Abstract
Purpose
The optimal pain management concept in children after tonsil surgery is controversial. Ibuprofen on an “around-the-clock” basis has been suggested to control postoperative pain sufficiently. Therefore, we established a standard scheme with weight-adapted recommended maximum ibuprofen dose. A reliable assessment of pain intensity can be performed with the Children’s and Infants’ Postoperative Pain Scale (CHIPPS) in children < 5 years, or with the Faces Pain Scale-Revised (FPS-R) in children aged ≥ 5 years. The Parents’ Postoperative Pain Measure (PPPM-D) may be a useful tool for both age groups. We hypothesized that not more than 30% of the children would need an opioid rescue medication during their in-hospital stay and analyzed the consistency of the PPPM-D with other pain scales.
Methods
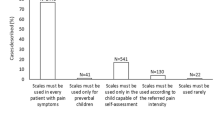
We included 158 in-patients aged 2–12 years. Ibuprofen was orally administered every 8 h. Three times daily, pain scores were assessed by CHIPPS or FPS-R, respectively. The PPPM-D was used in all children. Exceeding the cut-off value in one of the tools was regarded as relevant pain.
Results
A rescue medication was needed in 82.1% of children after tonsillectomy and 51.3% of children after tonsillotomy (P < 0.001). The cut-off value for relevant pain was mostly exceeded in the PPPM-D, but its overall concordance to the reference scales was low.
Conclusion
High-dose ibuprofen “around-the-clock” is insufficient to control pain in children after tonsil surgery. Research is needed to find an optimal schema for management and assessment of postoperative pain.



Similar content being viewed by others
References
Sutters KA, Isaacson G (2014) Posttonsillectomy pain in children. Am J Nurs 114:36–42
Windfuhr JP, Toepfner N, Steffen G, Waldfahrer F, Berner R (2016) Clinical practice guideline: tonsillitis II. Surg Manag Eur Arch Otorhinolarngol 273:989–1009
Statistisches Bundesamt [German Federal Statistical Office] (2017) DRG-Statistik. Wiesbaden
Constant I, Ayari Khalfallah S, Brunaud A et al (2014) How to replace codeine after tonsillectomy in children under 12 years of age? Guidelines of the French OtoRhinoLaryngology OtoRhinoLaryngology—Head and Neck Surgery Society (SFORL). Eur Ann Otorhinolaryngol Head Neck Dis 131:233–238
Ericsson E, Brattwall M, Lundeberg S (2015) Swedish guidelines for the treatment of pain in tonsil surgery in pediatric patients up to 18 years. Int J Pediatr Otorhinolaryngol 9:443–450
Mitchell RB, Archer SM, Ishman SL et al (2019) Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg 160:S1–S42
Hobson A, Wiffen PJ, Conlon JA (2015) As required versus fixed schedule analgesic administration for postoperative pain in children. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858
Gude P, Rieckert C, Bissantz N et al (2018) Need of analgetics in children aged 2–12 years after tonsil surgery. Laryngorhinootologie 97:465–473
Rodieux A, Piguet V, Desmeules J, Samer CF (2019) Safety issues of pharmacological acute pain treatment in children. Clin Pharmacol Ther 105:1130–1138
Zahn PK, Sabatowski R, Schug SA, Stamer UM, Pogatzki-Zahn EM (2010) Paracetamol for perioperative analgesia. Old substance—new insights. Anästhesist 59:940–952
Lönnqvist PA, Morton NS (2005) Postoperative analgesia in infants and children. Br J Anaesth 95:59–68
Rakow H, Finke W, Mutze K, Reich A, Reinhold P, Strauß JM (2007) Handlungsempfehlung zur perioperativen Schmerztherapie bei Kindern. Anästh Intensivmed 48:99–103
Bringuier S, Picot MC, Dadure C et al (2009) A prospective comparision of post-surgical behavioral pain scales in preschoolers highlighting the risk of false evaluations. Pain 145:60–68
Beyer JE, McGrath PJ, Berde CB (2009) Discordance between self-report and behavioral pain measures in children aged 3–7 years after surgery. J Pain Symptom Manag 5:350–356
Twycross A, Voepel-Lewis T, Vincent C, Franck L, von Baeyer CL (2015) A debate on the proposition that self-report is the gold standard in assessment of pediatric pain intensity. Clin J Pain 31:707–712
Stanford EA, Chambers C, Craig KD (2006) The role of developmental factors in predicting young children’s use of a self-report scale for pain. Pain 120:16–23
Chambers CT, Finley GA, McGrath PJ, Walsh TM (2003) The parents’ postoperative pain measure: replication an extension to 2–6-year-old children. Pain 105:437–443
Goebel S, Grimm S, Raab P, Ettl V, Faller H (2011) The German version of parents’ postoperative pain measure (PPPM-D). Validation on children 2–12 years old. Schmerz 25:534–543
Wilton NC, Leigh J, Rosen DR, Pandit U (1988) Preanesthetic sedation of preschool children using intranasal midazolam. Anesthesiology 69:972–975
Leinbach RF, Markwell SJ, Colliver JA, Lin SY (2003) Hot vs cold tonsillectomy: a systematic review of the literature. Otolaryngol Head Neck Surg 129:360–364
Walther-Larsen S, Aagaard GB, Friis SM, Petersen T, Møller-Sonnergaard J, Rømsing J (2016) Structured intervention for management of pain following day surgery in children. Paediatr Anaesth 26:151–157
Berghmans JM, Poley MJ, van der Ende J et al (2018) Association between children’s emotional/behavioral problems before adenotonsillectomy and postoperative pain scores at home. Paediatr Anaesth 28:803–812
Vons KM, Bijker JB, Verwijs EW, Majoor HM, de Graaff JC (2014) Postoperative pain during the first week after adenoiectomy and guillotine adenotonsillectomy in children. Paediatr Anaesth 24:476–482
Xin Y, Li X, Du J, Cheng J, Yi C, Mao H (2019) Efficacy of telephone follow-up in children tonsillecomy with day surgery. Indian J Pediatr 86:263–266
McNab S (2016) Intravenous maintenance fluid therapy in children. J Paediatr Child Health 52:137–140
Morinière S, Roux A, Bakhos D et al (2013) Radiofrequency tonsillotomy versus bipolar scissors tonsillectomy for the treatment of OSAS in children: a prospective study. Eur Ann Otorhinolaryngol Head Neck Dis 130:67–72
Cantarella G, Viglione S, Forti S, Minetti A, Pignataro L (2012) Comparing postoerative quality of life in children after microdebrider intracapsular tonsillotomy and tonsillectomy. Auris Nasus Larynx 39:407–410
Steward DW, Ragg PG, Sheppard S, Chalkiadis GA (2012) The severity and duration of postoperative pain and analgesia requirements in children after tonsillecomy, orchidopexy, or inguinal hernia repair. Paediatr Anaesth 22:136–143
Büttner W, Finke W (2000) Analysis of behavioural and physiological parameters for the assessment of postoperative analgesic demand in newborns, infants and young children: a comprehensive report on seven consecutive studies. Paediatr Anaesth 10:303–318
de Azevedo CB, Carenzi LR, de Queiroz DL, Anselmo-Lima WT, Valera FC, Tamashiro E (2014) Clinical utility of PPPM and FPS-R to quantify post-tonsillecomy pain in children. Int J Pediatr Otorhinolaryngol 78:296–299
Birnie KA, Hundert AS, Lalloo C, Nguyen C, Stinson JN (2019) Recommendations for selection of self-report pain intensity measures in children and adolescents: a systematic review and quality assessment properties. Pain 160:5–18
Barbagallo M, Sacerdote P (2019) Ibuprofen in the treatment of children’s inflammatory pain: a clinical and pharmacological overview. Minerva Pediatr 71:82–99
Roberts CA, Shah-Becker S, O'Connell Ferster A et al (2018) Randomized prospective evaluation of intraoperative intravenous acetaminophen in pediatric adenotonsillectomy. Otolaryngol Head Neck Surg 158:368–374
Cohen N, Sommer DD (2016) Post-tonsillectomy pain control: consensus or controversy? Pain Manag 6:31–37
Zhang LY, Zhong L, David M, Cervin A (2017) Tonsillectomy or tonsillotomy? A systematic review for paediatric sleep-dispordered breathing. Int J Pediatr Otorhinolaryngol 103:41–50
Borgström A, Nerfeld P, Friberg D (2019) Postoperative pain and bleeding after adenotonsillectomy versus adenotonsillotomy in pediatric obstructive sleep apnea: an RCT. Eur Arch Otorhinolaryngol 276:3231–3238
Hayhurst CJ, Durieux ME (2016) Differential opioid tolerance and opioid-induced hyperalgesia. Anesthesiology 124:483–488
Kim SH, Lee MH, Seo H et al (2013) Intraoperative infusion of 0.6–0.9 µg kg(−1) min(−1) remifentanil induces acute tolerance in young children after laparoscopic uteroneocystostomy. Anesthesiology 118:337–343
Davis PJ, Finkel JC, Orr RJ et al (2000) A randomized, double-blinded study of remifentanil versus fentanil for tonsillectomy and adenoidectomy surgery in pediatric ambulatory surgical patients. Anesth Analg 90:863–871
Roulleau P, Gall O, Desjeux L, Dagher C, Murat I (2003) Remifentanil infusion for cleft palate surgery in young infants. Paediatr Anaesth 13:701–707
Acknowledgements
We thank Dr. Nicolai Bissantz, Ph.D. at the Faculty of Mathematics, Ruhr-University Bochum, Bochum, Germany for his statistical support and Dr. Tobias Rothoeft, University Children’s Hospital, Ruhr-University Bochum, Bochum for the critical review of the manuscript.
Funding
Departmental funding only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the Ethical Committee of the Ruhr-University Bochum, Bochum, Germany (registration number: 5108-14, 26 August 2015) and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual parents of the participating children included in the study. Moreover, children aged ≥ 7 years were age-appropriate informed about the study and asked to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gude, P., Gustedt, F., Bellgardt, M. et al. High dose ibuprofen as a monotherapy on an around-the-clock basis fails to control pain in children undergoing tonsil surgery: a prospective observational cohort study. Eur Arch Otorhinolaryngol 277, 2115–2124 (2020). https://doi.org/10.1007/s00405-020-05929-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05929-5