Abstract
Introduction
Head and neck extramedullary plasmacytoma is a rare localized plasma cell neoplasm. We intended to perform this review of the published literature to assess the demographic profile, pattern of care and survival outcomes.
Methods
Two authors independently searched PubMed, Google search and Cochrane library for eligible studies from 1950 till July 1, 2016, published in English language.
Results
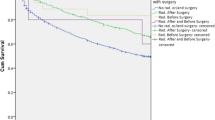
Median age of the cohort was 57 years (range 11–85). Site-wise distributions were paranasal sinuses 22.3% (70), nasal cavity 17.5% (55), nasopharynx 10.8% (34). Median size of SEMP was 3 cm (range 0.3–12 cm). Treatment distribution was radiotherapy (RT) in 52% (164), surgery (S) 19% (60), chemotherapy (C) 5% (16), S + RT 23.49% (74),CRT 1.9% (6), S + C 0.6% (2), S + RT + C 0.95% (3).Radiation was used as a modality in 78.4%(247), surgery in 44.1%(139), chemotherapy in 4.8%(15). Median radiation dose used was 45 Gy with range 20–61 Gy. Median overall survival (OS) was 40 months (range 0.5–298). Median local progression-free survival was 36 months (range 0–298). Median myeloma relapse-free survival was 36 months (range 0.5–298). Five- and 10-year OS was 78.33 and 68.61%. Five-year cause-specific survival (CSS) and 10-year CSS was 90.15 and 83.31%. Five-year LPFS was 94.78%, and 10-year LPFS was 88.43%. Five-year myeloma progression-free survival was 84.46%, and 10-year myeloma PFS was 80.44%. The factors associated with risk of local relapse were site of disease (sinonasal), secretory EMP, type of treatment received (surgery + RT > RT alone > surgery on univariate analysis). Risk factors for myeloma relapse were coexisting diseases, site of disease (sinonasal), bony erosion, size of lesion > 5 cm and type of treatment received on univariate analysis.
Conclusion
Our study shows that combined modality S + RT is superior compared to uni-modality in preventing local recurrence. Radiation dose of 45 Gy is optimal. Nodal irradiation has no impact on local recurrence.




Similar content being viewed by others
References
Mendenhall WM, Mendenhall CM, Mendenhall NP (2003) Solitary plasmacytoma of bone and soft tissues. Am J Otolaryngol 24(6):395–399
Pahor AL (1977) Extramedullary plasmacytoma of the head and neck, parotid and submandibular salivary glands. J Laryngol Otol 91(3):241–258
Susnerwala SS, Shanks JH, Banerjee SS, Scarffe JH, Farrington WT, Slevin NJ (1997) Extramedullary plasmacytoma of the head and neck region: clinicopathological correlation in 25 cases. Br J Cancer 75(6):921–927
Knowling MA, Harwood AR, Bergsagel DE (1983) Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol Off J Am Soc Clin Oncol 1(4):255–262
Ozsahin M, Tsang RW, Poortmans P, Belkacémi Y, Bolla M, Dinçbas FO et al (2006) Outcomes and patterns of failure in solitary plasmacytoma: a multicenter Rare Cancer Network study of 258 patients. Int J Radiat Oncol Biol Phys 1(1):210–217 64(
Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R (1999) Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol J Eur Soc Ther Radiol Oncol 52(3):245–249
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Med 6(7):e1000097
Kilciksiz S, Celik OK, Pak Y, Demiral AN, Pehlivan M, Orhan O et al (2008) Clinical and prognostic features of plasmacytomas: a multicenter study of Turkish Oncology Group-Sarcoma Working Party. Am J Hematol 83(9):702–707
Li Q-W, Niu S-Q, Wang H-Y, Wen G, Li Y-Y, Xia Y-F et al (2015) Radiotherapy Alone is Associated with Improved Outcomes Over Surgery in the Management of Solitary Plasmacytoma. Asian Pac J Cancer Prev APJCP 16(9):3741–3745
Gerry D, Lentsch EJ (2013) Epidemiologic evidence of superior outcomes for extramedullary plasmacytoma of the head and neck. Otolaryngol–Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg 148(6):974–981
Tournier-Rangeard L, Lapeyre M, Graff-Caillaud P, Mege A, Dolivet G, Toussaint B et al (2006) Radiotherapy for solitary extramedullary plasmacytoma in the head-and-neck region: a dose greater than 45 Gy to the target volume improves the local control. Int J Radiat Oncol Biol Phys 64(4):1013–1017
Smedt BD, Vanderstraeten B, Reynaert N, Gersem WD, Neve WD, Thierens H (2007) The influence of air cavities within the PTV on Monte Carlo-based IMRT optimization. J Phys Conf Ser 74(1):021003
Haraldsson P, Knöös T, Nyström H, Engström P (2003) Monte Carlo study of TLD measurements in air cavities. Phys Med Biol 48(18):N253–N259
Suh Y-G, Suh C-O, Kim JS, Kim S-J, Pyun HO, Cho J (2012) Radiotherapy for solitary plasmacytoma of bone and soft tissue: outcomes and prognostic factors. Ann Hematol 91(11):1785–1793
Reed V, Shah J, Medeiros LJ, Ha CS, Mazloom A, Weber DM et al (2011) Solitary plasmacytomas Cancer 117(19):4468–4474
Galieni P, Cavo M, Avvisati G, Pulsoni A, Falbo R, Bonelli MA et al (1995) Solitary plasmacytoma of bone and extramedullary plasmacytoma: two different entities? Ann Oncol 6(7):687–691
Hill QA, Rawstron AC, Tute RM de, Owen RG (2014) Outcome prediction in solitary plasmacytoma of bone: a risk stratification model utilizing bone marrow flow cytometry and light chain analysis. Blood 124(8):1296–1299
Tsang RW, Gospodarowicz MK, Pintilie M, Bezjak A, Wells W, Hodgson DC et al (2001) Solitary plasmacytoma treated with radiotherapy: impact of tumor size on outcome. Int J Radiat Oncol Biol Phys 50(1):113–120
Strojan P, Soba E, Lamovec J, Munda A (2002) Extramedullary plasmacytoma: clinical and histopathologic study. Int J Radiat Oncol Biol Phys 53(3):692–701
Patel TD, Vázquez A, Choudhary MM, Kam D, Baredes S, Eloy JA (2015) Sinonasal extramedullary plasmacytoma: a population-based incidence and survival analysis. Int Forum Allergy Rhinol 5(9):862–869
D’Aguillo C, Soni RS, Gordhan C, Liu JK, Baredes S, Eloy JA (2014 Sinonasal extramedullary plasmacytoma: a systematic review of 175 patients. Int Forum Allergy Rhinol 4(2):156–163
Sasaki R, Yasuda K, Abe E, Uchida N, Kawashima M, Uno T et al (2012) Multi-institutional analysis of solitary extramedullary plasmacytoma of the head and neck treated with curative radiotherapy. Int J Radiat Oncol 82(2):626–634
Thumallapally N, Meshref A, Mousa M, Terjanian T (2017) Solitary plasmacytoma: population-based analysis of survival trends and effect of various treatment modalities in the USA. BMC Cancer [Internet]. 2017 Jan 5 [cited 2017 Apr 16];17. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5216567/. Accessed 2017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have nothing to disclose.
Funding
No financial support received.
Conflicts of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Venkatesulu, B., Mallick, S., Giridhar, P. et al. Pattern of care and impact of prognostic factors on the outcome of head and neck extramedullary plasmacytoma: a systematic review and individual patient data analysis of 315 cases. Eur Arch Otorhinolaryngol 275, 595–606 (2018). https://doi.org/10.1007/s00405-017-4817-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4817-z