Abstract
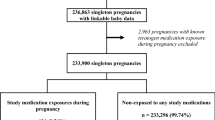
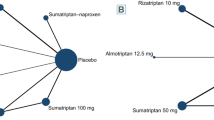
The present study aims to summarize the safety profile of the medications used to treat migraine during pregnancy by performing a systematic review and meta-analyses. The term “migrain*” combined with pregnancy terms were used to search Embase, PubMed, PsychInfo, Scopus, and Web of Science through 31 December 2020. Pooled prevalences of untreated and treated migraine patients were estimated using MetaXL software. Pooled odds ratios (OR) using random effects models were estimated in RevMan 5. All the identified studies assessed medications used to treat acute migraine. The pooled prevalence of adverse pregnancy outcomes in patients prescribed any migraine medication ranged from 0.4% (95% CI 0.2–0.7%) for stillbirth to 12.0% (95%CI 7.8–16.9%) for spontaneous abortions. Among untreated patients with migraine, the pooled prevalence of the assessed pregnancy outcomes ranged from 0.6% (95% CI: 0–1.7%) for stillbirth to 10.4% (95% CI: 8.9–12%) for gestational age < 37 weeks. Given the limited data, it was only possible to perform OR meta-analyses for triptans. The adjusted ORs for triptan users compared the general population were: for major malformations 1.07 (95%CI: 0.83–1.39, p = 0.60); birth weight < 2500g 1.18 (95%CI: 0.94–1.48, p = 0.16); gestational age < 37 weeks 1.49 (95% CI: 0.37–6.08, p = 0.58). In conclusion, triptans do not appear to increase the risk of pregnancy outcomes when compared to the general population. It was not possible to assess other migraine medications. Further studies are needed to investigate the safety of individual medications of acute and prophylactic migraine treatment among pregnant women.


Similar content being viewed by others
Availability of data and material
Upon request.
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211
Dodick DW (2018) A phase-by-phase review of migraine pathophysiology. Headache 58(Suppl 1):4–16
Dodick DW (2018) Migraine. Lancet 391(10127):1315–1330
Lipton RB et al (2007) Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68(5):343–349
Burch R (2020) Epidemiology and treatment of menstrual migraine and migraine during pregnancy and lactation: a narrative review. Headache 60(1):200–216
World Health Organization [WHO] (2011) Atlas of headache disorders and resources in the world 2011. A collaborative project of World Health Organization and Lifting the Burden. [cited 2020 November 19]; Available from http://apps.who.int/iris/handle/10665/44571
Amundsen S et al (2015) Pharmacological treatment of migraine during pregnancy and breastfeeding. Nat Rev Neurol 11(4):209–219
Tepper D (2015) Pregnancy and lactation–migraine management. Headache 55(4):607–608
Tanos V et al (2019) Review of migraine incidence and management in obstetrics and gynaecology. Eur J Obstet Gynecol Reprod Biol 240:248–255
Tomson T et al (2018) Comparative risk of major congenital malformations with eight different antiepileptic drugs: a prospective cohort study of the EURAP registry. Lancet Neurol 17(6):530–538
Saldanha IJ et al (2021) Management of primary headaches during pregnancy, postpartum, and breastfeeding: a systematic review. Headache 61(1):11–43
Sader E, Rayhill M (2018) Headache in pregnancy, the puerperium, and menopause. Semin Neurol 38(6):627–633
Bramer WM et al (2016) De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 104(3):240–243
Ouzzani M et al (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5(1):210
Shamseer L et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Doi SA et al (2015) Advances in the meta-analysis of heterogeneous clinical trials I: the inverse variance heterogeneity model. Contemp Clin Trials 45(Pt A):130–138
Barendregt JJ et al (2013) Meta-analysis of prevalence. J Epidemiol Community Health 67(11):974–978
Higgins JPT, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2020) Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane
O’Quinn S et al (1999) Pregnancy and perinatal outcomes in migraineurs using sumatriptan: a prospective study. Arch Gynecol Obstet 263(1–2):7–12
Kallen B, Nilsson E, Olausson PO (2011) Delivery outcome after maternal use of drugs for migraine: a register study in Sweden. Drug Saf 34(8):691–703
Nezvalova-Henriksen K, Spigset O, Nordeng H (2013) Triptan safety during pregnancy: a Norwegian population registry study. Eur J Epidemiol 28(9):759–769
Shuhaiber S et al (1998) Pregnancy outcome following first trimester exposure to sumatriptan. Neurology 51(2):581–583
Spielmann K et al (2018) Pregnancy outcome after anti-migraine triptan use: a prospective observational cohort study. Cephalalgia 38(6):1081–1092
Nezvalova-Henriksen K, Spigset O, Nordeng H (2009) Maternal characteristics and migraine pharmacotherapy during pregnancy: cross-sectional analysis of data from a large cohort study. Cephalalgia 29(12):1267–1276
Marchenko A et al (2015) Pregnancy outcome following prenatal exposure to triptan medications: a meta-analysis. Headache 55(4):490–501
Aukes AM et al (2019) Associations between migraine and adverse pregnancy outcomes: systematic review and meta-analysis. Obstet Gynecol Surv 74(12):738–748
Nezvalova-Henriksen K, Spigset O, Nordeng H (2010) Triptan exposure during pregnancy and the risk of major congenital malformations and adverse pregnancy outcomes: results from the Norwegian Mother and Child Cohort Study. Headache 50(4):563–575
Granella F et al (2000) Migraine with aura and reproductive life events: a case control study. Cephalalgia 20(8):701–707
Comission E (2020) European network of population based registries for the epidemiological surveillance of congenital anomalies. 2020 [cited 2020 August]. Available from https://eu-rd-platform.jrc.ec.europa.eu/eurocat_en
CDC (2019) Metropolitan atlanta congenital defects program (MACDP). [cited 2020 August]; Available from: https://www.cdc.gov/ncbddd/birthdefects/macdp.html
Olesen C et al (2000) Pregnancy outcome following prescription for sumatriptan. Headache 40(1):20–24
Acknowledgement
The ConcePTION project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 821520. This Joint Undertaking receives support from the European Union's Horizon 2020 research and innovation programme and EFPIA. The research leading to these results was conducted as part of the ConcePTION consortium. This paper only reflects the personal views of the stated authors.
Funding
Funding was provided by IMIConcePTION and Novartis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
DCD and SLL are employees of Novartis. MK is a former employee of Cognizant Technology Solutions on behalf of Novartis and a current employee of Barrington James Ltd on behalf of UCB. HL is a former employee of Eli Lilly and current employee of Gilead Science.
Ethical standards
This article does not contain any studies with human particpiants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Dudman, D.C., Tauqeer, F., Kaur, M. et al. A systematic review and meta-analyses on the prevalence of pregnancy outcomes in migraine treated patients: a contribution from the IMI2 ConcePTION project. J Neurol 269, 742–749 (2022). https://doi.org/10.1007/s00415-021-10534-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10534-5