indicators and baseline MoCA scores or UPDRS part III scores. A higher baseline CD3+ lymphocyte percentage was associated with a slower rate of decline in MoCA scores. Baseline immune indicators were not associated with the rate of change of the UPDRS part III scores.
Conclusion
The subset of peripheral T lymphocytes was related to the rate of cognitive decline in early PD patients, suggesting that the peripheral adaptive immune system may be involved in the process of cognitive decline in early PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson's disease (PD) is a neurodegenerative disease with motor and non-motor symptoms. The anti-Parkinson's drugs can relieve the motor symptom of PD patients, but cannot delay the progression of the disease [1]. As the disease progresses, both motor and non-motor symptoms are gradually aggravated and become more complicated, adding extremely heavy disease burdens on patients. However, there is great heterogeneity in the rate of disease progression among different PD patients. Therefore, it is important to search for related factors affecting the progression of PD disease and explore the potentiality of slowing the progression of PD disease.
Abundant evidence showed that immunity is closely related to neurodegenerative diseases [2]. Abnormal activation of the adaptive immune system is involved in the pathogenesis of PD. [3] Infiltration of CD4 + , CD8 + T lymphocytes, and IgG combined with neurons were found in the substantia nigra of PD patients [4]. Moreover, the density of CD8 + T lymphocytes infiltrated in the substantia nigra of PD patients was proportional to the degree of neuron loss [5,6,7]. Immunohistochemical staining also found that both Lewy bodies and oligodendroglia cells in the substantia nigra of PD patients could be labeled with anti-human complement protein antibodies, suggesting that the activation of the complement system is also involved in PD [8,9,10,11]. Meta-analysis showed that the CD3 + and CD4 + T lymphocyte subsets in the peripheral blood of PD patients decreased compared with normal controls [12]. The level of CD8 + T lymphocytes showed no significant difference in the early stage of the disease but decreased significantly in the late stage of the disease [12]. The CD4 + :CD8 + lymphocytes ratio in the peripheral blood of PD patients was also lower than that of normal controls [13, 14].
Previous cross-sectional studies found that peripheral immune indicators were related to the severity of PD symptoms, but reached inconsistent results [13, 15]. Hu et al. found that PD patients with advanced disease had higher CD4 + , CD8 + T lymphocyte subset, and CD4 + :CD8 + ratio than PD patients in the early stage [13]. The extent to which the CD3 + CD8 + T subset deviates from the reference range was positively correlated to the scores of the Movement Disorders Society-Unified Parkinson's Disease Rating Scale (MDS-UPDRS) part III [15]. A study found that the CD4 + , CD8 + T lymphocyte subset, and the CD4 + :CD8 + ratio of PD patients with dementia were lower than those without dementia [13]. Another study with a larger sample size found that PD patients with cognitive impairment had higher levels of peripheral blood lymphocytes than PD patients without cognitive impairment [16]. Previous studies also found that peripheral blood IgG levels were positively correlated with disease duration and the scores of the Unified Parkinson's Disease Rating Scale (UPDRS) part III [17]. PD patients who complained of attention and cognitive problems had lower levels of IgA in peripheral blood than those without complaints [11]. In addition, one study found that patients with cognitive complaints had lower levels of peripheral blood C3 [11], while another study found that lower cognitive test scores were associated with higher levels of peripheral blood C4 [10].
Several simple adaptive immune system markers have been reported to be involved in the pathology of PD by some previous studies, which can represent the peripheral adaptive immune status [4,5,6,7,8,9,10,11]. Recent literature also found that there were differences between PD and healthy controls in these immune markers [12, 17]. However, in the early stage of PD, whether the current peripheral markers can reflect the status of the adaptive immune system and whether these immune makers were probably associated with the progression of PD remains largely unknown. Therefore, we performed the current study to clarify whether these peripheral markers can predict the progression of early-stage PD.
Methods
Subjects
Subjects of this study were PD patients admitted to the outpatient department and inpatient department of the Neurology Department, West China Hospital of Sichuan University from August 2013 to April 2021. This study was approved by the Ethics Committee of West China Hospital of Sichuan University, and all subjects signed informed consent for the clinical study. Inclusion criteria were listed as follows: (1) diagnosed as PD according to the British Brain Bank Standard 19 or the 2015 version of Movement Disorder Society Clinical Diagnostic Criteria [18, 19]; (2) disease duration at baseline less than 3 years; (3) Hoehn and Yahr stage at baseline less than 3. Exclusion criteria were: (1) having severe postural hypotension, urinary incontinence, ataxia, gaze paralysis, severe cognitive impairment, postural instability, and other symptoms suggesting Parkinson's syndrome at baseline; (2) auxiliary examination (head MRI, bladder residual urine color ultrasound) at baseline indicating the patient was not Parkinson's disease; (3) diseases that can influence the peripheral immune indicators such as infectious diseases and autoimmune diseases at baseline; (4) under anti-inflammatory or other immunomodulatory therapies.
Clinical assessment
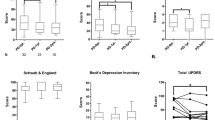
Subjects were followed up at baseline and annually for face-to-face assessment by a trained neurology clinician. The assessment included demographic characteristics, medical history, physical examination, and symptom scales. UPDRS and Hoehn & Yahr scales were used to assess the severity of the disease. The Montreal Cognitive Assessment (MoCA) was used to assess global cognition [20]. Anxiety and depression were determined by Hamilton Depression Rating Scale (HAMD, 24 items 22) and Hamilton Anxiety Rating Scale (Hamilton Anxiety Rating Scale, 24 Items 22) (HAMA 23) [21, 22]. Rapid Eye Movement Sleep Behavior Disorder (RBD) was defined as the Rapid Eye Movement Sleep Behavior Disorder Screening Questionnaire (RBDSQ) score equal to or greater than 5 [23]. Levodopa equivalent dose (LEDD) was calculated according to previous guidelines [24]. According to the previous literature, the ratio of the average score of the tremor subitem to the average score of the postural instability and gait difficulty subitem was calculated, and the patients were divided into three different movement subtypes: tremor-dominant (TD), indeterminate, and postural instability and gait difficulty (PIGD). A ratio ≤ 1 was defined as PIGD type, a ratio between 1 and 1.5 was defined as indeterminate, and a ratio over 1.5 or the PIGD score equal to 0 was defined as TD [25].
Laboratory examination
Percentages of the CD3 + subset, CD4 + subset, CD8 + subset, CD4 + :CD8 + ratio, and the level of C3, C4, IgG, IgA, and IgM in the serum were measured within 1 month before or after the baseline visit. Peripheral blood samples (∼ 9 ml each set) were obtained from each patient by venipuncture between 8:00 and 11: 00 am after fasting from midnight. Blood samples were collected into a sterile 7.5 ml tube with a clot activator and double gel (BD Vacutainer, SST, REF 367987) and then transported to the laboratory. The lymphocyte subsets were evaluated using the BD FACSCanto II Flow Cytometer [Becton Dickinson (BD) Biosciences, Heidelberg, Germany]. The percentage of the cells expressing CD3 + , CD4 + , and CD8 + markers was measured and the CD4 + :CD8 + ratio was calculated by dividing the percentage of CD4 + cells by the percentage of CD8 + cells. Levels of IgG, IgM, IgA, C3, and C4 were quantified using Luminex rate nephelometry (Beckman Coulter, Fullerton, CA, United States). All the experiments were conducted by board-certified laboratory technicians who were blind to the clinical data in the Biochemistry Laboratory of West China Hospital of Sichuan University.
Statistical analysis
We use the Kolmogorov−Smirnov test to test the normal state of continuous variables. The continuous variables of this study were not a normal distribution, so the continuous variables were shown in the median (four-point range), and the classification variables were shown in percentages. Using the Spearman correlation analysis to explore the relationship between baseline clinical features and peripheral immune indicators, and using the Kruskal−Wallis test to compare the peripheral immune indicators between patients with different baseline characteristics. We use the linear mixed-effect regression model to analyze the relationship between baseline blood indicators and the rate of change in motor and cognitive functions. Given the severity of the baseline symptoms and the speed of the symptoms are different among patients, we set a random intercept and random slope in the model. Because of the significant differences in the ranges of blood indicators, we standardized all indicators. The baseline peripheral immune indicators were incorporated as independent variables, and the UPDRS part III scores and the MoCA scores were incorporated as the dependent variables. The peripheral immune indicator variable was used as the main effect to evaluate the correlation of baseline blood indicators and baseline movement symptoms and cognitive levels. The interactions between peripheral immune indicators and time (in annual units) were used to evaluate the relationship between baseline blood indicators and the rate of change in symptoms. In the model with the UPRDS part III score being the dependent variable, we set the age, interaction of age and time, sex, disease duration, and baseline LEDD as covariable. In the model of MoCA score as the dependent variable, we set up age, sex, baseline UPRDS part III score, baseline LEDD, education, baseline use of Anticholinergic drug, and their interaction with time as the covariable. In further sensitivity analysis, we added the baseline RBD (yes or no), baseline HAMA scores, and baseline HAMD scores as covariables in the model to correct the impact of RBD and mood disorders on cognition. P < 0.05 was considered to be statistically significant, and all data analysis was completed using SPSS 22.0 and R 4.1.2.
Result
A total of 152 PD patients were included in the study and the baseline characteristics of the patient were shown in Table 1. The mean follow-up duration of the cohort was 30.75 months, with a total of 389.53 person-years of follow-up. The correlation between the baseline characteristics of the patients and the peripheral immune inflammation index was shown in Table 2. IgA (\(\rho\) = 0.218) and CD3 + T lymphocyte subset (\(\rho\) = 0.183) was negatively related to age. There is no significant correlation between the level of peripheral blood immune inflammation and the HAMA, HAMD, and RBDSQ scores. We found that female patients had a higher percentage of the CD3 + T lymphocyte subset and C3 level than male patients. (Stable 1) A total of 74 patients were classified as TD and 22 patients were classified as indeterminate, and 56 patients were classified as PIGD. There was no significant difference in the level of peripheral blood immune indicators in patients with different subtypes. (STable 2) As levodopa may influence the adaptive immune status, we also compared the immune characteristics of patients with or without levodopa treatment in Stable 3 and found that there were no differences between the two groups [26].
Table 3 shows the relationship between immune indicators and the disease severity at baseline. There was no association between the immune indicators and disease severity. Table 4 shows the relationship between peripheral immune indicators and the progression of disease severity. Patients with a higher baseline CD3 + T lymphocyte subset had a slower rate of decrease in MoCA scores (β = 0.220, P = 0.015). After adjusting the RBD, HAMA score, and HAMD score, a higher baseline CD3 + T lymphocyte subset still predicted a slower rate of cognitive deterioration (β = 0.224, P = 0.013). Other peripheral blood immune indicators were unrelated to the change in MoCA scores. The baseline peripheral blood immunoinflammatory levels were not related to the rate of change in the UPDRS part III scores.
Discussion
In this study, we found that PD patients with a higher baseline proportion of the CD3 + T lymphocyte subset had a slower rate of cognitive decline in the follow-up. The proportion of CD3 + , CD4 + , CD8 + T lymphocyte subset, and the CD4 + :CD8 + ratio was not correlated with the severity of the disease (cognitive symptoms, motor symptoms, RBD symptoms, anxiety symptoms, and depression symptoms) in early-stage PD patients. We found that female patients had a higher CD3 + T subset than male patients, and there was no significant difference in CD4 + , CD8 + T subset proportion, and CD4 + :CD8 + ratios between the females and males. We also found that the proportion of the CD3 + T lymphocyte subset (rho = -0.183) was negatively correlated with age, while CD4 + , CD8 + T lymphocyte subset, and CD4 + :CD8 + ratio were not significantly correlated with age.
Deviation from the reference range of the CD3 + CD8 + T subset was positively correlated to the MDS-UPDRS part III scores [15]. However, the disease duration of the population in the previous study was much longer than that in the current study, which may contribute to such different results. [15, 17] Previous meta-analyses found that there was no significant difference in peripheral blood CD8 + T subset between early-stage PD patients (Hoehn and Yahr stage 1−3) and normal controls. But late-stage PD patients (Hoehn and Yahr stage 4−5) had a significantly lower proportion of peripheral blood CD8 + T subset than normal controls, suggesting that the immune system dysfunction was significant with the progression of the disease [12]. Additionally, a previous study reported that female PD and normal control subjects had a higher level of CD3 + T lymphocyte subset than male PD and normal control subjects [17].
We found that CD3 + T lymphocyte subset proportion was not associated with baseline cognitive scores in patients but was associated with a faster rate of cognitive decline. This result was not driven by the use of levodopa since there were no differences in peripheral immune markers between patients with or without levodopa treatment. Previous studies also found that the peripheral lymphocyte count had a close association with cognition in PD patients. [27] In PD patients who carried ApoE ε4 allele, those with a lower peripheral blood lymphocyte count had a more rapid rate of decline in MoCA scores than that those with a higher count [27]. Our findings further highlight the association between the T lymphocyte count and cognitive decline in PD.
A longitudinal case study showed that the highest alpha-synuclein-specific T cell reactivity was detected prior to the onset of PD and the level of reactivity decreased after onset [26]. In addition, the infiltration of CD8 + T lymphocytes in the substantia nigra was detected prior to the dopaminergic neuron loss and the Lewy neurites appearance in patients with incidental Lewy disease [6]. The above-mentioned evidence raised an assumption that the adaptive immune system was activated in the prodromal stage of PD and decreased during the clinical stage [28]. The activity of disease-related adaptive immune status may become milder with the aggravation of the pathology in the clinical stage of PD [29]. And in the early stage of the pathology, the adaptive immune system was still active and the involvement of the cerebral cortex was absent or mild [29]. Although CD3 + T cell is not a specific representation of the alpha-Synuclein-specific adaptive immune, the association between a higher CD3 + T subset and a decreasing rate of cognition observed in the current study was consistent with the assumption. However, the selected immune markers in the current study were relatively simple. It is necessary to study the new and more complex immune markers such as alpha-synuclein-specific T cells and related cytokines in PD in future research.
CD3 + T subset reflects the proportion of T lymphocytes in total lymphocytes, while CD4 + and CD8 + T lymphocytes reflect the proportion of T helper (Th) cells and cytotoxic T lymphocytes in peripheral blood. Different subtypes of T lymphocytes produce various cytokines which promote the adaptive immune process and peripheral inflammation. Compared with normal controls, PD patients had lower proportions of the initial CD4 + T lymphocytes and initial CD8 + T lymphocytes, and higher proportions of central memory CD4 + T lymphocytes, Th2 cells that produce the anti-inflammatory cytokine IL-4, and Th17 cells that produce the pro-inflammatory cytokine IL-17A [30]. Around 0.2% of CD3 + T cells responded to the alpha-synuclein peptides and more than half of the responsive T cells produced IL-4 or produced IFNγ [31]. While those with anti-inflammatory overall cytokines status had a slower rate of cognitive decline compared to those with pro-inflammatory overall cytokines status in PD, T lymphocytes may influence the rate of cognitive symptom progression in PD patients through cytokines. [32]
There are some limitations of the current study. First, only MoCA was used to evaluate the overall cognitive status of patients. The multi-domain cognitive tests can be used to explore the correlation between peripheral adaptive immunity and changes in specific cognitive fields of PD patients. Second, the cognitive status of PD patients is influenced by their gene status. Although we adjusted the clinical characteristics as much as possible, further studies are needed to explore the association of immune and cognition in PD patients carrying different gene variations. Third, the vaccine history of the patients was not clear. The COVID-19 vaccine was popular under the background of the COVID-19 pandemic. We did a sensitivity analysis after excluding those enrolled after the appearance of the COVID-19 vaccine and reached a similar result (CD3 + T cell subset*TIME in the cognitive model: β = 0.222, SE = 0.090, P = 0.016).
There are some strengths of the current study. We only included patients with early-stage PD patients to avoid the reverse influence that the immune system changes along with the PD disease processing. In addition, this is a longitudinal cohort study so the association of the baseline immune study and the following changes in disease severity can be evaluated.
Conclusion
Our results suggest that peripheral blood immune indicators (CD3 + , CD4 + , CD8 + T lymphocyte subset, CD4 + :CD8 + ratio, IgG, IgA, IgM, C3, C4) were not related to disease severity (cognitive and motor symptoms). However, the higher proportion of CD3 + T lymphocyte subset at baseline was associated with a slower rate of cognitive decline in patients, suggesting that the immune system plays an important role in cognitive decline in early PD patients.
Availability of data and materials
The data used in the current study are available from the corresponding author upon reasonable request.
References
Grimes D, Fitzpatrick M, Gordon J, Miyasaki J, Fon EA, Schlossmacher M, Suchowersky O, Rajput A, Lafontaine AL, Mestre T, Appel-Cresswell S, Kalia SK, Schoffer K, Zurowski M, Postuma RB, Udow S, Fox S, Barbeau P, Hutton B (2019) Canadian guideline for Parkinson disease. CMAJ 191:E989–E1004
Li CY, Yang TM, Ou RW, Wei QQ, Shang HF (2021) Genome-wide genetic links between amyotrophic lateral sclerosis and autoimmune diseases. BMC Med 19:27
Kustrimovic N, Marino F, Cosentino M (2019) Peripheral immunity, immunoaging and neuroinflammation in Parkinson’s disease. Curr Med Chem 26:3719–3753
Orr CF, Rowe DB, Mizuno Y, Mori H, Halliday GM (2005) A possible role for humoral immunity in the pathogenesis of Parkinson’s disease. Brain J Neurol 128:2665–2674
Brochard V, Combadiere B, Prigent A, Laouar Y, Perrin A, Beray-Berthat V, Bonduelle O, Alvarez-Fischer D, Callebert J, Launay JM, Duyckaerts C, Flavell RA, Hirsch EC, Hunot S (2009) Infiltration of CD4+ lymphocytes into the brain contributes to neurodegeneration in a mouse model of Parkinson disease. J Clin Invest 119:182–192
Galiano-Landeira J, Torra A, Vila M, Bové J (2020) CD8 T cell nigral infiltration precedes synucleinopathy in early stages of Parkinson’s disease. Brain J Neurol 143:3717–3733
Kouli A, Camacho M, Allinson K, Williams-Gray CH (2020) Neuroinflammation and protein pathology in Parkinson’s disease dementia. Acta Neuropathol Commun 8:211
Yamada T, Akiyama H, McGeer PL (1990) Complement-activated oligodendroglia: a new pathogenic entity identified by immunostaining with antibodies to human complement proteins C3d and C4d. Neurosci Lett 112:161–166
Yamada T, McGeer PL, McGeer EG (1992) Lewy bodies in Parkinson’s disease are recognized by antibodies to complement proteins. Acta Neuropathol 84:100–104
Veselý B, Dufek M, Thon V, Brozman M, Királová S, Halászová T, Koriťáková E, Rektor I (2018) Interleukin 6 and complement serum level study in Parkinson’s disease. J Neural Transm (Vienna, Austria: 1996) 125:875–881
Sun C, Yu W, Zhao Z, Song C, Liu Y, Jia G, Wang X, Liu Y (2019) Peripheral humoral immune response is associated with the non-motor symptoms of Parkinson’s disease. Front Neurosci 13:1057
Jiang S, Gao H, Luo Q, Wang P, Yang X (2017) The correlation of lymphocyte subsets, natural killer cell, and Parkinson’s disease: a meta-analysis. Neurol Sci 38:1373–1380
Hu ZX, Song WN, Lu XD, Zhou ML, Shao JH (2018) Peripheral T lymphocyte immunity and l-dopamine in patients with Parkinson’s disease. J Biol Regul Homeost Agents 32:687–691
Baba Y, Kuroiwa A, Uitti RJ, Wszolek ZK, Yamada T (2005) Alterations of T-lymphocyte populations in Parkinson disease. Parkinsonism Relat Disord 11:493–498
Sun C, Zhao Z, Yu W, Mo M, Song C, Si Y, Liu Y (2019) Abnormal subpopulations of peripheral blood lymphocytes are involved in Parkinson’s disease. Ann Transl Med 7:637
Magistrelli L, Storelli E, Rasini E, Contaldi E, Comi C, Cosentino M, Marino F (2020) Relationship between circulating CD4+ T lymphocytes and cognitive impairment in patients with Parkinson’s disease. Brain Behav Immun 89:668–674
Chen X, Feng W, Ou R, Liu J, Yang J, Fu J, Cao B, Chen Y, Wei Q, Shang H (2021) Evidence for peripheral immune activation in Parkinson’s disease. Front Aging Neurosci 13:617370
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1601
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6:278–296
Clark DB, Donovan JE (1994) Reliability and validity of the Hamilton Anxiety Rating Scale in an adolescent sample. J Am Acad Child Adolesc Psychiatry 33:354–360
Stiasny-Kolster K, Mayer G, Schafer S, Moller JC, Heinzel-Gutenbrunner M, Oertel WH (2007) The REM sleep behavior disorder screening questionnaire–a new diagnostic instrument. Mov Disord 22:2386–2393
Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653
Jankovic J, McDermott M, Carter J, Gauthier S, Goetz C, Golbe L, Huber S, Koller W, Olanow C, Shoulson I et al (1990) Variable expression of Parkinson’s disease: a base-line analysis of the DATATOP cohort. The Parkinson Study Group. Neurology 40:1529–1534
Lindestam Arlehamn CS, Dhanwani R, Pham J, Kuan R, Frazier A, Rezende Dutra J, Phillips E, Mallal S, Roederer M, Marder KS, Amara AW, Standaert DG, Goldman JG, Litvan I, Peters B, Sulzer D, Sette A (2020) alpha-Synuclein-specific T cell reactivity is associated with preclinical and early Parkinson’s disease. Nat Commun 11:1875
Tsukita K, Sakamaki-Tsukita H, Takahashi R (2021) Lower circulating lymphocyte count predicts ApoE ε4-related cognitive decline in Parkinson’s disease. Mov Disord 36:2969–2971
Singhania A, Pham J, Dhanwani R, Frazier A, Rezende Dutra J, Marder KS, Phillips E, Mallal S, Amara AW, Standaert DG, Sulzer D, Peters B, Sette A, Lindestam Arlehamn CS (2021) The TCR repertoire of α-synuclein-specific T cells in Parkinson’s disease is surprisingly diverse. Sci Rep 11:302
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K (2004) Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res 318:121–134
Yan Z, Yang W, Wei H, Dean MN, Standaert DG, Cutter GR, Benveniste EN, Qin H (2021) Dysregulation of the adaptive immune system in patients with early-stage Parkinson disease. Neurology(R) Neuroimmunol NEUROINFLAMM 8:e1036
Sulzer D, Alcalay RN, Garretti F, Cote L, Kanter E, Agin-Liebes J, Liong C, McMurtrey C, Hildebrand WH, Mao X, Dawson VL, Dawson TM, Oseroff C, Pham J, Sidney J, Dillon MB, Carpenter C, Weiskopf D, Phillips E, Mallal S, Peters B, Frazier A, Lindestam Arlehamn CS, Sette A (2017) T cells from patients with Parkinson’s disease recognize α-synuclein peptides. Nature 546:656–661
Williams-Gray CH, Wijeyekoon R, Yarnall AJ, Lawson RA, Breen DP, Evans JR, Cummins GA, Duncan GW, Khoo TK, Burn DJ, Barker RA, group I-Ps (2016) Serum immune markers and disease progression in an incident Parkinson’s disease cohort (ICICLE-PD). Mov Disord 31:995–1003
Funding
This work was funded by the National Key Research and Development Plan (Grant No. 2021YFC2501203), the Sichuan Science and Technology Program (Grant No. 2022ZDZX0023), and the Sichuan Province Cadre Health Research Project (2022–115).
Author information
Authors and Affiliations
Contributions
YX: organization and execution of research project, design, and execution of statistical analysis, writing of the draft, review, and critique of the manuscript; QW: organization and execution of research project, design of the statistical analysis; RO: review, and critique of the manuscript; TY, QJ, YH, LZ, KL, SW, JL, BZ, WS, XC, YW, and CL: organization and execution of research project; HS: conception, organization, and execution of research project, review, and critique of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests. There were no financial conflicts of interest to disclose.
Ethics approval
This study was approved by the Institutional Ethics Committee of West China Hospital.
Consent to participate
Informed consent was obtained from all the participants of the study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, Y., Wei, Q., Ou, R. et al. Association between peripheral adaptive immune markers and disease progression in Parkinson's disease. J Neurol 270, 4444–4450 (2023). https://doi.org/10.1007/s00415-023-11790-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11790-3