Abstract
Purpose
Low diffusing capacity of the lung for carbon monoxide (DLCO) and spirometry values are associated with increased mortality risk. However, associations between mortality risk and cardiovascular disease with the transfer coefficient of the lung for carbon monoxide (KCO) and alveolar volume (VA) are unknown. This cohort study: (i) evaluated whether DLCO, KCO, and VA abnormalities are independently associated with cardiovascular morbidity and/or elevated mortality risk and, (ii) compared these associations with those using spirometry values.
Methods
Gas-diffusing capacity and spirometry data of 1165 adults seen at specialist respiratory outreach clinics over an 8-year period (241 with cardiovascular disease; 108 deceased) were analysed using multivariable Cox and logistic regression.
Results
DLCO, KCO, and VA values below the lower limit of normal (< − 1.64 Z-scores) were associated with elevated cardiovascular disease prevalence [respective odds ratios of 1.83 (95% CI 1.31–2.55), 1.56 (95% CI 1.08–2.25), 2.20 (95% CI 1.60–3.01)] and increased all-cause mortality risk [respective hazard ratios of 2.99 (95% CI 1.83–4.90), 2.14 (95% CI 1.38–3.32), 2.75 (95% CI 1.18–2.58)], after adjustment for factors including age, personal smoking, and respiratory disease. Compared to similar levels of spirometry abnormality, DLCO, KCO, and VA were associated with similar or greater mortality risk, and similar cardiovascular disease prevalence. Analysis of only those patients with clinical normal spirometry values (n = 544) showed these associations persisted for DLCO.
Conclusion
Low DLCO, KCO, and VA measurements are associated with cardiovascular disease prevalence. As risk factors of all-cause mortality, they are more sensitive than spirometry even among patients with no diagnosed respiratory disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is a growing evidence that low spirometric lung function is independently associated with increased future cardiovascular morbidity [1, 2], and overall mortality [1,2,3,4]. These associations have been demonstrated in asymptomatic patients without respiratory disease [4], and in patients whose spirometry Z-scores are reduced below zero but still within the clinically normal range (0 to − 1.64 Z-scores) [2, 5]. Comparatively fewer studies have reported on the association between diffusing capacity of the lung for carbon monoxide (DLCO) and mortality [6, 7]. Limited existing data suggests clinically abnormal DLCO is associated with elevated mortality risk with greater effect size than for spirometry [6, 7], even in the absence of diagnosed respiratory disease [6]. As yet, no studies have reported on associations between DLCO and overall cardiovascular morbidity. Furthermore, other key parameters of the diffusing capacity test, i.e., the transfer coefficient of the lung for carbon monoxide (KCO) and alveolar volume (VA), remain entirely unexplored for their association with either overall cardiovascular morbidity or all-cause mortality.
KCO is the rate of carbon monoxide (CO) removal from alveolar gas during the single breath hold manoeuvre [8], and is thus the change in log concentration of CO in the inspired gas volume (VI) divided by the breath hold time (10 ± 2 s [9] for an acceptable manoeuvre). Despite controversy surrounding the diagnostic utility of the KCO [10,11,12], it is useful in discerning patterns of parenchymal or obstructive pathologies [11, 13]. VA is an estimate of the volume of gas accessible to surfaces of gas exchange (the respiratory membrane that forms the alveolar wall) and equates to VI minus the volume of gas remaining in the large and small airways that does not participate in gas exchange [8]. The product of the KCO and VA is then adjusted for pressure to give the DLCO. The KCO and VA provide complementary information to the DLCO and afford insight into the root cause of DLCO abnormality, and both should be reported alongside the DLCO according to the current standard [9]. Given the clinical utility of these measurements and their availability to clinicians interpreting test results, assessing whether these parameters are also associated with future mortality risk would add valuable knowledge.
We utilised the data from regional and remote clinical populations seen and treated at specialist respiratory outreach clinics over an 8-year period to evaluate whether DLCO, KCO, and VA abnormalities are associated with future outcomes. The majority of participants were First Nations Australians who are, compared to non-First Nations people, at significantly increased risk of chronic respiratory [14] and cardiovascular disease [15] amongst other health disparities [16]. Investigating this question in an at-risk population is important, as such investigations are more likely to uncover significant associations. The objectives of our study were to (i) determine whether DLCO, KCO, and VA abnormalities are associated with cardiovascular morbidity and/or elevated mortality risk independent of other factors e.g., concurrent respiratory disease, and (ii) compare these associations with those involving FEV1, FVC, and FEV1/FVC values obtained from spirometry testing.
Materials and Methods
Study Design, Setting, and Participants
This is an 8-year retrospective analysis of adults referred to Indigenous Respiratory Outreach Care (IROC) clinics in regional and remote Queensland through their primary care physicians, community health workers, or self-referral. Inclusion criteria were adults aged 18–85 years at IROC clinic visit, who were medically reviewed with acceptable and repeatable [9] gas diffusing capacity and spirometry testing performed by a trained respiratory scientist between February 2012 and March 2020. Ethical approval for this study was granted by The Prince Charles Hospital Human Research Ethics Committee (Reference: HREC/2019/QPCH/58452).
Lung Function Testing
Gas diffusing capacity (single breath) and spirometry testing were performed according to European Respiratory Society (ERS) and American Thoracic Society (ATS) criteria [9, 17]. Patients were tested using an EasyOne Pro Lab (ndd Medizintechnik). Global Lung Function Initiative (GLI) multi-ethnic reference equations for spirometry (GLI-2012) [18] were used to generate predicted values for spirometry tests using the ‘other/mixed’ category, as this was found to be most suitable for use in First Nations Australian children and young adults [19]. GLI reference equations for gas diffusing capacity testing (GLI-2017), including the 2020 corrections [20], were applied to tests to derive Z-scores for each patient’s values [18, 20]. Notably, no ethnic correction is available. We used the ATS/ERS [21] four-tier grading with approximated Z-score equivalents proposed by Miller and Cooper [7] where GLI-derived [20] Z-scores ≥ − 1.64 were graded as normal, − 1.64 to − 3 as mild, − 3 to − 5 as moderate, and < − 5 as severe [7].
Data Verification and Definitions
Patient demographics, gas diffusing capacity and spirometry test data, cardiovascular disease, personal smoking status, household smoking data, and comorbidities recorded by a respiratory physician at baseline (first visit to IROC clinic) for each patient were collected. Mortality data was censored in August 2020, with both cause (where available) and date of death collected. Electronic and paper chart medical records were used to verify patient demographic, medical, personal smoking, and household smoking data.
Mortality data were collected from electronic medical records, using death certificates where available, or discharge summaries. Where cause of death was unclear or no information was available, cause of death was categorised as ‘unknown’. Chronic respiratory disease included respiratory physician diagnoses of chronic obstructive pulmonary disease, asthma, bronchiectasis, or other chronic pulmonary disease, and cardiovascular disease included ischaemic heart disease, congestive heart failure, stroke or transient ischaemic attack, and cardiac valve disease.
Statistical Analysis
Gas-diffusing capacity and spirometry data at first visit to IROC was used as the baseline for each patient included in this analysis. Odds ratios (ORs) for cardiovascular disease were calculated for gas diffusing capacity and spirometry Z-score tiers using logistic regression. Hazard ratios (HRs) for mortality events were calculated for baseline gas diffusing capacity and spirometry status using a Cox proportional hazards (PH) model after testing the PH assumption through visual inspection of log–log plots. Adjusted survival curves were generated assuming a Weibull distribution. Variables with p < 0.2 for any level on univariable modelling were included in final adjusted models. These variables included age, sex, personal smoking status, body mass index (BMI), First Nations status, and respiratory disease. Global Wald testing was performed on categorical variables. Stata17 (StataCorp LLC) was used for statistical analyses; two-tailed p values < 0.05 were considered significant.
Results
Over an 8-year period, 1853 patients were seen at adult IROC clinics. Of these, 1327 patients had gas diffusion capacity testing. We excluded 48 patients with no paper chart or electronic medical records, 14 patients aged > 85 years, and a further 100 who did not meet acceptability and repeatability criteria for gas diffusion capacity [9] or spirometry testing [17] (Fig. 1). Thus, a total of 1165 patients were included in this analysis where their demographic and gas diffusing capacity data are summarised in Table 1. The median time from baseline visit to data census was 3.5 years (IQR 2–5). Excluded participants were similar in age (59 years) with similar proportions of females (51%), were less likely to be current (24%) or former (24%) smokers but had similar cardiovascular disease prevalence (20%).
Gas diffusing capacity values for included patients were below the lower limit of normal (− 1.64 Z-score) for 517 (40%) DLCO, 298 (23%) KCO, and 451 (35%) VA results. Summary cardiovascular disease and mortality data for included patients are shown in Table 2.
Cardiovascular Morbidity
A total of 241 (21%) of patients had diagnosed cardiovascular disease at baseline. Our adjusted models showed abnormal DLCO (OR = 1.83, 95% CI 1.31, 2.55), KCO (OR = 1.56, 95% CI 1.08, 2.25), and VA (OR = 2.20, 95% CI 1.60, 3.01) were each associated with cardiovascular disease, independent of smoking status. Complete per-tier modelling is shown in Table 3.
When we limited the gas diffusing capacity data to those whose FEV1 and FVC values were within the clinically normal range (n = 544 patients including 26 deceased), DLCO (p = 0.01) and VA (p = 0.04) were still significantly associated with cardiovascular disease, while KCO (p = 0.14) was not. Additional analysis showed no effect modification of abnormal FEV1/FVC (< 0.7) on gas diffusing capacity values and associations with cardiovascular disease.
Mortality and Survival Distributions
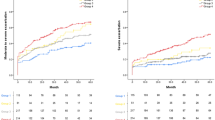
By August 2020, 108 (9%) patients had died. Respiratory-related death occurred in 42 (39%) patients, cardiovascular-related death in 25 (23%) patients, and other causes of death in 15 (14%), while we were unable to retrospectively determine cause of death in 16 (15%) patients. Adjusted survivor functions for gas-diffusing capacity and spirometry Z-score tiers are graphed in Fig. 2. The set of four curves appeared similar between gas diffusing capacity and spirometry tests, although the proportion of patients surviving appeared significantly less for severe DLCO, KCO, or VA grading. Of 84 patients with a DLCO below the lower limit of normal at baseline, only two had a lower KCO Z-score, and ten a lower VA Z-score.
Survival estimates for A DLCO, B KCO, C VA, D FEV1, E FVC, and F FEV1/FVC Z-score tiers [Severity tiers for Z-scores; normal (> − 1.64), mild (< − 1.64 to − 3), moderate (− 3 to − 5) and severe (< − 5) are shown on graph as lightest to darkest] over time. DLCO diffusing capacity of the lung for carbon monoxide, KCO transfer coefficient of the lung for carbon monoxide, VA alveolar volume, FEV1 forced expiratory volume in one second, FVC forced vital capacity
Multivariable Survival Modelling
DLCO (HR = 2.99, 95% CI 1.83, 4.90), KCO (HR = 2.14, 95% CI 1.38, 3.32), VA (HR = 1.75, 95% CI 1.18, 2.58) Z-scores below the lower limit of normal were associated with increased risk of all-cause mortality after adjustment for age, sex, smoking status, body mass index, First Nations status, and respiratory disease. Full per-tier modelling is available in Table 4, and adjusted survivor functions are plotted in Fig. 2.
Analysis restricted to only patients with normal FEV1 and FVC values showed that DLCO (p = 0.03) was still associated with increased overall mortality risk, while KCO (p = 0.16) and VA (p = 0.08) were not. Further analysis showed no effect modification of abnormal FEV1/FVC (< 0.7) on gas diffusing capacity values and survival.
Comparison to Spirometry
Median spirometry values were above the lower limit of normal (− 1.64 Z-score), with 575 (49%) FEV1, 457 (39%) FVC, and 363 (31%) FEV1/FVC results falling below the lower limit. Abnormal FEV1 (OR = 1.45, 95% CI 1.06, 1.97) and FVC (OR = 1.93, 95% CI 1.42, 2.63) were both associated with cardiovascular disease, with adjusted effect sizes for each tier similar to those seen for gas diffusing capacity measurements (Table 3). Abnormal FEV1 (HR = 2.21, 95% CI 1.41, 3.47), and FVC (HR = 2.57, 95% CI 1.71, 3.86) were also associated with elevated mortality risk, with adjusted effect sizes similar or less than equivalent gas diffusing capacity tiers (Table 4). We observed no associations between FEV1/FVC and either cardiovascular disease prevalence (OR = 0.84, 95% CI 0.60, 1.18) or elevated mortality risk (HR = 1.13, 95% CI 0.75, 1.70). In the subgroup of patients with normal spirometry, data relating to their gas diffusing capacity values with cardiovascular morbidity and adjusted survival curves and modelling were presented above.
Discussion
In this study of 1165 predominantly First Nations Australian patients seen at specialist respiratory outreach clinics in regional and remote Queensland, we found that DLCO, KCO, VA, FEV1, and FVC values below the clinically normal range were associated with cardiovascular disease and mortality. This finding was independent of factors such as age, sex, personal smoking, BMI, and concurrent respiratory disease. Mortality risk almost doubled for each category increase in DLCO, KCO, and VA tier (normal, mild, moderate, and severe) based on Z-scores in unadjusted but not adjusted models. While two other studies [6, 7] have reported similar findings with respect to the association of low diffusing capacity with future mortality, our study provides the first evidence that the KCO and VA, in addition to the DLCO, are each independent prognostic markers of mortality. Further, our data suggests estimated survival is similar or lower for gas diffusing capacity compared to equivalent spirometry Z-score tiers, suggesting that the former is more sensitive than the latter.
Neas et al. investigated pulmonary function as a predictor of mortality using First National Health and Nutrition Examination Survey (NHANES I) data [6]. Their analysis showed each 10% decrement in DLCO percentage predicted below the lower limit of normal was associated with increased mortality [risk ratio (RR) = 1.33, 95% CI 1.21, 1.45], with a greater effect size than for either FEV1 (RR = 1.15, 95% CI 1.10, 1.19) or FVC (RR = 1.15, 95% CI 1.10, 1.20) [6]. This association persisted after including only participants with an FEV1 > 90% predicted (RR = 1.30, 95% CI 1.08, 1.56) [6]. Our similar analysis with stricter criteria, requiring both normal FEV1 and FVC, support and extend this existing evidence and showed DLCO values below the lower limit of normal were still significantly associated with mortality. Our data suggest these associations with both all-cause mortality and cardiovascular disease occur independently of FEV1/FVC.
Recent analysis by Miller and Cooper [7] explored several grading schemes and showed the ATS/ERS four-tier system in combination with GLI reference equations [9] was best related to survival in a large (n = 13,829) clinical population and so were chosen for our analysis. Miller and Cooper reported a similarly large increase in risk related to DLCO Z-score abnormality (mild: HR = 2.0, 95% CI 1.8, 2.1; moderate: HR = 3.4, 95% CI 3.2, 3.7; severe: HR = 6.2, 95% CI 6.0, 7.3) [7] and these hazard ratios were consistently higher than those for FEV1 and FVC across each tier of Z-score grading [7]. In concordance in our study, the largest effect across both cardiovascular morbidity and survival analysis were seen in the DLCO, except for the mild tier in which there was significant variation. Our effect size estimates have wide confidence intervals that make differences in the associations of outcomes with gas diffusing capacity and spirometry measurements difficult to discern, however estimates for the severe Z-score tier appear much larger for gas diffusing capacity measurements than for spirometry. Taken together with previously published evidence [6, 7], our study supports that associations between cardiovascular morbidity and overall survival to DLCO, KCO, VA are similar or stronger than for equivalent FEV1, FVC, and FEV1/FVC values.
Our data supports a small but growing body of evidence that suggests that lung function impairment, as measured by spirometry and gas diffusing capacity, is associated with poor patient outcomes and this remains true in the absence of diagnosed respiratory disease [4, 6]. The limitations of diagnostic labels have, in part, given rise to the treatable traits paradigm, where clinical interventions are guided by genetic, phenotypic, and biomarker characteristics amongst others [22, 23]. Airflow limitation, eosinophilic airway inflammation, and emphysema [22] are examples of treatable traits that are identifiable using lung function testing, and our findings suggest these tests could also be applied outside of the respiratory clinic domain. Portability, (relative) low cost, standardisation, and well-defined guidelines for interpretation are key strengths of lung function tests that enable their use in a range of settings, including within office-based and outreach clinics. Broad application of the treatable traits approach necessitates the use of identification markers that are not isolated to large tertiary facilities in urban centres, but those that are ubiquitous and practical across the spectrum of clinical settings.
Our study has several important limitations. Firstly, we cannot discount the possibility of spectrum bias influencing our data, owing to the large number of clinic locations throughout Queensland. We are also reliant on mortality data reported in paper charts and electronic medical records, and so there may be a minority of deaths in this cohort that have not been accounted for. Secondly, although the GLI-2012 ‘other/mixed’ reference category has been found to be suitable for use in First Nations Australian children and young adults, we cannot be certain about its suitability to the adult population. GLI-2017 reference values were developed using participants of European ancestry and no ethnic correction is available [20]. It is unlikely these values are suitable for use in First Nations Australians. Thirdly, although we found significant associations, our data is limited by sample size, particularly within the severe Z-score tier of some measurements. This limits our ability to compare associations with outcome between gas diffusing capacity and spirometry measurements. Finally, our data includes adults seen in regional and remote Queensland, and so we cannot be certain about the generalisability of our findings to other populations more broadly.
In conclusion, our data suggests DLCO, KCO, and VA measurements below the clinically normal range are associated with cardiovascular disease and all-cause mortality. These associations are independent of factors such as age, personal smoking, and concurrent respiratory disease and persist even when spirometry values are normal. Our data also shows DLCO, KCO, and VA measurements were associated with similar or elevated mortality risk compared to spirometry equivalent spirometry Z-score tiers. Overall, DLCO, KCO, and VA are prognostic markers of cardiovascular disease and all-cause mortality, with DLCO the most capable measurement for this purpose as an additional prognostic marker available to clinicians.
References
Magnussen C, Ojeda FM, Rzayeva N, Zeller T, Sinning CR, Pfeiffer N, Beutel M, Blettner M, Lackner KJ, Blankenberg S, Munzel T, Rabe KF, Wild PS, Schnabel RB, Gutenberg Health Study Investigators (2017) FEV1 and FVC predict all-cause mortality independent of cardiac function—results from the population-based Gutenberg Health Study. Int J Cardiol 234:64–68. https://doi.org/10.1016/j.ijcard.2017.02.012
Duong M, Islam S, Rangarajan S, Leong D, Kurmi O, Teo K, Killian K, Dagenais G, Lear S, Wielgosz A, Nair S, Mohan V, Mony P, Gupta R, Kumar R, Rahman O, Yusoff K, du Plessis JL, Igumbor EU, Chifamba J, Li W, Lu Y, Zhi F, Yan R, Iqbal R, Ismail N, Zatonska K, Karsidag K, Rosengren A, Bahonar A, Yusufali A, Lamelas PM, Avezum A, Lopez-Jaramillo P, Lanas F, O’Byrne PM, Yusuf S, PURE Investigators (2019) Mortality and cardiovascular and respiratory morbidity in individuals with impaired FEV1 (PURE): an international, community-based cohort study. Lancet Glob Health 7(5):e613–e623. https://doi.org/10.1016/S2214-109X(19)30070-1
Sabia S, Shipley M, Elbaz A, Marmot M, Kivimaki M, Kauffmann F, Singh-Manoux A (2010) Why does lung function predict mortality? Results from the Whitehall II cohort study. Am J Epidemiol 172(12):1415–1423. https://doi.org/10.1093/aje/kwq294
Burney PG, Hooper R (2011) Forced vital capacity, airway obstruction and survival in a general population sample from the USA. Thorax 66(1):49–54. https://doi.org/10.1136/thx.2010.147041
Collaro AJ, Chang AB, Marchant JM, Chatfield MD, Dent A, Blake T, Mawn P, Fong K, McElrea MS (2021) Associations between lung function and future cardiovascular morbidity and overall mortality in a predominantly First Nations population: a cohort study. Lancet Reg Health-Western Pac 13:100188. https://doi.org/10.1016/j.lanwpc.2021.100188
Neas LM, Schwartz J (1998) Pulmonary function levels as predictors of mortality in a national sample of US adults. Am J Epidemiol 147(11):1011–1018. https://doi.org/10.1093/oxfordjournals.aje.a009394
Miller MR, Cooper BG (2021) Reduction in TLCO and survival in a clinical population. Eur Respir J. https://doi.org/10.1183/13993003.02046-2020
Hughes JM, Pride NB (2012) Examination of the carbon monoxide diffusing capacity (DLCO) in relation to its KCO and VA components. Am J Respir Crit Care Med 186(2):132–139. https://doi.org/10.1164/rccm.201112-2160CI
Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, Kendrick A, MacIntyre NR, Thompson BR, Wanger J (2017) ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J. https://doi.org/10.1183/13993003.00016-2016
van der Lee I, Zanen P, van den Bosch JM, Lammers JW (2006) Pattern of diffusion disturbance related to clinical diagnosis: the KCO has no diagnostic value next to the DLCO. Respir Med 100(1):101–109. https://doi.org/10.1016/j.rmed.2005.04.014
Cotton DJ, Graham BL (2013) The usefulness of Kco is questionable. Am J Respir Crit Care Med 187(6):660. https://doi.org/10.1164/ajrccm.187.6.660
Hughes JM, Pride NB (2001) In defence of the carbon monoxide transfer coefficient Kco (TL/VA). Eur Respir J 17(2):168–174. https://doi.org/10.1183/09031936.01.17201680
Fitting J (2004) Transfer factor for carbon monoxide: a glance behind the scene. Swiss Med Wkly 134:413–418
Australian Institute of Health and Welfare (2017) The burden of chronic respiratory conditions in Australia: a detailed analysis of the Australian Burden of Disease Study 2011. Australian Institute of Health and Welfare, Canberra
Australian Health Ministers’ Advisory Council (2020) Aboriginal and Torres Strait Islander Health Performance Framework-Summary report 2020. Australian Health Ministers’ Advisory Council, Canberra
Kirmayer LJ, Brass G (2016) Addressing global health disparities among Indigenous peoples. Lancet 388(10040):105–106. https://doi.org/10.1016/s0140-6736(16)30194-5
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, Hallstrand TS, Kaminsky DA, McCarthy K, McCormack MC, Oropez CE, Rosenfeld M, Stanojevic S, Swanney MP, Thompson BR (2019) Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med 200(8):e70–e88. https://doi.org/10.1164/rccm.201908-1590ST
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Ip MS, Zheng J, Stocks J, Initiative ERSGLF (2012) Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343. https://doi.org/10.1183/09031936.00080312
Blake TL, Chang AB, Chatfield MD, Marchant JM, McElrea MS (2020) Global Lung Function Initiative-2012 ‘other/mixed’ spirometry reference equation provides the best overall fit for Australian Aboriginal and/or Torres Strait Islander children and young adults. Respirology 25(3):281–288. https://doi.org/10.1111/resp.13649
Stanojevic S, Graham BL, Cooper BG, Thompson BR, Carter KW, Francis RW, Hall GL, Global Lung Function Initiative TLCO Working Group (2017) Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J. https://doi.org/10.1183/13993003.00010-2017
Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, Jensen R, Johnson DC, MacIntyre N, McKay R, Miller MR, Navajas D, Pedersen OF, Wanger J (2005) Interpretative strategies for lung function tests. Eur Respir J 26(5):948–968. https://doi.org/10.1183/09031936.05.00035205
Agusti A, Bel E, Thomas M, Vogelmeier C, Brusselle G, Holgate S, Humbert M, Jones P, Gibson PG, Vestbo J, Beasley R, Pavord ID (2016) Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 47(2):410–419. https://doi.org/10.1183/13993003.01359-2015
Agusti A, Barnes N, Cruz AA, Gibson PG, Heaney LG, Inoue H, Leather D, Martinez FJ, McDonald VM, Oppenheimer J, Papi A, Pavord ID, Thomas M, Walker S, Yates L (2021) Moving towards a treatable traits model of care for the management of obstructive airways diseases. Respir Med 187:106572. https://doi.org/10.1016/j.rmed.2021.106572
Acknowledgements
We thank the staff and patients who participated in IROC clinics, and their supporting local communities.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The authors received no specific funding for this work. AJC is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship (APP2003334). JMM is supported by a Children’s Hospital Foundation fellowship (RPC0772019). ABC is supported by a NHMRC Senior Practitioner Fellowship (APP1154302) and Children’s Hospital Foundation (top-up #50286) and reports multiple grants from NHMRC and other fees to the institution from work relating to IDMC membership of an unlicensed vaccine (GSK), and a COVID-19 vaccine (Moderna) outside the submitted work. MSM reports other grants from Children’s Hospital Foundation.
Author information
Authors and Affiliations
Contributions
AJC, ABC, JMM, and MSM contributed to the study design. AJC, KMF, and AD contributed to the data collection and collation. AJC and MDC were responsible for the statistical analysis. All authors contributed to the interpretation of the data, participated in the writing and critical revision of the manuscript, and have approved the final version for submission. AJC and MSM verified the underlying data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Collaro, A.J., Chang, A.B., Marchant, J.M. et al. Association of Gas Diffusing Capacity of the Lung for Carbon Monoxide with Cardiovascular Morbidity and Survival in a Disadvantaged Clinical Population. Lung 200, 783–792 (2022). https://doi.org/10.1007/s00408-022-00580-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00580-9