Abstract
Background
Spinal muscular atrophy (SMA) is an autosomal recessive disease where a deficient amount of SMN protein leads to progressive lower motor neuron degeneration. SMN-enhancing therapies are now available. Yet, fatigue and signs of impaired neuromuscular junction (NMJ) transmission could contribute to SMA phenotype. Amifampridine prolongs presynaptic NMJ terminal depolarization, enhancing neuromuscular transmission.
Methods
SMA-001 was a phase 2, 1:1 randomized, double-blind, placebo-controlled crossover study. Ambulatory (walking unaided at least 30 m) SMA Type 3 patients, untreated with SMN-enhancing medications, entered a run-in phase where amifampridine was titrated up to an optimized stable dose. Patients achieving at least three points improvement in Hammersmith Functional Motor Score Expanded (HFMSE) were randomized to amifampridine or placebo, alternatively, in the 28-day double-blind crossover phase. Safety was evaluated by adverse events (AE) collection. Primary efficacy measure was the HFMSE change from randomization. Secondary outcomes included timed tests and quality of life assessment. Descriptive analyses and a mixed effects linear model were used for statistics.
Results
From 14 January 2019, 13 patients, mean age 34.5 years (range 18–53), with 5/13 (38.5%) females, were included. No serious AE were reported. Transient paresthesia (33.3%) was the only amifampridine-related AE. Six patients for each treatment sequence were randomized. Amifampridine treatment led to a statistically significant improvement in HFMSE (mean difference 0.792; 95% CI from 0.22 to 1.37; p = 0.0083), compared to placebo, but not in secondary outcomes.
Discussion
SMA-001 study provided Class II evidence that amifampridine was safe and effective in treating ambulatory SMA type 3 patients. Clinical Trial Registration: NCT03781479; EUDRACT 2017-004,600-22.
Similar content being viewed by others
Introduction
Spinal muscular atrophy (SMA) is an autosomal recessive neuromuscular disease caused by homozygous deletions or mutations in the survival motor neuron 1 (SMN1) gene, located on 5q chromosome, encoding the SMN protein. Hallmarks of the disease are progressive degeneration of spinal cord and bulbar motor neurons with consequent weakness and atrophy of skeletal muscles, leading to respiratory deficiency and nutritional impairment in most severe forms [1]. SMA has an overall incidence of 1:6000–1:10,000 live births and is a major genetic cause of death in children [2, 3]. Five phenotypical types of SMA (0 to 4) are described on the basis of age at onset, ranging from in utero to adulthood, and maximum motor milestone achieved [3, 4]. Clinical severity is highly variable, even within the same type, mainly depending on the copies of a paralogous gene (SMN2), which partially compensates for SMN protein deficiency [5, 6]. For this reason, increasing SMN protein production by SMN2 is the target of two out of the three recently approved therapies for the treatment of SMA, the third being directed at reintroducing SMN1 gene [7,8,9]. SMN-enhancing treatments (i.e., nusinersen, risdiplam, or onasemnogene abeparvovec) have demonstrated to extend life expectancy and promote gaining of motor milestones. However, they do not fully recover the phenotypes, and other potentially complementary therapeutic strategies are under investigation [10, 11].
It has long been known that SMA is associated with an impairment of neuromuscular junction (NMJ) development and transmission, which contributes to muscle disturbance [12,13,14,15]. SMA Type 2 and 3 patients commonly report fatigue as a relevant symptom and display a significant decremental response at the repetitive nerve stimulation study, which supports the pathogenic role of NMJ dysfunction [12, 16, 17]. Thus, enhancing NMJ transmission might be a pivotal combinatorial approach for the treatment of SMA.
Amifampridine (3,4-diaminopyridine phosphate) is a voltage-dependent K + channel blocker that prolongs depolarization of the presynaptic neuromuscular junction terminal and increases acetylcholine release, empowering neuromuscular transmission and muscle function [18, 19]. Amifampridine is recommended for the symptomatic treatment of Lambert–Eaton myasthenic syndrome by the European Federation of Neurological Societies and the Food and Drug Administration in the USAs, and its efficacy has been proven in different autoimmune and genetic NMJ diseases, including anti-MuSK myasthenia gravis (MG) and congenital myasthenic syndrome (CMS) [20,21,22,23]. Amifampridine is rapidly absorbed after oral administration and rapidly eliminated, with the phosphate form having a short half-life of about 1.8 h [24, 25].
Based on this evidence, in the SMA-001 trial, we aimed to evaluate whether fostering neuromuscular transmission could improve fatigability and motor function in SMA patients; hence, we assessed the safety and efficacy of amifampridine in ambulatory patients with SMA Type 3, not receiving other disease-modifying therapies.
Methods
Study design
We conducted a randomized, double-blinded, placebo-controlled, crossover, phase 2a trial to assess the safety and efficacy of amifampridine phosphate (Firdapse®, Catalyst Pharmaceuticals, Inc., Coral Gables, FL, USA) in patients with SMA type 3 not receiving nusinersen. he study was conducted in Europe in two centers (Neurological Institute Carlo Besta IRCCS Foundation, Milan, Italy and Neurology Clinic, Faculty of Medicine, University of Belgrade, Belgrade, Serbia). After a screening period of maximum 14 days, all patients entered an open-label run-in period where orally self-administered amifampridine was titrated upward every 3–4r days, up to 80 mg/day [26], until reaching the maximal tolerable and effective dose. Patients had phone/video contacts with the investigator for each titration and at least one in-person site visit at Week 3. Run-in period could be extended if additional time was needed for dose titration. The effective dose was identified when patients achieved an improvement of at least three points in the Hammersmith Functional Motor Scale Expanded (HFMSE), assessed by a trained therapist [27, 28]. Afterward, if the patients demonstrated they could remain at a stable amifampridine dose and frequency for at least an additional 7 days, confirming at the end of this period the clinically significant HFMSE improvement compared to the start of the run-in period, they could enter the randomized, double-blinded crossover phase. andomization schedule was generated by the study randomization biostatistician and kept secret until study unblinding. Prepackaged medication kits were prepared by the central pharmacist according to randomization schedule and sent to centers. At the moment of randomization, investigators had to select the next available randomization number, linking the subject to the allocated treatment sequence, take the kit assigned to that subject, and dispense it. Investigators and participants were unaware of the allocated treatment sequence until the end of study. No stratification factors were applied. The total study duration was approximately 60 days for each patient, depending on the duration of the run-in period, and excluding the screening period. Patients who successfully completed the run-in and maintained inclusion criteria were randomly assigned 1:1 to the amifampridine/placebo (AP) or the placebo/amifampridine (PA) sequence and received amifampridine or placebo for 2 weeks, respectively (Period 1). Then, patients received amifampridine or placebo, whichever treatment they did not receive in Period 1, for other 2 weeks up to the end of the study (Period 2). From randomization day (day 0, Baseline) to the end of study (day 28), patients underwent in-person clinical visits every 7 days. Treatment periods were not separated by washout periods. This decision was made since, by the end of the first day of each treatment period, more than six elimination half-lives of each treatment would have passed, allowing the systemic elimination of the drug. The study was designed by the study authors (LM and GI) in collaboration with the sponsor. The study was sponsored by Catalyst Pharmaceuticals, Inc. and an independent Clinical Research Organization supervised and provided assistance to the trial conduit. Statistical analyses were performed by SPARC Consulting, Milan, Italy, on behalf of the sponsor. All the authors had access to the study data, gave critical revision of the manuscript, and approved the submission. The authors and Catalyst Pharmaceutical, Inc. vouch for the adherence to the trial protocol and data analysis. The CONSORT statement was followed for the realization of this paper [29]. The study protocol and statistical analysis plan are available in Online Resource 1 and Online Resource 2, respectively.
Patients
Key inclusion criteria for patients were age from 6 to 50 years; genetically confirmed SMA and clinically defined Type 3 form of the disease; ability to walk independently for at least 30 m; ability to participate in the study, based on the overall health and disease prognosis, in the opinion of the treating neurologist; no SMN-enhancing medications in the 6 months before screening. Salbutamol was permitted only if at a stable dose in the 6 months before screening.
Key exclusion criteria were long QT syndromes, concomitant use of medicinal products with a known potential to cause QTc prolongation, epilepsy and being currently on medication for epilepsy; breastfeeding or being pregnant at screening or planning to become pregnant at any time during the study period; treatment with an investigational drug, device, or biological agent in the 6 months before screening or during the study period; surgery for scoliosis or joint contractures in the 6 months before screening; history of drug allergy to any pyridine-containing substances or any amifampridine excipient. The full inclusion and exclusion criteria are available in the study protocol (Online Resource 1).
Study treatments
Amifampridine phosphate was provided in white 10 mg tablets. In the open-label run-in period, amifampridine was initially administered to all patients at 15 mg/day and titrated up to a maximum daily dose of 80 mg divided in three or four4 daily administrations based upon investigator’s judgment. Amifampridine dose and frequency had to be maintained stable in dose for at least 7 days before randomization. In the randomized, double-blinded crossover phase (Period 1 and Period 2), patients received their dosing regimen of amifampridine or a corresponding dose of placebo. Placebo was provided in tablets indistinguishable from amifampridine tablets and administered consistently to amifampridine dose regimen. Amifampridine and placebo were dispensed in bottles, individualized for each patient. To maintain blinding, bottles did not report information on the contained product (amifampridine or placebo) in the double-blinded phase. All doses were self-administered at home by the patients, except from one of the doses on the day of in-clinic visits. Treatment compliance was estimated based on the total dose of investigational product (amifampridine or placebo) that was not self-administered by patients and returned to investigators at in-clinic visits compared to the prescribed dose.
Study outcomes and end points
The primary safety end point was the characterization of the overall safety and tolerability of amifampridine compared to placebo. Adverse events (AE) were collected and classified according to MedDRA. All AE were collected from the first day of the run-in period to the end of study. Information on serious AE (SAE) were also collected during the screening period and in the 4 weeks after the last study visit. Treatment-emergent AE (TEAE) were defined as any AE starting from the date of randomization. For the primary safety end point, TEAE were compared between amifampridine and placebo. Other safety assessments included vital signs, clinical laboratory test results, ECGs, and physical evaluations. All safety assessments were performed before in-clinic dose administration.
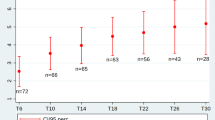
The primary efficacy end point of the study was the change from baseline (Day 0) in the HFMSE scores at 7, 14, 21, and 28 (end of study) days. HFMSE consists of 33 items, each scored from 0 to 2, up to a maximum of 66 points with higher scores indicating better motor performance.
Secondary quantitative efficacy end points were the change from baseline at 7, 14, 21, and 28 days in the 6-min walking test (6MWT), the time to rise from floor (from a supine position), the time to rise from chair, the time to climb four standardized stairs, and the time to walk 10 min [14]. Quality of life was evaluated with the Individualized Neuromuscular Quality of Life questionnaire (INQoL) or, in the case of pediatric patients, the Pediatric Quality of Life Inventory (PEDSQL) [30, 31]. Data on secondary efficacy outcomes were collected only during the double-blinded, crossover part of the trial and not in the open-label run-in period.
All efficacy assessments were performed on the day of every in-clinic study visit from baseline to end of study. HFMSE was also collected on the first day of the screening period and on the first day of the run-in period. Efficacy assessments were all performed after 45 min from the in-clinic AP dose administration at standardized times.
Statistical analysis
The sample size for this study was not formally calculated. Based on clinical considerations on the epidemiology of the disease, an anticipated sample size of approximately 12 patients to be randomized was estimated to be representative to evaluate the safety, tolerability, and evidence of efficacy of amifampridine in the target population.
Three study populations were defined for the analyses. The full analysis set (FAS) population consisted of all randomized patients who received at least one dose of amifampridine or placebo and had at least one post-treatment efficacy assessment. In the FAS population, patients were compared according to the treatment to which they were randomized in an intention-to-treat fashion. The per-protocol (PP) population consisted of a subset of patients from the FAS population who had no major protocol or inclusion/exclusion criteria deviations and who took at least 80% of the required treatment dose. The FAS population was used as the primary analysis set for all efficacy analyses. The safety population included all patients who were enrolled in the study and received at least one dose of amifampridine and all patients who entered the run-in period regardless of whether they were randomized to double-blind medication on day 0.
Descriptive statistics are presented as mean and standard deviation (SD) and median (range) for continuous variables and as counts (percentages) for categorical variables. For the primary efficacy end point analysis, a mixed effects linear model was used to estimate population least squares (LS) mean difference (MD) and 95% confidence intervals (CI) for each of the four period and sequence combination. Treatment (amifampridine or placebo) and treatment sequence (AP or PA) and the treatment by sequence interaction were entered in the model as fixed effects. Subject within sequence entered the model as a random effect with a block diagonal covariance structure. As for the primary efficacy end point analysis, quantitative secondary efficacy end points and INQoL were analyzed with the same linear mixed model with treatment and sequence entered as fixed effects and subjects within sequence entered as random effect with a block-diagonal covariance structure. There were no changes in the prespecified statistical analysis apart from INQoL statistics, which in the final analysis were both descriptive and inferential as opposed to only descriptitve as originally planned. Thus, results from the INQoL analysis should be interpreted as an exploratory post-hoc analysis. For safety analysis, all AE and SAE were summarized using system organ class and preferred terms and presented as counts and percentages. A p value ≤ 0.05 was considered statistically significant. Analyses were performed with SAS System, Version 9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Patients enrollment, randomization, and baseline characteristics
From 14 January 2019 to 17 September 2020, a total of 13 patients, 5 females and 8 males, with genetically confirmed SMA, due to homozygous exon 7 deletion for all patients, clinically defined as Type 3, were screened. All the patients were enrolled in the study and entered the run-in period. The mean age of the enrolled population was 34.5 (SD 11.3) years, with a median age of 35.0 years (range 18–53). Mean duration of treatment during the run-in period was 32.2 (SD 3.1) days, with a median of 31 days (range 29–38). At the end of the run-in period, 12 (92.3%) patients demonstrated an improvement in the HFMSE of at least 3 points at a stable amifampridine dose and were randomized, 6 to AP and 6 to PA sequences. Baseline demographic and clinical characteristics are presented in Table 1. HFMSE scores during the run-in period are described in Table 2. All 12 patients completed the study and were included in the Safety, FAS, and PP populations (Figure S1, Online Resource 3). One 45-year-old patient discontinued dosing and was not randomized since he did not show a 3-point improvement in HFMSE during the run-in period and was included in the Safety population only. No pediatric patients were included since all pediatric patients with SMA Type 3 followed at the center in Milan were receiving an SMN-enhancing medication at the time of study enrollment, while the center in Belgrade does not follow pediatric patients at all. Treatment compliance was similar between treatment sequences during Period 1 (91.67% and 92.78% for AP and PA sequences, respectively) and Period 2 (91.94% and 92.50% for AP and PA sequences, respectively). There were no major protocol deviations during the study. One 53-year-old male patient was inadvertently enrolled and randomized to the AP sequence, despite that the maximum age to enter the study was 50 years as per inclusion criteria. This deviation was considered minor and the patient was included in the analysis.
Primary safety end point and other safety evaluations
The primary safety analysis compared the occurrence of TEAE in patients receiving amifampridine to those receiving placebo (Table S1, Online Resource 3). Five (41.7%) and three (25.0%) patients reported at least one TEAE while receiving amifampridine or placebo, respectively. All TEAE were mild to moderate in severity. No SAE, including AE leading to hospitalization or deaths, or AE leading to study or study drug discontinuation were reported. No COVID-19 cases were reported and no patient tested positive for SARS-CoV-2 infection during the study period.
There were no clinically meaningful changes from screening observed for any mean hematology or mean chemistry laboratory parameters during the study (data not shown). One patient at Day 0 had a mild increase of transaminases that was considered possibly related to treatment with amifampridine phosphate. During the run-in period, when all participants were receiving amifampridine, 11 (84.6%) patients reported at least one AE (Table S2, Online Resource 3).
Primary efficacy end point
The primary efficacy end point was the change from Day 0 in HFMSE. A statistically significant improvement in HFMSE was observed in patients receiving amifampridine compared to those receiving placebo (LS MD = 0.729; 95% CI from 0.22 to 1.37; p = 0.0083) (Table 3). No significant period or carryover effects were observed in the model (p = 0.9449 and p = 0.1931, respectively). The percentage of HFMSE improved residual impairment for the different phases of the study (Table S3) and spaghetti plots describing randomized patients (Figure S2) are available in Online Resource 3.
Secondary efficacy end points
For the secondary efficacy end points, no significant differences from day 0 were observed in patients while receiving amifampridine compared to those receiving placebo in the 6-MWT, rising from the floor, rising from the chair, climbing four steps, or walking 10 m (Table 3). No significant period or carryover effects for all the secondary efficacy outcomes were observed.
In the INQoL exploratory analysis, amifampridine showed a statistically significant improvement in the fatigue subscale (p = 0.0081) and a significant reduction in the expected treatment effect subscale (p = 0.0120) compared to placebo, while for all other subscale scores the difference was non-significant (Table 3). A significant carryover effect was observed for pain (p = 0.0160) and emotions (p = 0.0237) subscales, while no significant period or carryover effects were observed for all the other INQoL subscales.
Classification of evidence
This investigation was designed to primarily evaluate the safety of amifampridine in ambulatory SMA Type 3 patients and to assess its efficacy by means of an improvement of the HFMSE. SMA-001 study provided Class II evidence that AP was safe and effective in treating ambulatory patients affected by SMA Type 3.
Discussion
During the SMA-001 trial, amifampridine was well tolerated by adult patients with SMA Type 3 at doses up to 80 mg per day. AE were all mild to moderate and were similar to those reported in clinical trials of amifampridine in LEMS patients [26, 32,33,34,35,36]. The most commonly occurring TEAEs considered related to treatment with amifampridine included oral and nasal paresthesia, oral hypoesthesia, flu-like symptoms, mild transaminases increase, and headache. No severe AE or treatment discontinuations due to AE were reported.
The SMA-001 study met the primary efficacy end point since patients receiving amifampridine had a statistically significant increase in HFMSE score, compared to those receiving placebo, in the double-blinded, crossover phase. However, the observed difference is not considered a clinically significant change as defined in the literature. In this regard, a recent study estimated that the minimal clinically important difference of HFMSE for ambulatory SMA Type 3 patients ranges between 1.5 and 4.3 points [37]. It is worthy of note though that during the run-in period of amifampridine titration, patients achieved a relevant improvement in motor function, as demonstrated by an increase in the mean value of the HFMSE score that exceeded the aforementioned cutoffs for clinically meaningful relevance. Other therapies specifically targeting the NMJ have been recently under investigation. Dalfampridine (4-aminopyridine) is a compound similar to amifampridine that was effective in improving fatigue and ambulation in multiple sclerosis patients [38]. In a randomized, placebo-controlled crossover trial, enrolling 11 adult SMA Type 3 ambulatory patients, which consisted of two crossover phases, a short-term and a long-term one, dalfampridine resulted in a mean difference of 1.84 and 0.6 points in the HFMSE score for the two phases, respectively, compared to placebo. These changes were not statistically significant [39]. The improvement in the long-term phase was similar to that observed in our patients in the primary efficacy outcome analysis. Nevertheless, in an observational cohort study on adult SMA Type 2 and 3 patients receiving nusinersen, ambulatory Type 3 patients achieved a mean improvement of 1.58 and 2.37 points at the HFMSE by 6 and 14 months, respectively, after treatment initiation [40]. Both changes were statistically significant and at 14 months the proportion of responders (i.e., achieving a 3-point improvement in HFMSE) was 48%. Baseline characteristics of SMA Type 3 patients included in this observational study were comparable to our trial and similar results were also reported in a further observational study on a German cohort of adult SMA patients [41]. Indeed, these observations are of great interest considering that in the run-in period of the SMA-001 study, 92% of patients achieved at least a three-point clinically meaningful response in HFMSE in about 1 month of amifampridine treatment. Actually, the fact that HFMSE score was already improved at randomization can partly explain the small effect observed afterward, during the double-blinded phase. A previous placebo-controlled crossover trial in MuSK MG patients showed that amifampridine significantly improved all disease-specific assessments evaluating disease severity and activities of daily life. Of note, likewise our study, this trial included a run-in phase and only responder patients entered the randomized phase. In MG patients, the magnitude of the mean difference of the effect was mainly due to the worsening of MG symptoms in patients while receiving placebo than in further improvement in patients while receiving amifampridine [22]. We observed similar behavior in the HFMSE score of SMA patients included in our study. However, we should also consider a possible learning effect on the execution of the scale, which could have reduced the entity of the measured worsening during placebo periods, accounting for the limited clinical significance of the improvement provided by amifampridine during the crossover phase. Although these results do not support a strong recommendation, they are encouranging with regard to the potential effect of amifampridine in improving motor function in SMA Type 3 patients which, unless being limited by the potential placebo effect (also potentially present in observational studies on nusinersen) and the short study duration, is obtained rapidly after a brief treatment period.
None of the quantitative secondary efficacy end points assessed in our study showed a significant difference between amifampridine and placebo. Similarly to the dalfampridine trial, 6MWT showed non-significant changes between active treatment and placebo [37, 39]. Interestingly, in our trial, amifampridine significantly improved fatigue in SMA Type 3 patients by means of a reduction in the INQoL fatigue subscale. Conversely, such improvement in fatigue was not observed in the dalfampridine trial. Discrepancies between changes in the 6MWT and the INQoL fatigue-related item have been already reported in a large cohort of Italian adult SMA patients treated with nusinersen and a further study showed that the perceived fatigue does not correlate with fatigability, which represents the objective measure of fatigue [42, 43]. Overall, these findings support the use of INQoL scale as a complementary tool in SMA patients’ evaluation. Although not statistically significant, amifampridine showed a tendency toward the improvement in the other disease symptoms and areas of life sections of the INQoL questionnaire, except for emotions. By contrast, the same population of treated patients reported a significant worsening of the expected treatment effect, compared to placebo. This was unexpected and we speculate that it might be related to the way the questions are shaped in the questionnaire and the time of its administration. Indeed, patients were asked whether they expect a future improvement from the current therapy in a moment (the randomization to the crossover phase) when they already achieved an improvement during the run-in phase and they are pretty stable.
Our study has some limitations. The sample size was small and a formal power analysis was not conducted. However, the number of enrolled patients was similar to the trial on dalfampridine, even though here the sample size was estimated on 6MWT, which was not the primary outcome measure outcome in our study [39]. Washout periods were not performed in our trial due to the short half-life of amifampridine [24, 25] and no period or carryover effects were found in the model for primary and secondary end points. Also, since SMA Type 3 does not have a rapid progression, all included patients were adults with a stable disease, and the overall study duration was of about 2 months, the presence of a possible period effect might be of limited to insignificant impact. In our study, pediatric patients could not be enrolled, since all SMA Type 3 patients followed at the participating centers were receiving an SMN-enhancing medication at the time of recruitment. Thus, the possible therapeutic role of amifampridine in pediatric patients should be evaluated in future trials.
Currently, preliminary results of a phase 2 clinical trial on the use of an acetylcholinesterase inhibitor in SMA patients support its potential use as an additive therapy [44]. Also, recent data suggested that NMJ transmission might be an SMN-independent therapeutic target [10], reinforcing the need for other pharmacological strategies to ameliorate motor function in SMA patients. In this landscape, larger, well-powered studies are needed to better define the role of amifampridine in the treatment of SMA patients as adjunctive therapy to SMN-enhancing medications for the cure of SMA.
Data availability
Data not provided in the article because of space limitations may be shared (anonymized) at the request of any qualified investigator for purposes of replicating procedures and results.
References
Hamilton G, Gillingwater TH (2013) Spinal muscular atrophy: going beyond the motor neuron. Trends Mol Med 19:40–50. https://doi.org/10.1016/j.molmed.2012.11.002
Ogino S, Leonard DGB, Rennert H et al (2002) Genetic risk assessment in carrier testing for spinal muscular atrophy. Am J Med Genet 110:301–307. https://doi.org/10.1002/ajmg.10425
Lunn MR, Wang CH (2008) Spinal muscular atrophy. Lancet (Lond, Engl) 371:2120–2133. https://doi.org/10.1016/S0140-6736(08)60921-6
Munsat TL, Davies KE (1992) International SMA consortium meeting (26–28 June 1992, Bonn, Germany). Neuromuscul Disord 2:423–428
Goulet BB, Kothary R, Parks RJ (2013) At the “junction” of spinal muscular atrophy pathogenesis: the role of neuromuscular junction dysfunction in SMA disease progression. Curr Mol Med 13:1160–1174. https://doi.org/10.2174/15665240113139990044
Kolb SJ, Kissel JT (2015) Spinal muscular atrophy. Neurol Clin 33:831–846. https://doi.org/10.1016/j.ncl.2015.07.004
Finkel RS, Mercuri E, Darras BT et al (2017) Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med 377:1723–1732. https://doi.org/10.1056/NEJMoa1702752
Darras BT, Masson R, Mazurkiewicz-Bełdzińska M et al (2021) Risdiplam-treated infants with type 1 spinal muscular atrophy versus historical controls. N Engl J Med 385:427–435. https://doi.org/10.1056/NEJMoa2102047
Mendell JR, Al-Zaidy S, Shell R et al (2017) Single-dose gene-replacement therapy for spinal muscular atrophy. N Engl J Med 377:1713–1722. https://doi.org/10.1056/NEJMoa1706198
Arnold WD, Severyn S, Zhao S et al (2021) Persistent neuromuscular junction transmission defects in adults with spinal muscular atrophy treated with nusinersen. BMJ Neurol Open 3:e000164. https://doi.org/10.1136/bmjno-2021-000164
Chaytow H, Faller KME, Huang Y-T, Gillingwater TH (2021) Spinal muscular atrophy: from approved therapies to future therapeutic targets for personalized medicine. Cell Rep Med 2:100346. https://doi.org/10.1016/j.xcrm.2021.100346
Wadman RI, Vrancken AFJE, van den Berg LH, van der Pol WL (2012) Dysfunction of the neuromuscular junction in spinal muscular atrophy types 2 and 3. Neurology 79:2050–2055. https://doi.org/10.1212/WNL.0b013e3182749eca
Pera MC, Luigetti M, Pane M et al (2017) 6MWT can identify type 3 SMA patients with neuromuscular junction dysfunction. Neuromuscul Disord 27:879–882. https://doi.org/10.1016/j.nmd.2017.07.007
Montes J, McDermott MP, Martens WB et al (2010) Six-minute walk test demonstrates motor fatigue in spinal muscular atrophy. Neurology 74:833–838. https://doi.org/10.1212/WNL.0b013e3181d3e308
Montes J, Dunaway S, Garber CE et al (2014) Leg muscle function and fatigue during walking in spinal muscular atrophy type 3. Muscle Nerve 50:34–39. https://doi.org/10.1002/mus.24081
de Groot IJM, de Witte LP (2005) Physical complaints in ageing persons with spinal muscular atrophy. J Rehabil Med 37:258–262. https://doi.org/10.1080/16501970510030156
Piepers S, van den Berg LH, Brugman F et al (2008) A natural history study of late onset spinal muscular atrophy types 3b and 4. J Neurol 255:1400–1404. https://doi.org/10.1007/s00415-008-0929-0
Maddison P, Newsom-Davis J, Mills KR (1998) Effect of 3,4-diaminopyridine on the time course of decay of compound muscle action potential augmentation in the Lambert–Eaton myasthenic syndrome. Muscle Nerve 21:1196–1198. https://doi.org/10.1002/(sici)1097-4598(199809)21:9%3c1196::aid-mus11%3e3.0.co;2-q
Maddison P, Newsom-Davis J, Mills KR (1998) Distribution of electrophysiological abnormality in Lambert–Eaton myasthenic syndrome. J Neurol Neurosurg Psychiatry 65:213–217. https://doi.org/10.1136/jnnp.65.2.213
Skeie GO, Apostolski S, Evoli A et al (2010) Guidelines for treatment of autoimmune neuromuscular transmission disorders. Eur J Neurol 17:893–902. https://doi.org/10.1111/j.1468-1331.2010.03019.x
Lindquist S, Stangel M (2011) Update on treatment options for Lambert–Eaton myasthenic syndrome: focus on use of amifampridine. Neuropsychiatr Dis Treat 7:341–349. https://doi.org/10.2147/NDT.S10464
Bonanno S, Pasanisi MB, Frangiamore R et al (2018) Amifampridine phosphate in the treatment of muscle-specific kinase myasthenia gravis: a phase IIb, randomized, double-blind, placebo-controlled, double crossover study. SAGE Open Med 6:2050312118819013. https://doi.org/10.1177/2050312118819013
Verma S, Mazell SN, Shah DA (2016) Amifampridine phosphate in congenital myasthenic syndrome. Muscle Nerve 54:809–810
Bever CTJ, Leslie J, Camenga DL et al (1990) Preliminary trial of 3,4-diaminopyridine in patients with multiple sclerosis. Ann Neurol 27:421–427. https://doi.org/10.1002/ana.410270411
CHMP Zenas, INN-amifampridine. https://www.ema.europa.eu/en/documents/assessment-report/firdapse-epar-public-assessment-report_en.pdf. Accessed 1 Nov 2021
Oh SJ, Shcherbakova N, Kostera-Pruszczyk A et al (2016) Amifampridine phosphate (Firdapse(®)) is effective and safe in a phase 3 clinical trial in LEMS. Muscle Nerve 53:717–725. https://doi.org/10.1002/mus.25070
O’Hagen JM, Glanzman AM, McDermott MP et al (2007) An expanded version of the Hammersmith Functional Motor Scale for SMA II and III patients. Neuromuscul Disord 17:693–697. https://doi.org/10.1016/j.nmd.2007.05.009
Pera MC, Coratti G, Forcina N et al (2017) Content validity and clinical meaningfulness of the HFMSE in spinal muscular atrophy. BMC Neurol 17:39. https://doi.org/10.1186/s12883-017-0790-9
Dwan K, Li T, Altman DG, Elbourne D (2019) CONSORT 2010 statement: extension to randomised crossover trials. BMJ 366:l4378. https://doi.org/10.1136/bmj.l4378
Sansone VA, Panzeri M, Montanari M et al (2010) Italian validation of INQoL, a quality of life questionnaire for adults with muscle diseases. Eur J Neurol 17:1178–1187. https://doi.org/10.1111/j.1468-1331.2010.02992.x
Orcesi S, Ariaudo G, Mercuri E et al (2014) A new self-report quality of life questionnaire for children with neuromuscular disorders: presentation of the instrument, rationale for its development, and some preliminary results. J Child Neurol 29:167–181. https://doi.org/10.1177/0883073813511859
Sanders DB, Howard JFJ, Massey JM (1993) 3,4-Diaminopyridine in Lambert–Eaton myasthenic syndrome and myasthenia gravis. Ann N Y Acad Sci 681:588–590. https://doi.org/10.1111/j.1749-6632.1993.tb22949.x
Sanders DB, Massey JM, Sanders LL, Edwards LJ (2000) A randomized trial of 3,4-diaminopyridine in Lambert–Eaton myasthenic syndrome. Neurology 54:603–607. https://doi.org/10.1212/wnl.54.3.603
McEvoy KM, Windebank AJ, Daube JR, Low PA (1989) 3,4-diaminopyridine in the treatment of Lambert–Eaton myasthenic syndrome. N Engl J Med 321:1567–1571. https://doi.org/10.1056/NEJM198912073212303
Oh SJ, Claussen GG, Hatanaka Y, Morgan MB (2009) 3,4-Diaminopyridine is more effective than placebo in a randomized, double-blind, cross-over drug study in LEMS. Muscle Nerve 40:795–800. https://doi.org/10.1002/mus.21422
Wirtz PW, Verschuuren JJ, van Dijk JG et al (2009) Efficacy of 3,4-diaminopyridine and pyridostigmine in the treatment of Lambert–Eaton myasthenic syndrome: a randomized, double-blind, placebo-controlled, crossover study. Clin Pharmacol Ther 86:44–48. https://doi.org/10.1038/clpt.2009.35
Stolte B, Bois J-M, Bolz S et al (2020) Minimal clinically important differences in functional motor scores in adults with spinal muscular atrophy. Eur J Neurol 27:2586–2594. https://doi.org/10.1111/ene.14472
Goodman AD, Brown TR, Cohen JA et al (2008) Dose comparison trial of sustained-release fampridine in multiple sclerosis. Neurology 71:1134–1141. https://doi.org/10.1212/01.wnl.0000326213.89576.0e
Chiriboga CA, Marra J, LaMarca NM et al (2020) Lack of effect on ambulation of dalfampridine-ER (4-AP) treatment in adult SMA patients. Neuromuscul Disord 30:693–700. https://doi.org/10.1016/j.nmd.2020.07.007
Maggi L, Bello L, Bonanno S et al (2020) Nusinersen safety and effects on motor function in adult spinal muscular atrophy type 2 and 3. J Neurol Neurosurg Psychiatry 91:1166–1174. https://doi.org/10.1136/jnnp-2020-323822
Hagenacker T, Wurster CD, Günther R et al (2020) Nusinersen in adults with 5q spinal muscular atrophy: a non-interventional, multicentre, observational cohort study. Lancet Neurol 19:317–325. https://doi.org/10.1016/S1474-4422(20)30037-5
Bonanno S, Zanin R, Bello L et al (2022) Quality of life assessment in adult spinal muscular atrophy patients treated with nusinersen. J Neurol. https://doi.org/10.1007/s00415-021-10954-3
Dunaway Young S, Montes J, Kramer SS et al (2019) Perceived fatigue in spinal muscular atrophy: a pilot study. J Neuromuscul Dis 6:109–117. https://doi.org/10.3233/JND-180342
Stam M, Wadman RI, Wijngaarde CA et al (2018) Protocol for a phase II, monocentre, double-blind, placebo-controlled, cross-over trial to assess efficacy of pyridostigmine in patients with spinal muscular atrophy types 2–4 (SPACE trial). BMJ Open 8:e019932. https://doi.org/10.1136/bmjopen-2017-019932
Acknowledgements
This trial was sponsored by Catalyst Pharmaceuticals, Inc.
Author information
Authors and Affiliations
Contributions
SB: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; analysis or interpretation of data. RG: drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. RZ: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; analysis or interpretation of data. VP: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data. CI: drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data. GB: drafting/revision of the manuscript for content, including medical writing for content; study concept or design. GI: drafting/revision of the manuscript for content, including medical writing for content; study concept or design. SI: drafting/revision of the manuscript for content, including medical writing for content; study concept or design. ZS: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data. SP: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data. LM: drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data.
Corresponding author
Ethics declarations
Conflicts of interest
S. Bonanno received honoraria for advisory board activities and compensation for travel and congress participation from Sanofi Genzyme, Biogen and Roche; R. Giossi received support for congress participation from Mylan; R. Zanin received funds for travel and congress participation from Biogen; V. Porcelli has nothing to disclose; C. Iannacone has received honoraria for statistical consultancy from Roche, Bayer-Schering, ReiThera, Abiogen, and MolMed; G. Baranello received speaker and consulting fees from Biogen, Novartis Gene Therapies, Inc. (AveXis), and Roche and has worked as principal investigator of SMA studies sponsored by Novartis Gene Therapies, Inc., and Roche; G. Ingenito has corporate appointment with Catalyst Pharmaceuticals; S. Iyadurai has corporate appointment with Catalyst Pharmaceuticals; Z. Stevic reports following conflicts of interest, all outside this work: receiving lecture honoraria from Pfizer and Roche; S. Peric reports following conflicts of interest, all outside this work: receiving lecture honoraria from Pfizer, Teva Actavis, Berlin Chemie Menarini, Mylan, Worwag, Adoc, and Salveo, research grants from Kedrion and Octapharma, consultant fees from argenx and Mylan, and travel grants from Octapharma, Kedrion, Teva Actavis, Sanofi Genzyme, Pfizer, Roche, Adoc, and Berlin Chemie Menarini, and reports no other conflicts of interest outside or related to this work; L. Maggi has received honoraria for speaking, advisory boards and compensation for congress participations from Sanofi Genzyme, Roche and Biogen, outside the submitted work.
Ethical standards
The trial was conducted in accordance with the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use Guidance Good Clinical Practice, the 1964 Declaration of Helsinki and its later amendments, local applicable law and regulatory requirements, was approved by institutional review boards and ethical committees of each participating center, and was registered in ClinicalTrials.gov (NCT03781479) and EUDRACT (2017-004600-22). All patients provided a written informed consent before any study procedure was performed, i.e., before the screening visit.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bonanno, S., Giossi, R., Zanin, R. et al. Amifampridine safety and efficacy in spinal muscular atrophy ambulatory patients: a randomized, placebo-controlled, crossover phase 2 trial. J Neurol 269, 5858–5867 (2022). https://doi.org/10.1007/s00415-022-11231-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11231-7