Abstract
Purpose
Anesthetics are required for procedures that deliver drugs/biologics, infectious/inflammatory agents, and toxicants directly to the lungs. However, the possible confounding effects of anesthesia on lung inflammation and injury are underreported. Here, we evaluated the effects of two commonly used anesthetic regimens on lung inflammatory responses to ozone in mice.
Methods
We tested the effects of brief isoflurane (Iso) or ketamine/xylazine/atipamezole (K/X/A) anesthesia prior to ozone exposure (4 h, 3 ppm) on lung inflammatory responses in mice. Anesthesia regimens modeled those used for non-surgical intratracheal instillations and were administered 1–2 h or 24 h prior to initiating ozone exposure.
Results
We found that Iso given 1–2 h prior to ozone inhibited inflammatory responses in the lung, and this effect was absent when Iso was given 23–24 h prior to ozone. In contrast, K/X/A given 1–2 h prior to ozone increased lung and systemic inflammation.
Conclusion
Our results highlight the need to comprehensively evaluate anesthesia as an experimental variable in the assessment of lung inflammation in response to ozone and other inflammatory stimuli.
Similar content being viewed by others
Introduction
Ozone (O3) is a widespread air toxicant with well-established inflammatory effects in the lungs, but it also affects other organs, such as the liver, spleen, and brain. Approaches for selectively inhibiting lung inflammation may provide insight on the systemic effects of O3 and could involve direct delivery of substances to the lungs through the trachea prior to O3 exposure. Volatile anesthetics such as isoflurane are frequently used for intratracheal instillations and other surgeries [1,2,3]. However, isoflurane can have anti-inflammatory effects [4, 5], which may be most potent in the respiratory tract since it is the first site of exposure. Injectable anesthetics such as ketamine/xylazine are also used for intratracheal instillations [6], but may also modulate inflammatory responses [7,8,9,10]. Currently, little is known about how anesthesia prior to O3 exposure affects inflammatory responses. To test this, we exposed mice to isoflurane (Iso) or ketamine/xylazine followed by atipamezole reversal (K/X/A) prior to O3. Conditions of anesthesia were designed to replicate those used for non-surgical intratracheal instillations of substances such as drugs or biologics that modulate effects of O3 on the lungs in mice. The day after O3 exposure, mice were evaluated for markers of systemic and pulmonary inflammation. We found that Iso and K/X/A modify lung inflammation in response to O3.
Methods
Animal Use
Female CD-1 mice, age 10–12 weeks, (Charles River Laboratories, Malvern, PA, USA) were used for air and O3 exposures. Females were used because they have more robust inflammatory responses to O3. Mice were given food and water ad libitum and kept on a 12-h light/12-h dark cycle. Protocols were approved by the institutional animal care and use committee of the VA Puget Sound Healthcare System.
Anesthesia
Isoflurane was administered by first weighing all mice, followed by placing mice in an induction chamber filled with 4% isoflurane for 1.5 min and then transferring to a nose cone where 3% isoflurane was used to maintain deep anesthesia for 5 min, which approximates the maximum time that a skilled technician needs to complete an intratracheal injection. Control mice were placed in the empty anesthesia chamber with room air for 1.5 min and then returned to their home cage. 1–2 h or 23–24 h after isoflurane exposure, O3 exposures began. Ketamine (80 mg/kg) and xylazine (10 mg/kg) in sterile saline were administered by intraperitoneal injection (IP). 20–30 min after the injection, mice were given 1 mg/kg atipamezole IP to quickly counteract the effects of the anesthesia. Control mice were given IP saline. 1–2 h after the atipamezole injection, O3 exposures began. All mice were numbered with a marker to track their identity, and mice were randomized so that the average time between anesthesia and air/ozone exposure was equivalent between groups. A schematic of O3 and anesthesia regimens is shown in Fig. 1.
O 3 Exposure
O3 exposures were conducted at 3 ppm for 4 h (10:00–14:00), which induce a robust inflammatory response without inducing respiratory distress [11]. For the exposure duration, 3–4 mice were housed in standard mouse cages with free access to water, but without food or bedding to prevent consumption of ozonated food or bedding materials. Up to four cages at a time were placed in a 30″ × 20″ × 20″ polypropylene chamber where O3 (3 ppm, chamber 1) or compressed dry air (chamber 2) was pumped into the chamber at equivalent rates. Anesthesia and O3 exposures were replicated at least once to capture day-to-day variability, and results for each dose showed consistent trends. O3 levels in the chambers were generated and regulated using an Oxycycler AT42 system (BioSpherix, Parish NY, USA). Prior to each experiment, the system was calibrated using a model 106-L O3 detector (2B Technologies, Boulder, CO, USA), and O3 levels were recorded from an inlet valve in one of the O3-exposed mouse cages every 10 s for the duration of exposures. In all experiments, O3 achieved its target concentration within 10 min, and levels were regulated within 10% of the target concentration (3 ppm ± 0.3 ppm) thereafter.
Blood Collection and Serum Amyloid A Measurement
22–24 h after the start of O3 exposure (12:00–14:00), mice were re-weighed and deeply anesthetized with IP urethane (Millipore Sigma, St. Louis, MO, USA). Blood was collected from the abdominal aorta, allowed to clot for 30 min, and then placed on ice. Blood was centrifuged at 2500×g for 15 min and serum was collected, aliquoted, and frozen at − 80 °C. Serum was diluted 1/10,000 for mice exposed to ozone and 1/50 for mice not exposed to ozone. Serum amyloid A (SAA) mouse duoset kits (R and D systems, Minneapolis, MN, USA) were used to quantify SAA in serum.
WLL and Pulmonary Inflammation Assessment
Whole-lung lavage (WLL) was performed on mice by perfusing and aspirating the lungs through the trachea three times with 1 mL sterile phosphate-buffered saline (3 mL total). WLL fluid was stored on ice and centrifuged at 200×g for 5 min at 4 °C. The supernatant was removed and 0.5 mLs of supernatant were reserved to resuspend the cell pellet. The remainder was frozen for measurement of total WLLL protein, which was performed using a microBradford assay. Total cells were manually counted using a hemacytometer. Differential cell counts were performed on Hemacolor-stained cytocentrifuge preparations. Cell counts were performed using ImageJ, and at least 200 cells were counted to determine relative cell proportions.
Statistics
Statistical analysis was done with Prism 8.4.2 (GraphPad Software, San Diego, CA, USA). Data are reported as mean ± SD and analyzed by two-way ANOVA for main effects and interactions and Tukey’s multiple comparisons test for comparisons of group means.
Results
Effects of Isoflurane and Ketamine/Xylazine/Atipamezole Anesthesia on Ozone-Induced Pulmonary Inflammation and Injury
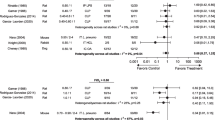
We first determined whether O3-induced responses in the lungs differed with Iso or K/X/A. Since drugs or other interventions to be administered intratracheally would ideally be given a short time before exposure to ozone to maximize their effects/minimize their metabolism, we evaluated anesthesia administration at 1–2 h prior to ozone exposure. We chose 1–2 h because this time frame allows the mice to recover from anesthesia and also reflects a time window that is typically sufficient for an administered drug to sufficiently activate/inhibit its biological target. A pilot study indicated that Iso given 1–2 h before O3 inhibited inflammation, suggesting that this regimen is unsuitable for studying anti-inflammatory interventions for O3 exposure. Therefore, we included a 24-h Iso pre-exposure in experimental replicates to determine whether the anti-inflammatory effects of Iso were sustained. The 24-h time point was chosen because the Iso and O3 exposures could then occur at approximately the same time of day as the 1–2-h Iso pre-exposure group. We compared K/X/A to Iso 1–2-h pre-O3 exposure to determine whether K/X/A is a suitable alternative anesthesia regimen to Iso (Schematics in Fig. 1A, B). Although the controls for ketamine were IP injected with saline, whereas Iso controls were not, we found that IP injections did not significantly influence the measured outcomes, and so we combined the Iso and Ketamine no anesthesia control groups for analysis. O3 significantly increased WLL total cells, macrophages, and neutrophils except in the 1–2-h Iso group (Fig. 2A–C). We further show that mice exposed to K/X/A and O3 had significantly increased WLL total cells, macrophages, and neutrophils vs. other O3-exposed groups. O3 significantly increased WLL protein in the no anesthesia group and 23–24-h Iso groups, but not in the 1–2-h Iso or K/X/A groups (Fig. 2D). The F-statistics and p-values for main effects and interactions are reported in Table 1.
Effects of isoflurane (Iso) and ketamine/xylazine/atipamezole (K/X/A) on inflammatory (A–C) and vascular damage (D) markers in the lung, blood levels of serum amyloid A (SAA, E), and weight loss (F). In all panels, n = 6–20 per group. ***p < 0.001, **p < 0.01, *p < 0.05, air vs. O3. ###p < 0.001, ##p < 0.01, #p < 0.05, vs. K/X/A + O3 group. &p < 0.05 vs. No Anesthesia + O3. Group mean comparisons were carried out using Tukey’s multiple comparisons test
Effects of Iso and K/X/A Anesthesia on Ozone-Induced Systemic Inflammation and Weight Loss
We next determined whether the effects of anesthesia extended to markers of ozone-induced systemic inflammation and behavioral effects. We have previously shown that the acute-phase protein SAA is consistently increased in blood following a 3 ppm exposure to O3 and its upregulation occurs in the absence of changes in other pro-inflammatory cytokines in blood [12]. Weight loss is a measurable outcome of sickness behavior, which can be induced by O3. Anesthesia has no effect on O3-induced weight loss based on the post hoc mean comparisons of the ozone groups (Fig. 2F); however, there was a significant main effect of treatment that explained 5.172% of the total variation (Table 1). O3 significantly increased SAA levels in all groups except for mice exposed to Iso 23–24 h prior (Fig. 2E). SAA levels induced by O3 were significantly higher in mice pre-anesthetized with K/X/A vs no anesthesia or Iso.
Discussion
We found that isoflurane inhibits O3-induced pulmonary inflammation if given 1–2 h prior to exposure, and this effect diminishes by 24 h. Isoflurane induces anesthesia via potentiation of inhibitory γ-aminobutyric acid type A (GABA A) receptors and inhibition of glutamatergic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and N-methyl-d-aspartate (NMDA) receptors [13]. Isoflurane also has anti-inflammatory activities in a variety of rodent models [4], although the mechanisms are not well defined. It has been shown that activation of GABA A receptors and inhibition of NMDA receptors have anti-inflammatory effects on immune cells [14,15,16], suggesting that the anti-inflammatory activities of Iso could be mediated through direct actions on leukocytes. In contrast to Iso, K/X/A increased O3-induced inflammatory responses to O3. Anti-inflammatory/protective effects through NMDA receptor antagonism have been described for ketamine and ketamine/xylazine combinations [9]. Whereas xylazine is a α2-adrenergic receptor agonist and potentiates anesthesia, atipamezole is an antagonist and leads to rapid anesthesia reversal within about 20 min [17]. The data on pro- vs. anti-inflammatory activities of the α2 adrenergic receptor are equivocal; however, a recent study showed that atipamezole may promote or prolong inflammation through its action via a α2-independent mechanism [18]. It is also possible that anesthetics affect the amount of leukocyte trafficking to the lungs by altering the cytokine and chemokine profiles that are induced by O3. Acute exposures to O3 upregulate cytokines and chemokines such as CCL11, IL-6, G-CSF, CXCL10, and CXCL1 in a dose-dependent and cell type-specific manner [19]. Cytokines, such as TNF-α, IL-1, and IL-6, chemokines, such as CXCL1, CXCL10, and CCL7, and chemokine receptors such as CCR2 have been shown to contribute to leukocyte trafficking to the lungs in response to O3 [20,21,22,23,24,25]. Future work is needed to delineate the immunomodulatory mechanisms of Iso and K/X/A.
Our results are the first to show that isoflurane exposure prior to O3 inhibits pulmonary inflammation, whereas K/X/A exposure has an enhancing effect. These results complement other recent works that have investigated anesthesia’s effects on pulmonary inflammation in response to ozone and other pro-inflammatory agents [5, 16, 26] and effects of anesthetics on the recovery of cells from WLL [27]. Although the scope of our study is limited in that we did not define a full-time course of anesthesia’s effects, our results highlight that brief, acute anesthetic regimens can alter inflammatory responses to O3. We conclude that anesthetics are important experimental variables whose evaluation is necessary for studies requiring their use prior to exposure to O3 or other pathological stimuli.
References
Driscoll KE et al (2000) Intratracheal instillation as an exposure technique for the evaluation of respiratory tract toxicity: uses and limitations. Toxicol Sci 55:24–35. https://doi.org/10.1093/toxsci/55.1.24
Morales-Nebreda L et al (2014) Intratracheal administration of influenza virus is superior to intranasal administration as a model of acute lung injury. J Virol Methods 209:116–120. https://doi.org/10.1016/j.jviromet.2014.09.004
Lawrenz MB, Fodah RA, Gutierrez MG, Warawa J (2014) Intubation-mediated intratracheal (IMIT) instillation: a noninvasive, lung-specific delivery system. J Vis Exp. https://doi.org/10.3791/52261
Lee YM, Song BC, Yeum KJ (2015) Impact of volatile anesthetics on oxidative stress and inflammation. Biomed Res Int 2015:242709. https://doi.org/10.1155/2015/242709
Lacher SE, Johnson C, Jessop F, Holian A, Migliaccio CT (2010) Murine pulmonary inflammation model: a comparative study of anesthesia and instillation methods. Inhalation Toxicol 22:77–83. https://doi.org/10.3109/08958370902929969
Helms MN, Torres-Gonzalez E, Goodson P, Rojas M (2010) Direct tracheal instillation of solutes into mouse lung. J Vis Exp. https://doi.org/10.3791/1941
Tan S, Wang Y, Chen K, Long Z, Zou J (2017) Ketamine alleviates depressive-like behaviors via down-regulating inflammatory cytokines induced by chronic restraint stress in mice. Biol Pharm Bull 40:1260–1267. https://doi.org/10.1248/bpb.b17-00131
Chen MH et al (2018) Rapid inflammation modulation and antidepressant efficacy of a low-dose ketamine infusion in treatment-resistant depression: a randomized, double-blind control study. Psychiatry Res 269:207–211. https://doi.org/10.1016/j.psychres.2018.08.078
Erdem MK, Yurdakan G, Yilmaz-Sipahi E (2014) The effects of ketamine, midazolam and ketamine/xylazine on acute lung injury induced by alpha-naphthylthiourea in rats. Adv Clin Exp Med 23:343–351. https://doi.org/10.17219/acem/37124
Szelenyi J et al (2000) Opposite role of alpha2- and beta-adrenoceptors in the modulation of interleukin-10 production in endotoxaemic mice. NeuroReport 11:3565–3568. https://doi.org/10.1097/00001756-200011090-00032
Kierstein S et al (2008) Ozone inhalation induces exacerbation of eosinophilic airway inflammation and hyperresponsiveness in allergen-sensitized mice. Allergy 63:438–446. https://doi.org/10.1111/j.1398-9995.2007.01587.x
Erickson MA et al (2017) Serum amyloid A: an ozone-induced circulating factor with potentially important functions in the lung-brain axis. FASEB J 31:3950–3965. https://doi.org/10.1096/fj.201600857RRR
Michelson NJ, Kozai TDY (2018) Isoflurane and ketamine differentially influence spontaneous and evoked laminar electrophysiology in mouse V1. J Neurophysiol 120:2232–2245. https://doi.org/10.1152/jn.00299.2018
Reyes-Garcia MG, Hernandez-Hernandez F, Hernandez-Tellez B, Garcia-Tamayo F (2007) GABA (A) receptor subunits RNA expression in mice peritoneal macrophages modulate their IL-6/IL-12 production. J Neuroimmunol 188:64–68. https://doi.org/10.1016/j.jneuroim.2007.05.013
Bhandage AK et al (2018) GABA regulates release of inflammatory cytokines from peripheral blood mononuclear cells and CD4(+) T cells and is immunosuppressive in type 1 diabetes. EBioMedicine 30:283–294. https://doi.org/10.1016/j.ebiom.2018.03.019
Wang Y et al (2016) N-methyl-d-aspartate receptor activation mediates lung fibroblast proliferation and differentiation in hyperoxia-induced chronic lung disease in newborn rats. Respir Res 17:136. https://doi.org/10.1186/s12931-016-0453-1
Mees L et al (2018) Faster emergence behavior from ketamine/xylazine anesthesia with atipamezole versus yohimbine. PLoS ONE 13:e0199087. https://doi.org/10.1371/journal.pone.0199087
Hu J et al (2018) Dexmedetomidine prevents cognitive decline by enhancing resolution of high mobility group box 1 protein-induced inflammation through a vagomimetic action in mice. Anesthesiology 128:921–931. https://doi.org/10.1097/ALN.0000000000002038
Tovar A et al (2020) Transcriptional profiling of the murine airway response to acute ozone exposure. Toxicol Sci 173:114–130. https://doi.org/10.1093/toxsci/kfz219
Bhalla DK, Reinhart PG, Bai C, Gupta SK (2002) Amelioration of ozone-induced lung injury by anti-tumor necrosis factor-alpha. Toxicol Sci 69:400–408. https://doi.org/10.1093/toxsci/69.2.400
Cho HY, Zhang LY, Kleeberger SR (2001) Ozone-induced lung inflammation and hyperreactivity are mediated via tumor necrosis factor-alpha receptors. Am J Physiol Lung Cell Mol Physiol 280:L537-546. https://doi.org/10.1152/ajplung.2001.280.3.L537
Johnston RA, Schwartzman IN, Flynt L, Shore SA (2005) Role of interleukin-6 in murine airway responses to ozone. Am J Physiol Lung Cell Mol Physiol 288:L390-397. https://doi.org/10.1152/ajplung.00007.2004
Park JW et al (2004) Interleukin-1 receptor antagonist attenuates airway hyperresponsiveness following exposure to ozone. Am J Respir Cell Mol Biol 30:830–836. https://doi.org/10.1165/rcmb.2003-0373OC
Michalec L et al (2002) CCL7 and CXCL10 orchestrate oxidative stress-induced neutrophilic lung inflammation. J Immunol 168:846–852. https://doi.org/10.4049/jimmunol.168.2.846
Francis M et al (2017) Editor’s highlight: CCR2 regulates inflammatory cell accumulation in the lung and tissue injury following ozone exposure. Toxicol Sci 155:474–484. https://doi.org/10.1093/toxsci/kfw226
Yuki K et al (2021) Anesthetics isoflurane and sevoflurane attenuate flagellin-mediated inflammation in the lung. Biochem Biophys Res Commun 557:254–260. https://doi.org/10.1016/j.bbrc.2021.04.045
Tighe RM, Birukova A, Yaeger MJ, Reece SW, Gowdy KM (2018) Euthanasia- and lavage-mediated effects on bronchoalveolar measures of lung injury and inflammation. Am J Respir Cell Mol Biol 59:257–266. https://doi.org/10.1165/rcmb.2017-0357OC
Funding
This study was funded by the National Institutes of Health (R21ES029657, MAE) and the Veterans Administration (MAE).
Author information
Authors and Affiliations
Contributions
All authors contributed to the collection and analysis of data, editing of manuscript drafts, and approved the final version of the manuscript. MAE, JAT, KKB, and MLW contributed to the study conception and design and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The use of mice on this study was approved by the VA Puget Sound Healthcare System IACUC, protocol 0924. Human subjects were not used on this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wilson, M.L., Thysell, J.A., Baumann, K.K. et al. Effects of Anesthesia on Ozone-Induced Lung and Systemic Inflammation. Lung 200, 269–275 (2022). https://doi.org/10.1007/s00408-022-00514-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-022-00514-5