Abstract
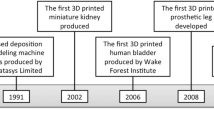
Three-dimensional (3D) printing is a promising technology that can use a patient’s image data to create complex and personalized constructs precisely. It has made great progress over the past few decades and has been widely used in medicine including medical modeling, surgical planning, medical education and training, prosthesis and implants. Three-dimensional (3D) bioprinting is a powerful tool that has the potential to fabricate bioengineered constructs of the desired shape layer-by-layer using computer-aided deposition of living cells and biomaterials. Advances in 3D printed implants and future tissue-engineered constructs will bring great progress to the field of otolaryngology. By integrating 3D printing into tissue engineering and materials, it may be possible for otolaryngologists to implant 3D printed functional grafts into patients for reconstruction of a variety of tissue defects in the foreseeable future. In this review, we will introduce the current state of 3D printing technology and highlight the applications of 3D printed prosthesis and implants, 3D printing technology combined with tissue engineering and future directions of bioprinting in the field of otolaryngology.


Similar content being viewed by others
References
Hull CW iU, Inc, assignee (1986) Apparatus for production of three-dimensional objects by stereolithography. US Patent 4,575,330 11
Zadpoor AA, Malda J (2017) Additive manufacturing of biomaterials, tissues, and organs. Ann Biomed Eng 45(1):1–11. doi:10.1007/s10439-016-1719-y
Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, Giesel FL (2010) 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 5(4):335–341. doi:10.1007/s11548-010-0476-x
Schubert C, van Langeveld MC, Donoso LA (2014) Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol 98(2):159–161. doi:10.1136/bjophthalmol-2013-304446
Marro A, Bandukwala T, Mak W (2016) Three-dimensional printing and medical imaging: a review of the methods and applications. Curr Probl Diagn Radiol 45(1):2–9. doi:10.1067/j.cpradiol.2015.07.009
Bartellas M, Ryan S, Doucet G, Murphy D, Turner J (2017) Three-dimensional printing of a hemorrhagic cervical cancer model for postgraduate gynecological training. Cureus 9(1):e950. doi:10.7759/cureus.950
Madurska MJ, Poyade M, Eason D, Rea P, Watson AJ (2017) Development of a patient-specific 3D-printed liver model for preoperative planning. Surg Innov 24(2):145–150. doi:10.1177/1553350616689414
Marconi S, Pugliese L, Botti M, Peri A, Cavazzi E, Latteri S, Auricchio F, Pietrabissa A (2017) Value of 3D printing for the comprehension of surgical anatomy. Surg Endosc. doi:10.1007/s00464-017-5457-5
Zuniga JM, Carson AM, Peck JM, Kalina T, Srivastava RM, Peck K (2017) The development of a low-cost three-dimensional printed shoulder, arm, and hand prostheses for children. Prosthet Orthot Int 41(2):205–209. doi:10.1177/030936461664
Callahan AB, Campbell AA, Petris C, Kazim M (2017) Low-cost 3D printing orbital implant templates in secondary orbital reconstructions. Ophthalmic Plast Reconstr Surg. doi:10.1097/IOP.0000000000000884
Cohen J, Reyes SA (2015) Creation of a 3D printed temporal bone model from clinical CT data. Am J Otolaryngol 36(5):619–624. doi:10.1016/j.amjoto.2015.02.012
Nuseir A, Hatamleh M, Watson J, Al-Wahadni AM, Alzoubi F, Murad M (2015) Improved construction of auricular prosthesis by digital technologies. J Craniofac Surg 26(6):e502–505. doi:10.1097/SCS.0000000000002012
Kozin ED, Remenschneider AK, Cheng S, Nakajima HH, Lee DJ (2015) Three-dimensional printed prosthesis for repair of superior canal dehiscence. Otolaryngol Head Neck Surg 153(4):616–619. doi:10.1177/0194599815592602
Owusu JA, Boahene K (2015) Update of patient-specific maxillofacial implant. Curr Opin Otolaryngol Head Neck Surg 23(4):261–264. doi:10.1097/MOO.0000000000000175
AlReefi MA, Nguyen LH, Mongeau LG, Haq BU, Boyanapalli S, Hafeez N, Cegarra-Escolano F, Tewfik MA (2016) Development and validation of a septoplasty training model using 3-dimensional printing technology. Int Forum Allergy Rhinol. doi:10.1002/alr.21887
Chan HH, Siewerdsen JH, Vescan A, Daly MJ, Prisman E, Irish JC (2015) 3D rapid prototyping for otolaryngology-head and neck surgery: applications in image-guidance, surgical simulation and patient-specific modeling. PLoS One 10(9):e0136370. doi:10.1371/journal.pone.0136370
Malda J, Visser J, Melchels FP, Jüngst T, Hennink WE, Dhert WJ, Groll J, Hutmacher DW (2013) 25th anniversary article: engineering hydrogels for biofabrication. Adv Mater 25(36):5011–5028. doi:10.1002/adma.201302042
Murphy SV, Atala A (2014) 3D bioprinting of tissues and organs. Nat Biotechnol 32(8):773–785. doi:10.1038/nbt.2958
Gu BK, Choi DJ, Park SJ, Kim MS, Kang CM, Kim CH (2016) 3-dimensional bioprinting for tissue engineering applications. Biomater Res 20:12. doi:10.1186/s40824-016-0058-2
Ozbolat IT (2015) Bioprinting scale-up tissue and organ constructs for transplantation. Trends Biotechnol 33(7):395–400. doi:10.1016/j.tibtech.2015.04.005
Ozbolat IT, Peng W, Ozbolat V (2016) Application areas of 3D bioprinting. Drug Discov Today 21(8):1257–1271. doi:10.1016/j.drudis.2016.04.006
Knowlton S, Onal S, Yu CH, Zhao JJ, Tasoglu S (2015) Bioprinting for cancer research. Trends Biotechnol 33(9):504–513. doi:10.1016/j.tibtech.2015.06.007
Snyder JE, Hamid Q, Wang C, Chang R, Emami K, Wu H, Sun W (2011) Bioprinting cell-laden matrigel for radioprotection study of liver by pro-drug conversion in a dual-tissue microfluidic chip. Biofabrication 3(3):034112. doi:10.1088/1758-5082/3/3/034112
Vorwerk U, Begall K (1998) Practice surgery on the artificial temporal bone. Development of temporal bone facsimiles with stereolithography. HNO 46(3):246–251
Suzuki M, Ogawa Y, Kawano A, Hagiwara A, Yamaguchi H, Ono H (2004) Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol 124(4):400–402
Monfared A, Mitteramskogler G, Gruber S, Salisbury JK Jr, Stampfl J, Blevins NH (2012) High-fidelity, inexpensive surgical middle ear simulator. Oto Neurotol 33(9):1573–1577. doi:10.1097/MAO.0b013e31826dbca5
Wulf J, Rohde L, Koppe T, Winder RJ (2012) Three-dimensional micro-imaging (μCT) based physical anatomic teaching models: implementation of a new learning aid for routine use in anatomy lectures. Stud Health Technol Inf 173:549–551
Rose AS, Kimbell JS, Webster CE, Harrysson OL, Formeister EJ, Buchman CA (2015) Multi-material 3D models for temporal bone surgical simulation. Ann Otol Rhinol Laryngol 124(7):528–536. doi:10.1177/0003489415570937
Longfield EA, Brickman TM, Jeyakumar A (2015) 3D printed pediatric temporal bone: a novel training model. Otol Neurotol 36(5):793–795. doi:10.1097/MAO.0000000000000750
Da Cruz MJ, Francis HW (2015) Face and content validation of a novel three-dimensional printed temporal bone for surgical skills development. J Laryngol Otol 129(Suppl 3):S23–S29. doi:10.1017/S0022215115001346
Hochman JB, Rhodes C, Wong D, Kraut J, Pisa J, Unger B (2015) Comparison of cadaveric and isomorphic three-dimensional printed models in temporal bone education. Laryngoscope 125(10):2353–2357. doi:10.1002/lary.24919
Mowry SE, Jammal H, Myer C 4th, Solares CA, Weinberger P (2015) A novel temporal bone simulation model using 3D printing techniques. Otol Neurotol 36(9):1562–1565. doi:10.1097/MAO.0000000000000848
Kuru L, Maier H, Müller M, Lenarz T, Lueth TC (2016) A 3D-printed functional anatomical human middle ear model. Hear Res 340:204–213. doi:10.1016/j.heares.2015.12.025
Wanibuchi M, Noshiro S, Sugino T, Akiyama Y, Mikami T, Iihoshi S, Miyata K, Komatsu K, Mikuni N (2016) Training for skull base surgery with a colored temporal bone model created by three-dimensional printing technology. World Neurosurg 91:66–72. doi:10.1016/j.wneu.2016.03.084
Berens AM, Newman S, Bhrany AD, Murakami C, Sie KC, Zopf DA (2016) Computer-aided design and 3D printing to produce a costal cartilage model for simulation of auricular reconstruction. Otolaryngol Head Neck Surg 155(2):356–359. doi:10.1177/0194599816639586
Alrasheed AS, Nguyen LHP, Mongeau L, Funnell WRJ, Tewfik MA (2017) Development and validation of a 3D-printed model of the ostiomeatal complex and frontal sinus for endoscopic sinus surgery training. Int Forum Allergy Rhinol 7(8):837–841. doi:10.1002/alr.21960
Chang DR, Lin RP, Bowe S, Bunegin L, Weitzel EK, McMains KC, Willson T, Chen PG (2017) Fabircation and validation of a low-cost, medium-fidelity silicone injection molded endoscopic sinus surgery simulation model. Laryngoscope 127(4):781–786. doi:10.1002/lary.26370
Tai BL, Wang AC, Joseph JR, Wang PI, Sullivan SE, McKean EL, Shih AJ, Rooney DM (2016) A physical simulator for endoscopic endonasal drilling techniques: technical note. J Neurosurg 124(3):811–816. doi:10.3171/2015.3.JNS1552
Sander IM, Liepert TT, Doney EL, Leevy WM, Liepert DR (2017) Patient education for endoscopic sinus surgery: preliminary experience using 3D-printed clinical imaging data. J Funct Biomater 8(2):E13. doi:10.3390/jfb8020013
Chiesa Estomba CM, González Fernández I, Iglesias Otero MÁ (2016) How we do it: anterior and posterior nosebleed trainer, the 3D printing epistaxis project. Clin Otolaryngol. doi:10.1111/coa.12711
Danti S, D’Alessandro D, Pietrabissa A, Petrini M, Berrettini S (2009) Development of tissue-engineered substitutes of the ear ossicles: PORP-shaped poly(propylene fumarate)-based scaffolds cultured with human mesenchymal stromal cells. J Biomed Mater Res A 92(4):1343–1356. doi:10.1002/jbm.a.32447
Martin AD, Harner SG (2004) Ossicular reconstruction with titanium prosthesis. Laryngoscope 114(1):61–64
Baker AB, O’Connell BP, Nguyen SA, Lambert PR (2015) Ossiculoplasty with titanium prostheses in patients with intact stapes: comparison of TORP versus PORP. Otol Neurotol 36(10):1676–1682. doi:10.1097/MAO.0000000000000893
Goldenberg RA, Driver M (2000) Long-term results with hydroxylapatite middle ear implants. Otolaryngol Head Neck Surg 122(5):635–642
Xiong Y, Chen P, Sun J (2012) Studies on personalized porous titanium implant fabricated using three-dimensional printing forming technique. J Biomed Eng 29(2):247–250 (article in Chinese)
Li XS, Sun JJ, Jiang W, Liu X (2009) Effect on cochlea function by tissue-engineering osside prosthets containing controlled release bone morphogenetic protein 2 transplanted into acoustic build in guinea pig. Chin J Otorhinolaryngol Head Neck Surg 44(6):490–493 (article in Chinese)
Phillippi JA, Miller E, Weiss L, Huard J, Waggoner A, Campbell P (2008) Microenvironments engineered by inkjet bioprinting spatially direct adult stem cells toward muscle-and bone-like subpopulations. Stem Cells 26(1):127–134. doi:10.1634/stemcells.2007-0520
Sandström C (2015) Adopting 3D printing for manufacturing-evidence from the hearing aid industry. Technol Forecast Soc Change 102:160–168
Kaye R, Goldstein T, Zeltsman D, Grande DA, Smith LP (2016) Three dimensional printing: a review on the utility within medicine and otolaryngology. Int J Pediatr Otorhinolaryngol 89:145–148. doi:10.1016/j.ijporl.2016.08.007
Bos EJ, Scholten T, Song Y, Verlinden JC, Wolff J, Forouzanfar T, Helder MN, van Zuijlen P (2015) Developing a parametric ear model for auricular reconstruction: a new step towards patient-specific implants. J Craniomaxillofac Surg 43(3):390–395. doi:10.1016/j.jcms.2014.12.016
Watson J, Hatamleh MM (2014) Complete integration of technology for improved reproduction of auricular prostheses. J Prosthet Dent 111(5):430–436. doi:10.1016/j.prosdent.2013.07.018
Zopf DA, Mitsak AG, Flanagan CL, Wheeler M, Green GE, Hollister SJ (2015) Computer aided-designed, 3-dimensionally printed porous tissue bioscaffolds for craniofacial soft tissue reconstruction. Otolaryngol Head Neck Surg 152(1):57–62. doi:10.1177/0194599814552065
Suaste-Gómez E, Rodríguez-Roldán G, Reyes-Cruz H, Terán-Jiménez O (2016) Developing an ear prosthesis fabricated in polyvinylidene fluoride by a 3D printer with sensory intrinsic properties of pressure and temperature. Sensors 16(3):332. doi:10.3390/s16030332
Guillemot F, Souquet A, Catros S et al (2010) High-throughput laser printing of cells and biomaterials for tissue engineering. Acta Biomater 6(7):2494–2500. doi:10.1016/j.actbio.2009.09.029
Cui X, Breitenkamp K, Finn MG, Lotz M, D’Lima DD (2012) Direct human cartilage repair using three-dimensional bioprinting technology. Tissue Eng Part A 18(11–12):1304–1312. doi:10.1089/ten.TEA.2011.0543
Fedorovich NE, Schuurman W, Wijnberg HM, Prins HJ, van Weeren PR, Malda J, Alblas J, Dhert WJ (2012) Biofabrication of osteochondral tissue equivalents by printing topologically defined, cell-laden hydrogel scaffolds. Tissue Eng Part C Methods 18(1):33–44. doi:10.1089/ten.TEC.2011.0060
Markstedt K, Mantas A, Tournier I, Martinez Avila H, Hagg D, Gatenholm P (2015) 3D bioprinting human chondrocytes with nanocellulose-alginate bioink for cartilage tissue engineering applications. Biomacromolecules 16(5):1489–1496. doi:10.1021/acs.biomac.5b00188
Park JY, Choi YJ, Shim JH, Park JH, Cho DW (2017) Development of a 3D cell printed structure as an alternative to autologs cartilage for auricular reconstruction. J Biomed Mater Res B Appl Biomater. doi:10.1002/jbm.b.33639
Lee JS, Hong JM, Jung JW, Shim JH, Oh JH, Cho DW (2014) 3D printing of composite tissue with complex shape applied to ear regeneration. Biofabrication 6(2):024103. doi:10.1088/1758-5082/6/2/024103
Mannoor MS, Jiang Z, James T, Kong YL, Malatesta KA, Soboyejo WO, Verma N, Gracias DH, McAlpine MC (2013) 3D printed bionic ears. Nano Lett 13(6):2634–2639
Monasta L, Ronfani L, Marchetti F, Montico M, Vecchi Brumatti L, Bavcar A, Grasso D, Barbiero C, Tamburlini G (2012) Burden of disease caused by otitis media: systematic review and global estimates. PLoS One 7(4):e36226. doi:10.1371/journal.pone.0036226
Boedts D, De Cock M, Andries L, Marquet J (1990) A scanning electron-microscopic study of different tympanic grafts. Am J Otol 11(4):274–277
Kozin ED, Black NL, Cheng JT, Cotler MJ, McKenna MJ, Lee DJ, Lewis JA, Rosowski JJ, Remenschneider AK (2016) Design, fabrication, and in vitro testing of novel three-dimensionally printed tympanic membrane grafts. Hear Res 340:191–203. doi:10.1016/j.heares.2016.03.005
Kuo CY, Wilson E, Fuson A, Gandhi N, Monfaredi R, Jenkins A, Romero M, Santoro M, Fisher JP, Cleary K, Reilly B (2017) Repair of tympanic membrane perforations with customized, bioprinted ear grafts using chinchilla models. Tissue Eng Part A. doi:10.1089/ten.TEA.2017.0246
Onerci Altunay Z, Bly JA, Edwards PK, Holmes DR, Hamilton GS, O’Brien EK, Carr AB, Camp JJ, Stokken JK, Pallanch JF (2016) Three dimensional printing of large nasal septal perforations for optimal prosthetic closure. Am J Rhinol Allergy 30(4):287–293. doi:10.2500/ajra.2016.30.4324
Stokken JK, Pallanch JF (2017) The emerging role of 3-dimensional printing in rhinology. Otolaryngol Clin N Am 50(3):583–588. doi:10.1016/j.otc.2017.01.014
Choi YD, Kim Y, Park E (2017) Patient-specific augmentation rhinoplasty using a three-dimensional simulation program and three-dimensional printing. Aesthet Surg J. doi:10.1093/asj/sjx046
Kim YS, Shin YS, Park DY, Choi JW, Park JK, Kim DH, Kim CH, Park SA (2015) The application of three-dimensional printing in animal model of augmentation rhinoplasty. Ann Biomed Eng 43(9):2153–2162. doi:10.1007/s10439-015-1261-3
Park SH, Yun BG, Won JY et al (2017) New application of three-dimensional printing biomaterial in nasal reconstruction. Laryngoscope 127(5):1036–1043. doi:10.1002/lary.26400
Goyal V, Masters IB, Chang AB (2005) Interventions for primary (intrinsic) tracheomalacia in children. Cochrane Database Syst Rev 10:CD005304. doi:10.1002/14651858.CD005304.pub3
Zopf DA, Hollister SJ, Nelson ME, Ohye RG, Green GE (2013) Bioresorbable airway splint created with a three-dimensional printer. N Engl J Med 368(21):2043–2045. doi:10.1056/NEJMc1206319
Kuehn BM (2016) Clinicians embrace 3D printers to solve unique clinical challenges. JAMA 315(4):333–335. doi:10.1001/jama.2015.17705
Kaye R, Goldstein T, Aronowitz D, Grande DA, Zeltsman D, Smith LP (2017) Ex vivo tracheomalacia model with 3D-printed external tracheal splint. Laryngoscope 127(4):950–955. doi:10.1002/lary.26213
Huang L, Wang L, He J, Zhao J, Zhong D, Yang G, Guo T, Yan X, Zhang L, Li D, Cao T, Li X (2016) Tracheal suspension by using 3-dimensional printed personalized scaffold in a patient with tracheomalacia. J Thorac Dis 8(11):3323–3328. doi:10.21037/jtd.2016.10.53
Guibert N, Moreno B, Hermant C (2017) Usefulness of 3D printing to manage complex tracheal stenosis. J Bronchology Interv Pulmonol 24(2):e27–e29. doi:10.1097/LBR.0000000000000380
Law JX, Liau LL, Aminuddin BS, Ruszymah BH (2016) Tissue-engineered trachea: a review. Int J Pediatr Otorhinolaryngol 91:55–63. doi:10.1016/j.ijporl.2016.10.012
Grillo HC (2002) Tracheal replacement: a critical review. Ann Thorac Surg 73(6):1995–2004
Den Hondt M, Vranckx JJ (2017) Reconstruction of defects of the trachea. J Mater Sci Mater Med 28(2):24. doi:10.1007/s10856-016-5835-x
Delaere P, Vranckx J, Verleden G, De Leyn P, Van Raemdonck D, Leuven Tracheal Transplant Group (2010) Tracheal allotransplantation after withdrawal of immunosuppressive therapy. N Engl J Med 362(2):138–145. doi:10.1056/NEJMoa0810653
Conconi MT, De Coppi P, Di Liddo R, Vigolo S, Zanon GF, Parnigotto PP, Nussdorfer GG (2005) Tracheal matrices, obtained by a detergent-enzymatic method, support in vitro the adhesion of chondrocytes and tracheal epithelial cells. Transpl Int 18(6):727–734
Badylak SF, Freytes DO, Gilbert TW (2009) Extracellular matrix as a biological scaffold material: structure and function. Acta Biomater 5(1):1–13. doi:10.1016/j.actbio.2008.09.013
Macchiarini P, Jungebluth P, Go T et al (2008) Clinical transplantation of a tissue-engineered airway. Lancet 372(9655):2023–2030. doi:10.1016/S01406736(08)61598-6
Gonfiotti A, Jaus MO, Barale D et al (2014) The first tissue-engineered airway transplantation: 5-year follow-up results. Lancet 383(9913):238–244. doi:10.1016/s0140-6736(13)62033-4
Ott LM, Zabel TA, Walker NK, Farris AL, Chakroff JT, Ohst DG, Johnson JK, Gehrke SH, Weatherly RA, Detamore MS (2016) Mechanical evaluation of gradient electrospun scaffolds with 3D printed ring reinforcements for tracheal defect repair. Biomed Mater 11(2):025020. doi:10.1088/1748-6041/11/2/025020
Stannard W, O’Callaghan C (2006) Ciliary function and the role of cilia in clearance. J Aerosol Med 19(1):110–115
Chang JW, Park SA, Park JK, Choi JW, Kim YS, Shin YS, Kim CH (2014) Tissue-engineered tracheal reconstruction using three-dimensionally printed artificial tracheal graft: preliminary report. Artif Organs 38(6):E95–E105. doi:10.1111/aor.12310
Park JH, Park JY, Nam IC, Hwang SH, Kim CS, Jung JW, Jang J, Lee H, Choi Y, Park SH, Kim SW, Cho DW (2015) Human turbinate mesenchymal stromal cell sheets with bellows graft for rapid tracheal epithelial regeneration. Acta Biomater 25:56–64. doi:10.1016/j.actbio.2015.07.014
Park JH, Hong JM, Ju YM, Jung JW, Kang HW, Lee SJ, Yoo JJ, Kim SW, Kim SH, Cho DW (2015) A novel tissue-engineered trachea with a mechanical behavior similar to native trachea. Biomaterials 62:106–115. doi:10.1016/j.biomaterials.2015.05.008
Goldstein TA, Smith BD, Zeltsman D, Grande D, Smith LP (2015) Introducing a 3-dimensionally printed, tissue-engineered graft for airway reconstruction: a pilot study. Otolaryngol Head Neck Surg 153(6):1001–1006. doi:10.1177/0194599815605492
Rehmani SS, Al-Ayoubi AM, Ayub A, Barsky M, Lewis E, Flores R, Lebovics R, Bhora FY (2017) Three-dimensional-printed bioengineered tracheal grafts: preclinical results and potential for human use. Ann Thorac Surg. doi:10.1016/j.athoracsur.2017.03.051
Gao M, Zhang H, Dong W et al (2017) Tissue-engineered trachea from a 3D-printed scaffold enhances whole-segment tracheal repair. Sci Rep 7(1):5246. doi:10.1038/s41598-017-05518-3
Kontio R (2014) Update on mandibular reconstruction: computer-aided design, imaging, stem cells and future applications. Curr Opin Otolaryngol Head Neck Surg 22(4):307–315. doi:10.1097/MOO.0000000000000065
Lee M, DeConde A, Aghaloo T, Lee M, Tetradis S, St. John M (2013) Biomimetic scaffolds loaded with adipose-derived stem cells and BMP-2 induce healing of mandibular defects. Otolaryngol Head and Neck Surg 149(2 Suppl):35–36
(2015) The world’s first AM mandible implant. http://www.layerwisecom/the-worldsfirst-patient-specific-am-lower-jaw/. Accessed 22 Feb 2015
Griffith H (2015) Pioneering 3D printing reshapes patient’s face in Wales. http://www.bbccom/news/uk-wales-26534408. Accessed 22 Feb 2015
Rachmiel A, Shilo D, Blanc O, Emodi O (2017) Reconstruction of complex mandibular defects using integrated dental custom-made titanium implants. Br J Oral Maxillofac Surg 55(4):425–427. doi:10.1016/j.bjoms.2017.01.006
Qassemyar Q, Assouly N, Temam S, Kolb F (2017) Use of a three-dimensional custom-made porous titanium prosthesis for mandibular body reconstruction. Int J Oral Maxillofac Surg. doi:10.1016/j.ijom.2017.06.001
Lu YCF, Zhao X, Shao ZZ, Cao ZB (2006) Experimental study on facial nerve regeneration by porous silk fibroin conduit. Chin J Otorhinolaryngol Head Neck Surg 41(8):603–606 (article in Chinese)
Ma F, Zhu T, Xu F, Wang Z, Zheng Y, Tang Q, Chen L, Shen Y, Zhu J (2017) Neural stem/progenitor cells on collagen with anchored basic fibroblast growth factor as potential natural nerve conduits for facial nerve regeneration. Acta Biomater 50:188–197. doi:10.1016/j.actbio.2016.11.064
Liu H, Wen W, Hu M, Bi W, Chen L, Liu S, Chen P, Tan X (2013) Chitosan conduits combined with nerve growth factor microspheres repair facial nerve defects. Neural Regener Res 8(33):3139–3147. doi:10.3969/j.issn.1673-5374.2013.33.008
Owens CM, Marga F, Forgacs G, Heesch CM (2013) Biofabrication and testing of a fully cellular nerve graft. Biofabrication 5(4):045007. doi:10.1088/1758-5082/5/4/045007
Chang CC, Boland ED, Williams SK, Hoying JB (2011) Direct-write bioprinting three-dimensional biohybrid systems for future regenerative therapies. J Biomed Mater Res B Appl Biomater 98(1):160–170. doi:10.1002/jbm.b.31831
Ozbolat IT, Yu Y (2013) Bioprinting toward organ fabrication: challenges and future trends. IEEE Trans Biomed Eng 60(3):691–699. doi:10.1109/TBME.2013.2243
Acknowledgements
This work was supported by grants from National Natural Science of China (81271094) and the Shanghai Science and Technology Committee (17441901600).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
This article does not involve any studies with human participants or animals performed by any of the authors and therefore no informed consent was required.
Rights and permissions
About this article
Cite this article
Zhong, N., Zhao, X. 3D printing for clinical application in otorhinolaryngology. Eur Arch Otorhinolaryngol 274, 4079–4089 (2017). https://doi.org/10.1007/s00405-017-4743-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4743-0