Abstract
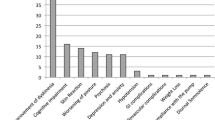
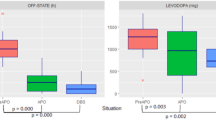
Prospective comparative long-term data on the effect of deep brain stimulation (DBS) of the subthalamic nucleus (STN) and continuous subcutaneous infusion of apomorphine (CSAI) in patients with advanced Parkinson disease (PD) are lacking. We report 5-year follow-up of 25 PD patients treated with either STN-DBS (n = 13) or CSAI (n = 12) who fulfilled CAPSIT-PD criteria. Cohorts were matched for disease duration and severity of motor complications. Baseline clinical and neuropsychological status did not differ among cohorts. Patients were assessed with the UPDRS, MMSE, HAMD-17 and Neuropsychiatric Inventory (NPI).Twelve subjects reached the 5-year follow-up with STN-DBS (one was lost at follow-up) versus two in the CSAI cohort. Drop-outs with CSAI were due to subcutaneous nodules (n = 2), insufficient control of motor fluctuations and dyskinesia (n = 4), death for unrelated reasons (n = 3) and one was lost at follow-up. Average apomorphine dose at last visit was 83.4 ± 19.2 mg/day and average treatment duration was 30 months. At 1-year as well as at last follow-up (intention-to-treat analysis), both therapies decreased daily off-time but only STN-DBS reduced dyskinesia duration and severity. Decrement of medications was greater with STN-DBS. There was a significant worsening of NPI after STN-DBS, primarily because four subjects developed apathy.

Similar content being viewed by others
Abbreviations
- CF:
-
Category fluency
- CPM:
-
Raven’s Colored Progressive Matrices
- CSAI:
-
Continuous subcutaneous apomorphine infusion
- CVLT:
-
California Verbal Learning Test
- HAMD-17:
-
Hamilton Depression Rating Scale-17
- H&Y:
-
Hoehn and Yahr
- MMSE:
-
Mini-Mental State Examination
- NPI:
-
Neuropsychiatric Inventory
- PF:
-
Phonemic fluency
- PWL:
-
Paired Word Learning
- STN-DBS:
-
Subthalamic nucleus-deep brain stimulation
- UPDRS:
-
Unified Parkinson Disease Rating Scale
References
Antonini A (2007) New strategies in motor parkinsonism. Parkinsonism Relat Disord 13:446–449
Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ Jr, CSP 468 Study Group et al (2009) Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA 301:63–73
Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, German Parkinson Study Group, Neurostimulation Section et al (2006) A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med 355:896–908
Deleu D, Hanssens Y, Northway MG (2004) Subcutaneous apomorphine: an evidence-based review of its use in Parkinson’s disease. Drugs Aging 21:687–709
García Ruiz PJ, Sesar Ignacio A, Ares Ares Pensado B, Castro García A, Alonso Frech F, Alvarez López M et al (2008) Efficacy of long-term continuous subcutaneous apomorphine infusion in advanced Parkinson’s disease with motor fluctuations: a multicenter study. Mov Disord 23:1130–1136
Antonini A, Tolosa E (2009) Apomorphine and levodopa infusion therapies for advanced Parkinson’s disease: selection criteria and patient management. Expert Rev Neurother 9:859–867
De Gaspari D, Siri C, Landi A, Cilia R, Bonetti A, Natuzzi F et al (2006) Clinical and neuropsychological follow up at 12 months in patients with complicated Parkinson’s disease treated with subcutaneous apomorphine infusion or deep brain stimulation of the subthalamic nucleus. J Neurol Neurosurg Psychiatry 77:450–453
Defer GL, Widner H, Marié RM, Rémy P, Levivier M (1999) Core assessment program for surgical interventional therapies in Parkinson’s disease (CAPSIT-PD). Mov Disord 14:572–584
Lang AE, Widner H (2002) Deep brain stimulation for Parkinson’s disease: patient selection and evaluation. Mov Disord 17:94–101
Grosset KA, Grosset DG (2006) Proposed dose equivalence for rapid switching between dopamine agonists in Parkinson’s disease. Clin Ther 28:1063–1064
Vergani F, Landi A, Antonini A, Parolin M, Cilia R, Grimaldi M et al (2007) Anatomical identification of active contacts in subthalamic deep brain stimulation. Surg Neurol 67:140–146
Isaias I, Tagliati M (2007) Deep brain stimulation programming for movement disorders. In: Tarsy D, Okun M, Starr P, Vitek J (eds) DBS in neurological and psychiatric disorders. Humana Press, New York
Friston KJ, Grasby PM, Bench CJ, Frith CD, Cowen PJ, Liddle PF et al (1992) Measuring the neuromodulatory effects of drugs in man with positron emission tomography. Neurosci Lett 141:106–110
Montoya A, Lal S, Menear M, Duplessis E, Thavundayil J, Schmitz N, Lepage M (2008) Apomorphine effects on episodic memory in young healthy volunteers. Neuropsychologia 46:292–300
Colosimo C, Merello M, Hughes AJ, Sieradzan K, Lees AJ (1998) Apomorphine responses in Parkinson’s disease and the pathogenesis of motor complications. Neurology 50:573–574
Nutt JG, Carter JH (2000) Apomorphine can sustain the long-duration response to l-dopa in fluctuating PD. Neurology 54:247–250
Manson AJ, Turner K, Lees AJ (2002) Apomorphine monotherapy in the treatment of refractory motor complications of Parkinson’s disease: long-term follow-up study of 64 patients. Mov Disord 17:1235–1241
Tyne HL, Parsons J, Sinnott A, Fox SH, Fletcher NA, Steiger MJ (2004) A 10 year retrospective audit of long-term apomorphine use in Parkinson’s disease. J Neurol 251:1370–1374
Katzenschlager R, Hughes A, Evans A, Manson AJ, Hoffman M, Swinn L et al (2005) Continuous subcutaneous apomorphine therapy improves dyskinesias in Parkinson’s disease: a prospective study using single-dose challenges. Mov Disord 20:151–157
Stocchi F, Vacca L, De Pandis MF, Barbato L, Valente M, Ruggieri S (2001) Subcutaneous continuous apomorphine infusion in fluctuating patients with Parkinson’s disease: long-term results. Neurol Sci 22:93–94
Kanovský P, Kubová D, Bares M, Hortová H, Streitová H, Rektor I, Znojil V (2002) Levodopa-induced dyskinesias and continuous subcutaneous infusions of apomorphine: results of a two-year, prospective follow-up. Mov Disord 17:188–191
Voon V, Kubu C, Krack P, Houeto JL, Tröster AI (2006) Deep brain stimulation: neuropsychological and neuropsychiatric issues. Mov Disord 21:305–327
Contarino MF, Daniele A, Sibilia AH, Romito LM, Bentivoglio AR, Gainotti G, Albanese A (2007) Cognitive outcome 5 years after bilateral chronic stimulation of subthalamic nucleus in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 78:248–252
Castelli L, Lanotte M, Zibetti M, Caglio M, Rizzi L, Ducati A et al (2007) Apathy and verbal fluency in STN stimulated PD patients. An observational follow-up study. J Neurol 254:1238–1243
Witt K, Daniels C, Reiff J, Krack P, Volkmann J, Pinsker MO et al (2008) Neuropsychological and psychiatric changes after deep brain stimulation for Parkinson’s disease: a randomised, multicentre study. Lancet Neurol 7:605–614
Sudhyadhom A, Bova FJ, Foote KD, Rosado CA, Kirsch-Darrow L, Okun MS (2007) Limbic, associative, and motor territories within the targets for deep brain stimulation: potential clinical implications. Curr Neurol Neurosci Rep 7:278–289
Forsaa EB, Larsen JP, Wentzel-Larsen T, Herlofson K, Alves G (2008) Predictors and course of health-related quality of life in Parkinson’s disease. Mov Disord 23:1420–1427
Simuni T, Sethi K (2008) Nonmotor manifestations of Parkinson’s disease. Ann Neurol 64:65–80
McKinlay A, Grace RC, Dalrymple-Alford JC, Anderson TJ, Fink J, Roger D (2008) Neuropsychiatric problems in Parkinson’s disease: comparisons between self and caregiver report. Aging Ment Health 12:647–653
Czernecki V, Schupbach M, Yaici S, Levy R, Bardinet E, Yelnik J et al (2008) Apathy following subthalamic stimulation in Parkinson disease: a dopa- mine responsive symptom. Mov Disord 23:964–969
Thobois S, Ardouin C, Lhommée E, Klinger H, Lagrange C, Xie J et al (2010) Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: predictors and underlying mesolimbic denervation. Brain 133:1111–1127
Le Jeune F, Drapier D, Bourguignon A, Peron J, Mesbah H, Drapier S et al (2009) Subthalamic nucleus stimulation in Parkinson disease induces apathy: a PET study. Neurology 73:1746–1751
Temel Y, Kessels A, Tan S, Topdag A, Boon P, Visser-Vandewalle V (2006) Behavioural changes after bilateral subthalamic stimulation in advanced Parkinson disease: a systematic review. Parkinsonism Relat Disord 12:265–272
Ellis C, Lemmens G, Parkes JD, Abbott RJ, Pye IF, Leigh PN, Chaudhuri KR (1997) Use of apomorphine in Parkinsonian patients with neuropsychiatric complications to oral treatment. Parkinsonism Relat Disord 3:103–107
Stibe CM, Lees AJ, Kempster PA, Stern GM (1998) Subcutaneous apomorphine in parkinsonian on-off oscillations. Lancet 1:403–406
Giovannoni G, O’Sullivan JD, Turner K, Manson AJ, Lees AJ (2000) Hedonistic homeostatic dysregulation in patients with Parkinson’s disease on dopamine replacement therapies. J Neurol Neurosurg Psychiatry 68:423–428
Morgante L, Basile G, Epifanio A, Spina E, Antonini A, Stocchi F et al (2003) Continuous apomorphine infusion and neuropsychiatric disorders: a controlled study in patients with advanced Parkinson’s disease. Neurol Sci 24:174–175
Morgante L, Basile G, Epifanio A, Spina E, Antonini A, Stocchi F et al (2004) Continuous apomorphine infusion (CAI) and neuropsychiatric disorders in patients with advanced Parkinson’s disease: a follow-up of two years. Arch Gerontol Geriatr 38:291–296
Parsons TD, Rogers SA, Braaten AJ, Woods SP, Tröster AI (2006) Cognitive sequelae of subthalamic nucleus deep brain stimulation in Parkinson’s disease: a meta-analysis. Lancet Neurol 5:578–588
Funkiewiez A, Ardouin C, Caputo E, Krack P, Fraix V, Klinger H et al (2004) Long term effects of bilateral subthalamic nucleus stimulation on cognitive function, mood, and behaviour in Parkinson’s disease. J Neurol Neurosurg Psychiatry 75:834–839
Kalbe E, Voges J, Weber T, Haarer M, Baudrexel S, Klein JC et al (2009) Frontal FDG-PET activity correlates with cognitive outcome after STN-DBS in Parkinson disease. Neurology 72:42–49
Cilia R, Marotta G, Landi A, Isaias IU, Mariani CB, Vergani F et al (2009) Clinical and cerebral activity changes induced by subthalamic nucleus stimulation in advanced Parkinson’s disease: a prospective case control study. Clin Neurol Neurosurg 111:140–146
Acknowledgments
All authors approve the contents of the submission and none has conflict of interest regarding this study. IUI, GR, AL, FN, CS, GP: stock ownership in medically-related fields, consultancies, advisory boards, partnerships, honoraria, grants, intellectual property rights, expert testimony and royalties for the past year and 12 months preceding this study: none. AA received speaking honoraria by GE Healthcare, Boehringer-Ingelheim, Solvay, Novartis, UCB and GSK not related to the conduction of this study; stock ownership in medically-related fields, advisory boards, partnerships, grants, intellectual property rights, expert testimony and royalties for the past year and 12 months preceding this study: none. The study was funded in part by a grant of the Grigioni Foundation for Parkinson’s disease.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Antonini, A., Isaias, I.U., Rodolfi, G. et al. A 5-year prospective assessment of advanced Parkinson disease patients treated with subcutaneous apomorphine infusion or deep brain stimulation. J Neurol 258, 579–585 (2011). https://doi.org/10.1007/s00415-010-5793-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-010-5793-z