Abstract
Purpose
The objectives of this study were to observe the regulating effect of KTP laser and Nd:YAG laser in the repair of vocal fold scars.
Methods
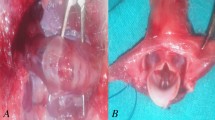
All rabbits were injured in the muscular layer with a sharp instrument, and then the vocal folds were treated with a KTP laser and a Nd:YAG laser at a power of 2, 4, 6 and 8 W 1 month after the injury. One month after treatment, the rabbits were killed and the throats were removed to detect changes in histology and gene expression of the vocal fold scar after laser therapy.
Results
The best efficacy of all KTP laser treatment groups was the KTP laser 6 W group. Regarding the detection of gene expression, in the KTP laser 6 W and Nd:YAG laser 6 W groups, col-3A1 was decreased compared to the scar group (P < 0.05), and col-1A1 was decreased only in the KTP laser 6 W group (P < 0.05). TGF-β1 levels in the two groups were lower than in the scar group. There were also significant differences in the levels of IL-1β, COX-2 and TNF-α in the two laser groups compared with the scar group (P < 0.05).
Conclusion
KTP laser and Nd:YAG laser treatments for vocal fold scars have particular therapeutic effects. The KTP laser may be better than the Nd:YAG laser for the regulation of vocal fold scars.
Level of evidence
NA.




Similar content being viewed by others
References
Hirano M, Jackson LC (1995) Phonosurgery: past, present, and future. Trans ABEA 25:22
Welham N, Choi SH, Dailey SH, Ford CN, Jiang JJ, Bless DM (2011) Prospective multi-arm evaluation of surgical treatments for vocal fold scar and pathologic sulcus vocalis. Laryngoscope 121(6):1252–1260
Hsiung MW, Woo P, Minasian A, Schaefer Mojica J (2000) Fat augmentation for glottic insufficiency. Laryngoscope 110(6):1026–1033
Hiwatashi N, Bing R, Kraja I, Branski RC (2017) Mesenchymal stem cells have antifibrotic effects on transforming growth factor-b1-stimulated vocal fold fibroblasts. Laryngoscope 127(1):E35–E41
Jennifer L (2010) Tissue engineering for treatment of vocal fold scar. Curr Opin Otolaryngol Head Neck Surg 18:521–525
Gugatschka M, Ohno S, Saxena A, Hirano S (2012) Regenerative medicine of the larynx. Where are we today? A review. J Voice 26(5):670.e7–670.e13
Casiraghi F, Remuzzi G, Abbate M, Perico N (2013) Multipotent mesenchymal stromal cell therapy and risk of malignancies. Stem Cell Rev 9(1):65–79
Herberts CA, Kwa MS, Hermsen HP (2011) Risk factors in the development of stem cell therapy. J Transl Med 22:9:29
Burns JA, Zeitels SM, Akst LM, Broadhurst MS, Hillman RE, Anderson R (2007) 532 nm pulsed potassium-titanyl-phosphate laser treatment of laryngeal papillomatosis under general anesthesia. Laryngoscope 117(8):1500–1504
Zeitels SM, Anderson RR, Hillman RE, Burns JA (2007) Experience with office-based pulsed-dye laser (PDL) treatment. Ann Otol Rhinol Laryngol 116(4):317–318
Mortensen MM, Woo P, Ivey C et al (2008) The use of the pulse dye laser in the treatment of vocal fold scar: a preliminary study. Laryngoscope 118(10):1884–1888
Lin Y, Yamashita M, Zhang J et al (2009) Pulsed dye laser-induced inflammatory response and extracellular matrix turnover in rat vocal folds and vocal fold fibroblasts. Lasers Surg Med 41(8):585–594
Sheu M, Sridharan S, Paul B, Mallur P, Gandonu S, Bing R, Zhou H, Branski RC, Amin MR (2013) The utility of the potassium titanyl phosphate laser in modulating vocal fold scar in a rat model. Laryngoscope 123(9):2189–2194
Xie X, Young J Kost K, McGregor M (2013) KTP 532 nm laser for laryngeal lesions. A systematic review. J Voice 27(2):245–249
Helman SN, Pitman MJ (2017) Office-based 532-nanometer pulsed potassium-titanyl-phosphate laser for marsupialization of laryngeal and vallecular mucoceles. Laryngoscope 127(5):1116–1118
Sheu M, Sridharan S, Kuhn M, Wang S, Paul B, Venkatesan N, Fuller CW, Simpson CB, Johns M, Branski RC, Amin MR (2012) Multi-institutional experience with the in-office potassium titanyl phosphate laser for laryngeal lesions. J Voice 26(6):806–810
Wojdas A, Szczygielski K, Kosek J, Ratajczak J, Jurkiewiczc D (2011) The application of KTP laser in otolaryngology—3 years experience. Otolaryngol Pol 65(4):281–284
Long JL (2010) Tissue engineering for treatment of vocal fold scar. Curr Opin Otolaryngol Head Neck Surg 18(6):521–525
Hahn MS, Teply BA, Stevens MM, Zeitels SM, Langer R (2006) Collagen composite hydrogels for vocal fold lamina propria restoration. Biomaterials 27(7):1104–1109
Friedrich G, Dikkers FG, Arens C, Remacle M, Hess M, Giovanni A, Duflo S, Hantzakos A, Bachy V, Gugatschka M, European Laryngological Society, Phonosurgery Committee (2013) Vocal fold scars: current concepts and future directions. Consensus report of the Phonosurgery Committee of the European Laryngological Society. Eur Arch Otorhinolaryngol 270(9):2491–2507
Ehrlich H, Garg H, Longaker MT (2000) Scarless wound healing. Marcel Dekker, New York, pp 99–114
Longaker MT, Whitby DJ, Adzick NS et al (1990) Studies in fetal wound healing: VI. Second and early third trimester fetal wounds demonstrate rapid collagen deposition without scar formation. J Pediatr Surg 25(1):63–68
Morykwas MJ, Ledbetter MS, Ditesheim JA, White WL, Vander Ark AD, Argenta LC (1991) Cellular inflammation of fetal excisional wounds: effects of amniotic fluid exclusion. Inflammation 15(3):173–180
Frantz FW, Bettinger DA, Haynes JH et al (1993) Biology of fetal repair: the presence of bacteria in fetal wounds induces an adult-like healing response. J Pediatr Surg 28(3):428–433
Kumta S, Ritz M, Hurley JV, Crowe D, Romeo R, O’Brien BM (1994) Acute inflammation in foetal and adult sheep: the response to subcutaneous injection of turpentine and carrageenan. Br J Plast Surg 47(5):360–368
Zhou H, Felsen D, Sandulache VC, Amin MR, Kraus DH, Branski RC (2011) Prostaglandin (PG)E2 exhibits antifibrotic activity in vocal fold fibroblasts. Laryngoscope 121(6):1261–1265
Lim X, Tateya I, Tateya T et al (2006) Immediate inflammatory response and scar formation in wounded vocal folds. Ann Otol Rhinol Laryngol 115(12):921–929
Welham NV, Lim X, Tateya I, Bless DM (2008) Inflammatory factor profiles one hour following vocal fold injury. Ann Otol Rhinol Laryngol 117(2):145–152
Rousseau B, Ge PJ, Ohno T et al (2008) Extracellular matrix gene expression after vocal fold injury in a rabbit model. Ann Otol Rhinol Laryngol 117(8):598–603
. Graupp M, Gruber HJ, Weiss G, Kiesler K, Bachna-Rotter S, Friedrich G, Gugatschka M (2015) Establishing principles of macromolecular crowding for in vitro fibrosis research of the vocal fold lamina propria. Laryngoscope 125(6):203–209
Derynck R, Zhang YE (2003) Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature 425(6958):577–584
Zhang YE (2009) Non-Smad pathways in TGF-β signaling. Cell Res 19(1):128–139
Chang Z, Kishimoto Y, Hasan A, Welham NV (2014) TGF-β3 modulates the inflammatory environment and reduces scar formation following vocal fold mucosal injury in rats. Dis Model Mech 7(1):83–91
Karbiener M, Darnhofer B, Frisch MT, Rinner B, Birner-Gruenberger R, Gugatschka M (2017) Comparative proteomics of paired vocal fold and oral mucosa fibroblasts. J Proteom 23(155):11–21
Szpaderska AM, Zuckerman JD, DiPietro LA (2003) Differential injury responses in oral mucosal and cutaneous wounds. J Dent Res 82(8):621–626
Kwak DH, Bae TH, Kim WS, Kim HK (2016) Anti-vascular endothelial growth factor (Bevacizumab) therapy reduces hypertrophic scar formation in a rabbit ear wounding model. Arch Plast Surg 43(6):491–497
van der Veer WM, Niessen FB, Ferreira JA et al (2011) Time course of the angiogenic response during normotrophic and hypertrophic scar formation in humans. Wound Repair Regen 19(3):292–301
Gawronska-Kozak B (2011) Scarless skin wound healing in FOXN1 deficient (nude) mice is associated with distinctive matrix metalloproteinase expression. Matrix Biol 30(4):290–300
Li H, Nahas Z, Feng F, Elisseeff JH, Boahene K (2013) Tissue engineering for in vitro analysis of matrix metalloproteinases in the pathogenesis of keloid lesions. JAMA Facial Plast Surg 15(6):448–456
Knittel T, Mehde M, Grundmann A, Saile B, Scharf JG, Ramadori G (2000) Expression of matrix metalloproteinases and their inhibitors during hepatic tissue repair in the rat. Histochem Cell Biol 113(6):443–453
Funding
This study received no financial support or funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work; there is no professional or other personal interest of any nature or kind in any product, service and/or company that could be construed as influencing the position presented in, or the review of, the manuscript entitled.
Ethical approval
All animal procedures followed a protocol approved by the Institutional Animal Care and Use Committee at Fudan University.
Rights and permissions
About this article
Cite this article
Zhang, J., Zhen, R. & Wei, C. Potassium titanyl phosphate laser-induced inflammatory response and extracellular matrix turnover in rabbit vocal fold scar. Eur Arch Otorhinolaryngol 275, 1525–1532 (2018). https://doi.org/10.1007/s00405-018-4957-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4957-9