Abstract
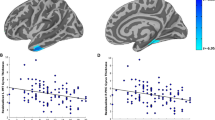
The concept of acute stress disorder (ASD) was introduced as a diagnostic entity to improve the identification of traumatized people who are likely to develop posttraumatic stress disorder (PTSD). Neuroanatomical models suggest that changes in the prefrontal cortex, amygdala, and hippocampus play a role in the development of PTSD. Using voxel-based morphometry, this study aimed to investigate the predictive power of gray matter volume (GMV) alterations for developing PTSD. The GMVs of ASD patients (n = 21) were compared to those of PTSD patients (n = 17) and healthy controls (n = 18) in whole-brain and region-of-interest analyses. The GMV alterations seen in ASD patients shortly after the traumatic event (T1) were also correlated with PTSD symptom severity and symptom clusters 4 weeks later (T2). Compared with healthy controls, the ASD patients had significantly reduced GMV in the left visual cortex shortly after the traumatic event (T1) and in the left occipital and prefrontal regions 4 weeks later (T2); no significant differences in GMV were seen between the ASD and PTSD patients. Furthermore, a significant negative association was found between the GMV reduction in the left lateral temporal regions seen after the traumatic event (T1) and PTSD hyperarousal symptoms 4 weeks later (T2). Neither amygdala nor hippocampus alterations were predictive for the development of PTSD. These data suggest that gray matter deficiencies in the left hemispheric occipital and temporal regions in ASD patients may predict a liability for developing PTSD.



Similar content being viewed by others
References
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC. https://doi.org/10.1176/appi.books.9780890423349
Bryant RA (2013) An update of acute stress disorder. PTSD Res Q 24:1–7
Spiegel D, Koopman C, Cardeña E, Classen C (1996) Dissociative symptoms in the diagnosis of acute stress disorder. In: Ray WJ (ed) Michelson LK. Plenum, New York, pp 367–380
Bryant RA (2018) The current evidence for acute stress disorder. Curr Psychiatry Rep. https://doi.org/10.1007/s11920-018-0976-x
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington, DC
Kleim B, Ehlers A, Glucksman E (2007) Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychol Med 37(10):1457–1467. https://doi.org/10.1017/S0033291707001006
Bryant RA (2006) Acute stress disorder. Psychiatry 5:238–239. https://doi.org/10.1053/j.mppsy.2006.04.003
Veazey C, Blanchard EB (2005) Early indicators and interventions for traumatic stress disorders secondary to motor vehicle accidents. In: Hennessy D, Wiesenthal D (eds) Nova Science. Hauppauge, NY, pp 199–214
Bryant RA (2011) Acute stress disorder as a predictor of posttraumatic stress disorder: a systematic review. J Clin Psychiatry 72(2):233–239. https://doi.org/10.4088/JCP.09r05072blu
Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC (2012) The capacity of acute stress disorder to predict posttraumatic psychiatric disorders. J Psychiatr Res 46(2):168–173. https://doi.org/10.1016/j.jpsychires.2011.10.007
Bryant RA (2003) Acute stress reactions: can biological responses predict posttraumatic stress disorder? CNS Spectr 8(9):668–674
Ahmed-Leitao F, Spies G, van den Heuvel L, Seedat S (2016) Hippocampal and amygdala volumes in adults with posttraumatic stress disorder secondary to childhood abuse or maltreatment: a systematic review. Psychiatry Res Neuroimaging 256:33–43. https://doi.org/10.1016/j.pscychresns.2016.09.008
Bromis K, Calem M, Reinders AATS, Williams SCR, Kempton MJ (2018) Meta-analysis of 89 structural MRI studies in posttraumatic stress disorder and comparison with major depressive disorder. Am J Psychiatry. https://doi.org/10.1176/appi.ajp.2018.17111199
O’Doherty DCM, Chitty KM, Saddiqui S, Bennett MR, Lagopoulos J (2015) A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Res Neuroimaging 232(1):1–33. https://doi.org/10.1016/j.pscychresns.2015.01.002
Kühn S, Gallinat J (2013) Gray matter correlates of posttraumatic stress disorder: a quantitative meta-analysis. Biol Psychiat 73(1):70–74. https://doi.org/10.1016/j.biopsych.2012.06.029
Woon FL, Sood S, Hedges DW (2010) Hippocampal volume deficits associated with exposure to psychological trauma and posttraumatic stress disorder in adults: a meta-analysis. Progress Neuropsychopharmacol Biol Psychiatry 34(7):1181–1188. https://doi.org/10.1016/j.pnpbp.2010.06.016
Karl A, Malta LS, Maercker A (2006) Meta-analytic review of event-related potential studies in post-traumatic stress disorder. Biol Psychol 71(2):123–147. https://doi.org/10.1016/j.biopsycho.2005.03.004
Kitayama N, Vaccarino V, Kutner M, Weiss P, Bremner JD (2005) Magnetic resonance imaging (MRI) measurement of hippocampal volume in posttraumatic stress disorder: a meta-analysis. J Affect Disord 88:79–86. https://doi.org/10.1016/j.jad.2005.05.014
Rogers MA, Yamasue H, Abe O, Yamada H, Ohtani T, Iwanami A, Aoki S, Kato N, Kasai K (2009) Smaller amygdala volume and reduced anterior cingulate gray matter density associated with history of post-traumatic stress disorder. Psychiatry Res Neuroimaging 174(3):210–216. https://doi.org/10.1016/j.pscychresns.2009.06.001
Liu Y, Li Y-J, Luo E-P, Lu H-B, Yin H (2012) Cortical thinning in patients with recent onset post-traumatic stress disorder after a single prolonged trauma exposure. PLoS One 7(6):e39025. https://doi.org/10.1371/journal.pone.0039025
Ahmed F, Ras J, Seedat S (2012) Volumetric structural magnetic resonance imaging findings in pediatric posttraumatic stress disorder and obsessive compulsive disorder: a systematic review. Front Psychol 3:568. https://doi.org/10.3389/fpsyg.2012.00568
Im JJ, Kim B, Hwang J, Kim JE, Kim JY, Rhie SJ, Namgung E, Kang I, Moon S, Lyoo IK, Park C-H, Yoon S (2017) Diagnostic potential of multimodal neuroimaging in posttraumatic stress disorder. PLoS One 12(5):e0177847. https://doi.org/10.1371/journal.pone.0177847
Chen Y, Fu K, Feng C, Tang L, Zhang J, Huan Y, Cui J, Mu Y, Qi S, Xiong L, Ma C, Wang H, Tan Q, Yin H (2012) Different regional gray matter loss in recent onset PTSD and non PTSD after a single prolonged trauma exposure. PLoS One 7(11):e48298. https://doi.org/10.1371/journal.pone.0048298
Kroes MCW, Rugg MD, Whalley MG, Brewin CR (2011) Structural brain abnormalities common to posttraumatic stress disorder and depression. J Psychiatry Neurosci 36(4):256–265. https://doi.org/10.1503/jpn.100077
Tavanti M, Battaglini M, Borgogni F, Bossini L, Calossi S, Marino D, Vatti G, Pieraccini F, Federico A, Castrogiovanni P, De Stefano N (2012) Evidence of diffuse damage in frontal and occipital cortex in the brain of patients with post-traumatic stress disorder. Neurol Sci 33:59–68. https://doi.org/10.1007/s10072-011-0659-4
Cheng B, Huang X, Li S, Hu X, Luo Y, Wang X, Yang X, Qiu C, Yang Y, Zhang W, Bi F, Roberts N, Gong Q (2015) Gray matter alterations in post-traumatic stress disorder, obsessive–compulsive disorder, and social anxiety disorder. Front Behav Neurosci 9:219. https://doi.org/10.3389/fnbeh.2015.00219
Li H-J, Sun J-Z, Zhang Q-L, Wei D-T, Li W-F, Jackson T, Hitchman G, Qiu J (2014) Neuroanatomical differences between men and women in help-seeking coping strategy. Sci Rep 4:5700. https://doi.org/10.1038/srep05700
Morey RA, Haswell CC, Hooper SR, De Bellis MD (2016) Amygdala, hippocampus, and ventral medial prefrontal cortex volumes differ in maltreated youth with and without chronic posttraumatic stress disorder. Neuropsychopharmacology 41(3):791–801. https://doi.org/10.1038/npp.2015.205
Wrocklage KM, Averill LA, Scott JC, Averill CL, Schweinsburg B, Trejo M, Roy A, Weisser V, Kelly C, Martini B, Harpaz-Rotem I, Southwick SM, Krystal JH, Abdallah CG, Haven W, States U (2017) Cortical thickness reduction in combat exposed U.S. veterans with and without PTSD. Eur Neuropsychopharmacol 27(5):515–525. https://doi.org/10.1016/j.euroneuro.2017.02.010
Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, Domschke K, Hohoff C, Ohrmann P, Bauer J, Lindner C, Postert C, Konrad C, Arolt V, Heindel W, Suslow T (2012) Limbic scars: long-term consequences of childhood magnetic resonance imaging. Biol Psychiatry 71(4):286–293. https://doi.org/10.1016/j.biopsych.2011.10.021
Burgmer M, Rehbein MA, Wrenger M, Kandil J, Heuft G, Steinberg C, Pfleiderer B, Junghöfer M (2013) Early affective processing in patients with acute posttraumatic stress disorder: magnetoencephalographic correlates. PLoS One 8(8):e71289. https://doi.org/10.1371/journal.pone.0071289
Sekiguchi A, Sugiura M, Taki Y, Kotozaki Y, Nouchi R, Takeuchi H, Araki T, Hanawa S, Nakagawa S, Miyauchi CM, Sakuma A, Kawashima R (2013) Brain structural changes as vulnerability factors and acquired signs of post-earthquake stress. Mol Psychiatry 18(5):618–623. https://doi.org/10.1038/mp.2012.51
Yamasue H, Kasai K, Iwanami A, Ohtani T, Yamada H, Abe O, Kuroki N, Fukuda R, Tochigi M, Furukawa S, Sadamatsu M, Sasaki T, Aoki S, Ohtomo K, Asukai N, Kato N (2003) Voxel-based analysis of MRI reveals anterior cingulate gray-matter volume reduction in posttraumatic stress disorder due to terrorism. Proc Natl Acad Sci USA 100(15):9039–9043. https://doi.org/10.1073/pnas.1530467100
Rocha-Rego V, Pereira MG, Oliveira L, Mendlowicz MV, Fiszman A, Marques-Portella C, Berger W, Chu C, Joffily M, Moll J, Mari JJ, Figueira I, Volchan E (2012) Decreased premotor cortex volume in victims of urban violence with posttraumatic stress disorder. PLoS One 7(8):e42560. https://doi.org/10.1371/journal.pone.0042560
Bryant RA, Felmingham KL, Kemp A, Das P, Hughes G, Peduto A, Williams L (2008) Amygdala and ventral anterior cingulate activation predicts treatment response to cognitive behaviour therapy for post-traumatic stress disorder. Psychol Med 38(4):555–561. https://doi.org/10.1017/S0033291707002231
Jatzko A, Vogler C, Demirakca T, Ruf M, Malchow B, Falkai P, Braus DF, Ende G, Schmitt A (2013) Pattern and volume of the anterior cingulate cortex in chronic posttraumatic stress disorder (PTSD). Eur Arch Psychiatry Clin Neurosci 263:585–592. https://doi.org/10.1007/s00406-013-0408-1
Dickie EW, Brunet A, Akerib V, Armony JL (2013) Anterior cingulate cortical thickness is a stable predictor of recovery from post-traumatic stress disorder. Psychol Med 43(3):645–653. https://doi.org/10.1017/S0033291712001328
Corbo V, Clément M-H, Armony JL, Pruessner JC, Brunet A (2005) Size versus shape differences: contrasting voxel-based and volumetric analyses of the anterior cingulate cortex in individuals with acute posttraumatic stress disorder. Biol Psychiatry 58(2):119–124. https://doi.org/10.1016/j.biopsych.2005.02.032
Zhang Q, Zhuo C, Lang X, Li H, Qin W, Yu C (2014) Structural impairments of hippocampus in coal mine gas explosion-related posttraumatic stress disorder. PLoS One 9(7):e102042. https://doi.org/10.1371/journal.pone.0102042
Meng Y, Qiu C, Zhu H, Lama S, Lui S, Gong Q, Zhang W (2014) Anatomical deficits in adult posttraumatic stress disorder: a meta-analysis of voxel-based morphometry studies. Behav Brain Res 270:307–315. https://doi.org/10.1016/j.bbr.2014.05.021
Golkar A, Lonsdorf TB, Olsson A, Lindstrom KM, Berrebi J, Fransson P, Schalling M, Ingvar M, Öhman A (2012) Distinct contributions of the dorsolateral prefrontal and orbitofrontal cortex during emotion regulation. PLoS One 7(11):e48107. https://doi.org/10.1371/journal.pone.0048107
Banks SJ, Eddy KT, Angstadt M, Nathan PJ, Phan KL (2007) Amygdala-frontal connectivity during emotion regulation. Soc Cognit Affect Neurosci 2(4):303–312. https://doi.org/10.1093/scan/nsm029
Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN (2008) Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron 59:1037–1050. https://doi.org/10.1016/j.neuron.2008.09.006
Kanske P, Heissler J, Schönfelder S, Bongers A, Wessa M (2011) How to regulate emotion? Neural networks for reappraisal and distraction. Cereb Cortex 21:1379–1388. https://doi.org/10.1093/cercor/bhq216
Lanius RA, Williamson PC, Hopper J, Densmore M, Boksman K, Gupta MA, Neufeld RWJ, Gati JS, Menon RS (2003) Recall of emotional states in posttraumatic stress disorder: an fMRI investigation. Biol Psychiatry 53(3):204–210. https://doi.org/10.1016/S0006-3223(02)01466-X
Scult MA, Knodt AR, Swartz JR, Brigidi BD, Hariri AR (2017) Thinking and feeling: individual differences in habitual emotion regulation and stress-related mood are associated with prefrontal executive control. Clin Psychol Sci 5(1):150–157. https://doi.org/10.1177/2167702616654688
Zander T, Horr NK, Bolte A, Volz KG (2016) Intuitive decision making as a gradual process: investigating semantic intuition-based and priming-based decisions with fMRI. Brain Behav 6(1):e00420. https://doi.org/10.1002/brb3.420
Arnsten AFT, Raskind MA, Taylor FB, Connor DF (2015) The effects of stress exposure on prefrontal cortex: translating basic research into successful treatments for post-traumatic stress disorder. Neurobiol Stress 1:89–99. https://doi.org/10.1016/j.ynstr.2014.10.002
Milad MR, Wright CI, Orr SP, Pitman RK, Quirk GJ, Rauch SL (2007) Recall of fear extinction in humans activates the ventromedial prefrontal cortex and hippocampus in concert. Biol Psychiatry 62(5):446–454. https://doi.org/10.1016/j.biopsych.2006.10.011
Shin LM, Rauch SL, Pitman RK (2006) Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann N Y Acad Sci 1071:67–79. https://doi.org/10.1196/annals.1364.007
Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9(1):97–113. https://doi.org/10.1016/0028-3932(71)90067-4
Bryant RA, Harvey AG, Dang ST, Sackville T (1998) Assessing acute stress disorder: psychometric properties of a structured clinical interview. Psychol Assess 10(3):215–220. https://doi.org/10.1037/1040-3590.10.3.215
Cwik JC, Sartory G, Schürholt B, Knuppertz H, Seitz RJ (2014) Posterior midline activation during symptom provocation in acute stress disorder: an fMRI study. Front Psychiatry 5:49. https://doi.org/10.3389/fpsyt.2014.00049
Cwik JC, Sartory G, Nuyken M, Schürholt B, Seitz RJ (2017) Posterior and prefrontal contributions to the development of posttraumatic stress disorder symptom severity: an fMRI study of symptom provocation in acute stress disorder. Eur Arch Psychiatry Clin Neurosci 267(6):495–505. https://doi.org/10.1007/s00406-016-0713-6
Elsesser K (1999) Interview zur Akuten Belastungsstörung; German version of Acute Stress Disorder Interview (ASDI). Universität Wuppertal, Unveröffentlicht
Blake DD (1994) Rationale and development of the Clinician-Administered PTSD Scales. PTSD Res Q 5(2):1–8
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM (1995) The development of a Clinician-Administered PTSD Scale. J Trauma Stress 8(1):75–90. https://doi.org/10.1007/BF02105408
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM (1998) Clinician-administered PTSD scale for DSM-IV. National Center for Posttraumatic Stress Disorder-Behavioral Science Division, Boston
Schnyder U, Moergeli H (2002) German version of clinician-administered PTSD Scale. J Trauma Stress 15(6):487–492. https://doi.org/10.1023/A:1020922023090
Weathers FW, Ruscio AM, Keane TM (1999) Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychol Assess 11(2):124–133. https://doi.org/10.1037//1040-3590.11.2.124
Margraf J (1994) Diagnostisches Kurz-Interview psychischer Störungen (Mini-DIPS). Beltz, Weinheim
Margraf J, Cwik JC (2017) Mini-DIPS Open Access: Diagnostisches Kurzinterview bei psychischen Störungen, 2nd edn. Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum, Bochum
Margraf J, Cwik JC, Pflug V, Schneider S (2017) Strukturierte klinische Interviews zur Erfassung psychischer Störungen über die Lebensspanne: gütekriterien und Weiterentwicklungen der DIPS-Verfahren. Zeitschrift für Klinische Psychologie und Psychotherapie 46(3):176–186. https://doi.org/10.1026/1616-3443/a000430
Margraf J, Cwik JC, Suppiger A, Schneider S (2017) Diagnostisches Interview bei Psychischen Störungen - Open Access (DIPS-OA), 5th edn. Forschungs- und Behandlungszentrum für psychische Gesundheit, Ruhr-Universität Bochum, Bochum. https://doi.org/10.13154/rub.100.89
In-Albon T, Suppiger A, Schlup B, Wendler S, Margraf J, Schneider S (2008) Validität des Diagnostischen Interviews bei Psychischen Störungen (DIPS für DSM-IV-TR). Zeitschrift für Klinische Psychologie und Psychotherapie 37(1):33–42. https://doi.org/10.1026/1616-3443.37.1.33
Rajapakse JC, Giedd JN, Rapoport JL (1997) Statistical approach to segmentation of single-channel cerebral MR images. IEEE Trans Med Imaging 16(2):176–186
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, Mazoyer B, Joliot M (2002) Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI signle-subject brain. NeuroImage 15:273–289
Borgwardt S, Radua J, Mechelli A, Fusar-Poli P (2012) Why are psychiatric imaging methods clinically unreliable? Conclusions and practical guidelines for authors, editors and reviewers. Behav Brain Funct 8:46. https://doi.org/10.1186/1744-9081-8-46
Braun AR, Guillemin A, Hosey L, Varga M (2001) The neural organization of discourse: an H215O-PET study of narrative production in English and American sign language. Brain 124(10):2028–2044. https://doi.org/10.1093/brain/124.10.2028
Kirschen MP, Chen SHA, Desmond JE (2010) Modality specific cerebro-cerebellar activations in verbal working memory: an fMRI study. Behav Neurol 23(1–2):51–63. https://doi.org/10.3233/BEN-2010-0266
Crottaz-Herbette S, Anagnoson RT, Menon V (2004) Modality effects in verbal working memory: differential prefrontal and parietal responses to auditory and visual stimuli. NeuroImage 21(1):340–351. https://doi.org/10.1016/j.neuroimage.2003.09.019
Goldin PR, McRae K, Ramel W, Gross JJ (2008) The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiat 63(6):577–586. https://doi.org/10.1016/j.biopsych.2007.05.031
Bourne C, Mackay CE, Holmes EA (2013) The neural basis of flashback formation: the impact of viewing trauma. Psychol Med 43(7):1521–1532. https://doi.org/10.1017/S0033291712002358
Lee TMC, Lee TMY, Raine A, Chan CCH (2010) Lying about the valence of affective pictures: an fMRI study. PLoS One 5(8):e12291–e12291. https://doi.org/10.1371/journal.pone.0012291
Sussman D, Pang EW, Jetly R, Dunkley BT, Taylor MJ (2016) Neuroanatomical features in soldiers with post-traumatic stress disorder. BMC Neurosci 17:13. https://doi.org/10.1186/s12868-016-0247-x
Tomoda A, Navalta CP, Polcari A, Sadato N, Teicher MH (2009) Childhood sexual abuse is associated with reduced gray matter volume in visual cortex of young women. Biol Psychiatry 66(7):642–648. https://doi.org/10.1016/j.biopsych.2009.04.021
Nardo D, Högberg G, Lanius RA, Jacobsson H, Jonsson C, Hällström T, Pagani M (2013) Gray matter volume alterations related to trait dissociation in PTSD and traumatized controls. Acta Psychiatry Scand 128(3):222–233. https://doi.org/10.1111/acps.12026
Lanius RA, Bluhm R, Lanius U, Pain C (2006) A review of neuroimaging studies in PTSD: heterogeneity of response to symptom provocation. J Psychiatry Res 40(8):709–729. https://doi.org/10.1016/j.jpsychires.2005.07.007
Brewin CR, Dalgleish T, Joseph S (1996) A dual representation theory of posttraumatic stress disorder. Psychol Rev 103(4):670–686. https://doi.org/10.1037/0033-295X.103.4.670
Brewin CR (2001) A cognitive neuroscience account of posttraumatic stress disorder and its treatment. Behav Res Ther 39(4):373–393
Brewin CR, Gregory JD, Lipton M, Burgess N (2010) Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychol Rev 117(1):210–232. https://doi.org/10.1037/a0018113
O’Doherty DCM, Tickell A, Ryder W, Chan C, Hermens DF, Bennett MR, Lagopoulos J (2017) Neuroimaging frontal and subcortical grey matter reductions in PTSD. Psychiatry Res Neuroimag 266:1–9. https://doi.org/10.1016/j.pscychresns.2017.05.008
Kasai K, Yamasue H, Gilbertson MW, Shenton ME, Rauch SL, Pitman RK (2008) Evidence for acquired pregenual anterior cingulate gray matter loss from a twin study of combat-related posttraumatic stress disorder. Biol Psychiat 63(6):550–556. https://doi.org/10.1016/j.biopsych.2007.06.022
Eckart C, Stoppel C, Kaufmann J, Tempelmann C, Hinrichs H, Elbert T, Heinze H-J, Kolassa I-T (2011) Structural alterations in lateral prefrontal, parietal and posterior midline regions of men with chronic posttraumatic stress disorder. Journal of Psychiatry and Neuroscience Neuroscience 36(3):176–186. https://doi.org/10.1503/jpn.100010
Tomoda A, Suzuki H, Rabi K, Sheu Y-S, Polcari A, Teicher MH (2010) Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. NeuroImage 47(Suppl 2):T66–T71. https://doi.org/10.1016/j.neuroimage.2009.03.005
Zhang J, Tan Q, Yin H, Zhang X, Huan Y, Tang L, Wang H, Xu J, Li L (2011) Decreased gray matter volume in the left hippocampus and bilateral calcarine cortex in coal mine flood disaster survivors with recent onset PTSD. Psychiatry Res Neuroimag 192(2):84–90. https://doi.org/10.1016/j.pscychresns.2010.09.001
Cremers HR, Wager TD, Yarkoni T (2017) The relation between statistical power and inference in fMRI. PLoS One 12(11):e0184923. https://doi.org/10.1371/journal.pone.0184923
Szabó C, Kelemen O, Levy-Gigi E, Kéri S (2015) Acute response to psychological trauma and subsequent recovery: no changes in brain structure. Psychiatry Res Neuroimag 231(3):269–272. https://doi.org/10.1016/j.pscychresns.2015.01.005
Meng L, Jiang J, Jin C, Liu J, Zhao Y, Wang W, Li K, Gong Q (2016) Trauma-specific grey matter alterations in PTSD. Sci Rep 6:33748. https://doi.org/10.1038/srep33748
Kroes MCW, Whalley MG, Rugg MD, Brewin CR (2011) Association between flashbacks and structural brain abnormalities in posttraumatic stress disorder. Eur Psychiatry 26(8):525–531. https://doi.org/10.1016/j.eurpsy.2011.03.002
Li L, Wu M, Liao Y, Ouyang L, Du M, Lei D, Chen L, Yao L, Huang X, Gong Q (2014) Grey matter reduction associated with posttraumatic stress disorder and traumatic stress. Neurosci Biobehav Rev 43(37):163–172. https://doi.org/10.1016/j.neubiorev.2014.04.003
Qin P, Northoff G (2011) How is our self related to midline regions and the default-mode network? NeuroImage 57(3):1221–1233. https://doi.org/10.1016/j.neuroimage.2011.05.028
Abu-Akel A, Shamay-Tsoory S (2011) Neuroanatomical and neurochemical bases of theory of mind. Neuropsychologia 49(11):2971–2984. https://doi.org/10.1016/j.neuropsychologia.2011.07.012
Feng S, Ye X, Mao L, Yue X (2014) The activation of theory of mind network differentiates between point-to-self and point-to-other verbal jokes: an fMRI study. Neurosci Lett 564:32–36. https://doi.org/10.1016/j.neulet.2014.01.059
Schurz M, Radua J, Aichhorn M, Richlan F, Perner J (2014) Fractionating theory of mind: a meta-analysis of functional brain imaging studies. Neurosci Biobehav Rev 42:9–34. https://doi.org/10.1016/j.neubiorev.2014.01.009
Calabro FJ, Vaina LM (2012) Interaction of cortical networks mediating object motion detection by moving observers. Exp Brain Res 221(2):177–189. https://doi.org/10.1007/s00221-012-3159-8
Gilaie-Dotan S, Bentin S, Harel M, Rees G, Saygin AP (2011) Normal form from biological motion despite impaired ventral stream function. Neuropsychologia 49(5):1033–1043. https://doi.org/10.1016/j.neuropsychologia.2011.01.009
Zachariou V, Klatzky R, Behrmann M (2014) Ventral and dorsal visual stream contributions to the perception of object shape and object location. J Cognit Neurosci 26(1):189–209. https://doi.org/10.1162/jocn_a_00475
Gilaie-Dotan S, Kanai R, Bahrami B, Rees G, Saygin AP (2013) Neuroanatomical correlates of biological motion detection. Neuropsychologia 51(3):457–463. https://doi.org/10.1016/j.neuropsychologia.2012.11.027
Reeder RR, Perini F, Peelen MV (2015) Preparatory activity in posterior temporal cortex causally contributes to object detection in scenes. J Cognit Neurosci 27(11):2117–2125. https://doi.org/10.1162/jocn_a_00845
Jatzko A, Rothenhöfer S, Schmitt A, Gaser C, Demirakca T, Weber-Fahr W, Wessa M, Magnotta V, Braus DF (2006) Hippocampal volume in chronic posttraumatic stress disorder (PTSD): MRI study using two different evaluation methods. J Affect Disord 94(1–3):121–126. https://doi.org/10.1016/j.jad.2006.03.010
Wignall EL, Dickson JM, Vaughan P, Farrow TFD, Wilkinson ID, Hunter MD, Woodruff PWR (2004) Smaller hippocampal volume in patients with recent-onset posttraumatic stress disorder. Biol Psychiat 56:832–836. https://doi.org/10.1016/j.biopsych.2004.09.015
Gurvits TV, Shenton ME, Hokama H, Ohta H, Lasko NB, Gilbertson MW, Orr SP, Kikinis R, Jolesz FA, McCarley RW, Pitman RK (1996) Magnetic resonance imaging study of hippocampal volume in chronic, combat-related posttraumatic stress disorder. Biol Psychiat 40(11):1091–1099. https://doi.org/10.1016/S0006-3223(96)00229-6
Letizia B, Maricla T, Sara C, Alessia L, Riccardo PN, Rosita G, Gianpaolo V, Fulvio P, Paolo C (2008) Magnetic resonance imaging volumes of the hippocampus in drug-naive patients with post-traumatic stress disorder without comorbidity conditions. J Psychiatr Res 42(9):752–762. https://doi.org/10.1016/j.jpsychires.2007.08.004
Kanazawa Y, Nakamura K, Ishii T, Aso T, Yamazaki H, Omori K (2017) Phonological memory in sign language relies on the visuomotor neural system outside the left hemisphere language network. PLoS One 12(9):e0177599–e0177599. https://doi.org/10.1371/journal.pone.0177599
Labudda K, Mertens M, Janszky J, Bien CG, Woermann FG (2012) Atypical language lateralisation associated with right fronto-temporal grey matter increases—a combined fMRI and VBM study in left-sided mesial temporal lobe epilepsy patients. NeuroImage 59(1):728–737. https://doi.org/10.1016/j.neuroimage.2011.07.053
Dole M, Meunier F, Hoen M (2013) Gray and white matter distribution in dyslexia: a VBM study of superior temporal gyrus asymmetry. PLoS One 8(10):1–14. https://doi.org/10.1371/journal.pone.0076823
Haagsma JA, Polinder S, Olff M, Toet H, Bonsel GJ, van Beeck EF (2012) Posttraumatic stress symptoms and health-related quality of life: a two year follow up study of injury treated at the emergency department. BMC Psychiatry 12:1. https://doi.org/10.1186/1471-244X-12-1
Baldaçara L, Jackowski AP, Schoedl A, Pupo M, Andreoli SB, Mello MF, Lacerda ALT, Mari JJ, Bressan RA (2011) Reduced cerebellar left hemisphere and vermal volume in adults with PTSD from a community sample. J Psychiatry Res 45(12):1627–1633. https://doi.org/10.1016/j.jpsychires.2011.07.013
Brewin CR, Holmes EA (2003) Psychological theories of posttraumatic stress disorder. Clin Psychol Rev 23(3):339–376. https://doi.org/10.1016/S0272-7358(03)00033-3
Brewin CR, Burgess N (2014) Contextualisation in the revised dual representation theory of PTSD: a response to Pearson and colleagues. J Behav Ther Exp Psychiatry 45(1):217–219. https://doi.org/10.1016/j.jbtep.2013.07.011
David SP, Ware JJ, Chu IM, Loftus PD, Fusar-Poli P, Radua J, Munafò MR, Ioannidis JPA (2013) Potential reporting bias in fMRI studies of the brain. PLoS One 8(7):e70104. https://doi.org/10.1371/journal.pone.0070104
Kuester A, Köhler K, Ehring T, Knaevelsrud C, Kober L, Krüger-Gottschalk A, Schäfer I, Schellong J, Wesemann U, Rau H (2017) Comparison of DSM-5 and proposed ICD-11 criteria for PTSD with DSM-IV and ICD-10: changes in PTSD prevalence in military. Eur J Psychotraumatol 8(1):1386988. https://doi.org/10.1080/20008198.2017.1386988
Gong Q, Li L, Tognin S, Wu Q, Pettersson-Yeo W, Lui S, Huang X, Marquand AF, Mechelli A (2014) Using structural neuroanatomy to identify trauma survivors with and without post-traumatic stress disorder at the individual level. Psychol Med 44(1):195–203. https://doi.org/10.1017/S0033291713000561
Acknowledgments
All authors have agreed to authorship. There has been no prior publication. The authors would like to thank Jan Kirsten for editing the manuscript and Erika Rädisch (Institute of Diagnostic and Interventional Radiology) for assistance in acquiring the MRI scans. Furthermore, the authors would like to thank Benjamin Schürholt and Sascha Brunheim for their technical support, and Judith Holz and Helge Knuppertz for their support in the data collection. The authors would like to dedicate this study with the deepest respect and in grateful remembrance of Prof. Dr. Gudrun Sartory.
Funding
The study was supported by the Deutsche Forschungsgemeinschaft (DFG) (SA 735/18-1; SE 494/7-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report to have no biomedical or financial interest or potential conflict of interest.
Ethical standards
The Ethics Committees of the Universities of Wuppertal and Düsseldorf approved the study. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Rights and permissions
About this article
Cite this article
Cwik, J.C., Vahle, N., Woud, M.L. et al. Reduced gray matter volume in the left prefrontal, occipital, and temporal regions as predictors for posttraumatic stress disorder: a voxel-based morphometric study. Eur Arch Psychiatry Clin Neurosci 270, 577–588 (2020). https://doi.org/10.1007/s00406-019-01011-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01011-2