Abstract
Purpose
New-onset proteinuria, as a pivotal sign of representative renal lesions in preeclampsia, is still the most common diagnostic tool for this condition and has been proven to be related to a significantly abnormal sFlt-1/VEGF ratio in circulation. At the same time, blood pressure control plays a vital role in the occurrence and evolution of proteinuria. Therefore, it is particularly helpful to investigate their interval, not only for performing urinalysis for protein more accurately but also for evaluating blood pressure as well as the aggravation of illness, as the related research is limited.
Methods
This retrospective study included 515 preeclampsia patients and 358 normotensive pregnant women who labored in the Second Hospital of Tianjin Medical University from January 2016 to January 2020. First, we described the onset circumstance of high blood pressure and proteinuria as well as the interval among the case group and the subgroups. Then, we determined whether there were significant differences in the basic information, laboratory test results, and newborns between the case and normal groups. Finally, multifactor ANOVA was used to determine the factors influencing the interval.
Results
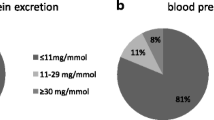
1. The two most common complications in preeclampsia were proteinuria (88.35%) and placental dysfunction (5.05%). Moreover, 72.04% of preeclampsia cases were diagnosed by abnormal blood pressure together with new-onset proteinuria. 2. The average interval between high blood pressure and proteinuria was 22 gestational days (from 0 to 106 days), and this interval was not significantly different between mild and severe PE (26 days vs. 21 days, P > 0.05) but significantly differed between early-onset and late-onset PE (9 days vs. 28 days, P < 0.05). 3. The number of prenatal visits, serum creatinine in the early trimester, gestational time and diastolic blood pressure value when increased blood pressure was initially detected may influence the interval between the onset of increased blood pressure and proteinuria.
Conclusion
New-onset proteinuria was still the main parameter for identifying preeclampsia. The interval between increased blood pressure and proteinuria was probably related to the imbalance in the sFlt-1/VEGF ratio; therefore, we should pay attention to monitor proteinuria during the prenatal visits, especially for patients with a lower frequency of prenatal visits, higher serum creatinine in the early trimester, earlier onset and higher diastolic blood pressure at the initial onset of increased blood pressure.

Similar content being viewed by others
Data availability
In consideration of the privacy policy, the authors will provide the relevant data which support this research in response to reasonable requests.
References
Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R (2014) Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol 8:466–480. https://doi.org/10.1038/nrneph.2014.102
Tay J, Foo L, Masini G, Bennett PR, McEniery CM, Wilkinson IB, Lees CC (2018) Early and late preeclampsia are characterized by high cardiac output, but in the presence of fetal growth restriction, cardiac output is low: insights from a prospective study. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2018.02.007
Avolio A, Kim MO, Adji Am Gangoda S, Avadhanam B, Tan I, Butlin M (2018) Cerebral haemodynamics: effects of systemic arterial pulsatile function and hypertension. Curr Hypertens Rep 3:20. https://doi.org/10.1007/s11906-018-0822-x
de Mendonca ELSS, da Silva JVF, Mello CS, de Oliveira ACM (2022) Serum uric acid levels associated with biochemical parameters linked to preeclampsia severity and to adverse perinatal outcomes. Arch Gynecol Obstet 6:1453–1463. https://doi.org/10.1007/s00404-021-06313-2
Magee LA, Nicolaides KH, von Dadelszen P (2022) Preeclampsia. Obstet Gynecol Surv 11:641–643. https://doi.org/10.1097/01.ogx.0000899472.90847.03
Omani-Samani R, Ranjbaran M, Almasi-Hashiani A (2019) Adverse maternal and neonatal outcomes in women with preeclampsia in Iran. J Matern-Fetal Neonat Med 2:212–216. https://doi.org/10.1080/14767058.2017.1376643
Wetta LA, Szychowski JM, Seals S, Mancuso MS, Biggio JR, Tita ATN (2013) Risk factors for uterine atony/postpartum hemorrhage requiring treatment after vaginal delivery. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2013.03.011
Koike T, Minakami H, Izumi A, Watanabe T, Matsubara S, Sato I (2002) Recurrence risk of preterm birth due to preeclampsia. Gynecol Obstet Invest 1:22–27. https://doi.org/10.1159/000049406
Harskamp RE, Zeeman GG (2007) Preeclampsia: at risk for remote cardiovascular disease. Am J Med Sci 4:291–295. https://doi.org/10.1097/MAJ.0b013e3180a6f094
Roberts JM, Escudero C (2012) The placenta in preeclampsia. Pregnancy Hypertens 2:72–83. https://doi.org/10.1016/j.preghy.2012.01.001
Wright D, Tan MY, O’Gorman N, Poon LC, Syngelaki A, Wright A, Nicolaides KH (2019) Predictive performance of the competing risk model in screening for preeclampsia. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2018.11.1087
LeFevre ML (2014) Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US preventive services task force recommendation statement. Ann Intern Med 11:819-U114. https://doi.org/10.7326/M14-1884
Meertens LJE, Scheepers HCJ, Willemse JPMM, Spaanderman MEA, Smits LJM (2018) Should women be advised to use calcium supplements during pregnancy A decision analysis. Matern Child Nutr. https://doi.org/10.1111/mcn.12479
Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM (2004) Delayed postpartum preeclampsia: An experience of 151 cases. Am J Obstet Gynecol 5:1464–1466. https://doi.org/10.1016/j.ajog.2004.02.037
Robillard PY, Dekker G, Iacobelli S, Chaouat G (2016) An essay of reflection: why does preeclampsia exist in humans, and why are there such huge geographical differences in epidemiology? J Reprod Immunol 114:44–47. https://doi.org/10.1016/j.jri.2015.07.001
Ren J, Fan ZR, Li J, Wang YJ, Zhang JN (2023) Hua SF (2023) Blood pressure patterns of hypertensive disorders of pregnancy in first and second trimester and contributing factors: a retrospective study. J Obstet Gynaecol. https://doi.org/10.1080/01443615.2023.2171776
Kattah A (2020) Preeclampsia and kidney disease: deciphering cause and effect. Curr Hypertens Rep. https://doi.org/10.1007/s11906-020-01099-1
Bartal MF, Lindheimer MD, Sibai BM (2022) Proteinuria during pregnancy: definition, pathophysiology, methodology, and clinical significance. Am J Obstet Gynecol 2:S819–S834. https://doi.org/10.1016/j.ajog.2020.08.108
Peterson JC, Adler S, Burkart JM, Greene T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG, Seifter JL (1995) Blood-pressure control, proteinuria, and the progression of renal-disease-The modification of diet in renal-disease study. Ann Intern Med. https://doi.org/10.7326/0003-4819-123-10-199511150-00003
Khedun SM, Naicker T, Moodley J (2000) Relationship between histopathological changes in post partum renal biopsies and renal function tests of African women with early onset pre-eclampsia. Acta Obstet Gynecol Scand 5:350–354. https://doi.org/10.1034/j.1600-0412.2000.079005350.x
Onda K, Tong S, Beard S, Binder N, Muto M, Senadheera SN, Parry L, Dilworth M, Renshall L, Brownfoot F, Hastie R, Tuohey L, Palmer K, Hirano T, Ikawa M, Kaitu’u-Lino T, Hannan NJ (2017) Proton pump inhibitors decrease soluble fms-like tyrosine kinase-1 and soluble endoglin secretion, decrease hypertension and rescue endothelial dysfunction. Hypertension. https://doi.org/10.1161/HYPERTENSIONAHA.116.08408
Lariviere R, Lebel M (2003) Endothelin-1 in chronic renal failure and hypertension. Can J Physiol Pharmacol 6:607–621. https://doi.org/10.1139/Y03-012
Caruso-Neves C, Pinheiro AAS, Cai H, Souza-Menezes J, Guggino WB (2006) PKB and megalin determine the survival or death of renal proximal tubule cells. Proc Natl Acad Sci U S A 49:18810–18815. https://doi.org/10.1073/pnas.0605029103
Prakash J, Ganiger VC, Prakash S, Iqbal M, Kar DP, Singh U, Verma A (2018) Acute kidney injury in pregnancy with special reference to pregnancy-specific disorders: a hospital based study (2014–2016). J Nephrol 1:79–85. https://doi.org/10.1007/s40620-017-0466-y
Yu DH, Petermann A, Kunter U, Rong S, Shankland SJ, Floege J (2005) Urinary podocyte loss is a more specific marker of ongoing glomerular damage than proteinuria. J Am Soc Nephrol 6:1733–1741. https://doi.org/10.1681/ASN.2005020159
Murakami S, Saitoh M, Kubo T, Koyama T, Kobayashi M (2000) Renal disease in women with severe preeclampsia or gestational proteinuria. Obstet Gynecol 6:945–949. https://doi.org/10.1016/S0029-7844(00)01055-3
Wang IK, Muo CH, Chang YC, Liang CC, Chang CT, Lin SY, Yen TH, Chuang FR, Chen PC, Huang CC, Wen CP, Sung FC, Morisky DE (2013) Association between hypertensive disorders during pregnancy and end-stage renal disease: a population-based study. Can Med Assoc J 3:207–213. https://doi.org/10.1503/cmaj.120230
Magee LA, Brown MA, Hall DR, Gupte S, Hennessy A, Karumanchi SA, Kenny LC, McCarthy F, Myers J, Poon LC, Rana S, Saito S, Staff AC, Tsigas E, von Dadelszen P (2022) The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis and management recommendations for international practice. Pregnancy Hypertens 27:148–169. https://doi.org/10.1016/j.preghy.2021.09.008
Sibai BM (2003) Diagnosis and management of gestational hypertension and Preeclampsia. Obstet Gynecol 1:181–192. https://doi.org/10.1016/S0029-7844(03)00475-7
Jelena MS, Miljanv K, Dragana RJ, Milan S, Vladimir A, Ivana D (2016) Preeclampsia with and without intrauterine growth restriction-Two pathogenetically different entities? Pregnancy Hypertens 4:573–582. https://doi.org/10.1080/10641955.2016.1212872
Hauth JC, Ewell MG, Levine RJ, Esterlitz JR, Sibai B, Curet LB, Catalano PM, Morris CD (2000) Pregnancy outcomes in healthy nulliparas who developed hypertension. Obstet Gynecol. https://doi.org/10.1016/S0029-7844(99)00462-7
Nischintha S, Pallavee P, Seetesh G (2014) Correlation between 24-h urine protein, spot urine protein/creatinine ratio, and serum uric acid and their association with fetomaternal outcomes in preeclamptic women. J Nat Sci Biol Med 2:255–260. https://doi.org/10.4103/0976-9668.136151
Mol BJ, Roberts CT, Thangaratinam S, Magee LA, de Groot CJM, Hofmeyr GJ (2016) Pre-eclampsia. Lancet. https://doi.org/10.1016/S0140-6736(15)00070-7
Turner RJ, Bloemenkamp KWM, Penning ME, Bruijn JA, Baelde HJ (2015) From glomerular endothelium to Podocyte pathobiology in preeclampsia: a paradigm shift. Curr Hypertens Rep. https://doi.org/10.1007/s11906-015-0566-9
Wang LY, Zhang TE, Fang M, Shen N, Wang DP, Teng JQ, Fu B, Xie H, Hong Q, Lin HL (2015) Podocytes protect glomerular endothelial cells from hypoxic injury via deSUMOylation of HIF-1 alpha signaling. Int J Biochem Cell Biol 58:17–27. https://doi.org/10.1016/j.biocel.2014.10.030
Fogo AB, Kon V (2010) The glomerulus - a view from the inside - the endothelial cell. Int J Biochem Cell Biol 9:1388–1397. https://doi.org/10.1016/j.biocel.2010.05.015
Ferrazzani S, Caruso A, Decarolis S, Martino IV, Mancuso S (1990) Proteinuria and outcome of 444 Pregnancies complicated by hypertension. Am J Obstet Gynecol 2:366–371. https://doi.org/10.1016/0002-9378(90)90387-M
Cravedi P, Ruggenenti P, Remuzzi G (2012) Proteinuria should be used as a surrogate in CKD. Nat Rev Nephrol 5:301–306. https://doi.org/10.1038/nrneph.2012.42
Higby K, Suiter CR, Phelps JY, Silerkhodr T, Langer O (1994) Normal values of urinary albumin and total protein excretion during pregnancy. Am J Obstet Gynecol 4:984–989. https://doi.org/10.1016/S0002-9378(13)90019-3
Heim A, Pasche A, Feihl F, Liaudet L, Waeber B (2007) Hypertension: early detection of target organ damage. Rev Med Suisse 124(1996):1999–2002 ((In French))
Payne BA, Hutcheon JA, Ansermino JM, Hall DR, Bhutta ZA, Bhutta SZ, Biryabarema C, Grobman WA, Groen H, Haniff F, Li J, Magee LA, Merialdi M, Nakimuli A, Qu ZG, Sikandar R, Sass N, Sawchuck D, Steyn DW, Widmer M, Zhou J, von Dadelszen P (2014) A risk prediction model for the assessment and triage of women with hypertensive disorders of pregnancy in low-resourced settings: the miniPIERS (Pre-eclampsia Integrated Estimate of RiSk) multi-country prospective cohort study. PLoS Med. https://doi.org/10.1371/journal.pmed.1001589
Buchbinder A, Sibai BM, Caritis S, MacPherson C, Hauth J, Lindheimer MD, Klebanoff M, VanDorsten P, Landon M, Paul R, Miodovnik M, Meis P, Thurnau G (2002) Adverse perinatal outcomes are significantly higher in severe gestational hypertension than in mild preeclampsia. Am J Obstet Gynecol 1:66–71. https://doi.org/10.1067/mob.2002.120080
Barton JR, O’Brien JM, Bergauer NK, Jacques DL, Sibai BM (2001) Mild gestational hypertension remote from term: Progression and outcome. Am J Obstet Gynecol 5:979–983. https://doi.org/10.1067/mob.2001.112905
Lindheimer MD, Kanter D (2010) Interpreting abnormal proteinuria in pregnancy the need for a more pathophysiological approach. Obstet Gynecol 2:365–375. https://doi.org/10.1097/AOG.0b013e3181cb9644
Airoldi J, Weinstein L (2007) Clinical significance of proteinuria in pregnancy. Obstet Gynecol Surv 2:117–124. https://doi.org/10.1097/01.ogx.0000253301.55009.ac
Piccoli GB, Daidola G, Attini R, Parisi S, Fassio F, Naretto C, Deagostini MC, Castelluccia N, Ferraresi M, Roccatello D, Todros T (2013) Kidney biopsy in pregnancy: evidence for counselling? a systematic narrative review. Br J Obstet Gynaecol 4:412–427. https://doi.org/10.1111/1471-0528.12111
Ekiz A, Kaya B, Polat I, Avci ME, Ozkose B, Caliskan RK, Yildirim G (2016) The outcome of pregnancy with new onset proteinuria without hypertension: retrospective observational study. J Matern-Fetal Neonat Med 11:1765–1769. https://doi.org/10.3109/14767058.2015.1061497
Sibai BM, Barton JR (2007) Expectant management of severe preeclampsia remote from term: patient selection, management, and delivery indications. Am J Obstet Gynecol 6:514–516. https://doi.org/10.1016/j.ajog.2007.02.021
Zeisler H, Llurba E, Chantraine FJ, Vatish M, Staff AC, Sennstrom M, Olovsson M, Brennecke SP, Stepan H, Allegranza D, Schoedl M, Grill S, Hund M, Verlohren S (2019) Soluble fms-like tyrosine kinase-1 to placental growth factor ratio: ruling out pre-eclampsia for up to 4 weeks and value of retesting. Ultrasound Obstet Gynecol 3:367–375. https://doi.org/10.1002/uog.19178
Masini G, Foo LF, Tay J, Wilkinson IB, Valensise H, Gyselaers W, Lees CC (2022) Reply: preeclampsia has 2 phenotypes that require different treatment strategies. Am J Obstet Gynecol 1:114–115. https://doi.org/10.1016/j.ajog.2021.09.006
Burton GJ, Redman CW, Roberts JM, Moffett A (2019) Pre-eclampsia: pathophysiology and clinical implications. BMJ (Br Med J). https://doi.org/10.1136/bmj.l2381
Sohlberg S, Mulic-Lutvica A, Lindgren R, Ortiz-Nieto F, Wikstrom AK, Wikstrom J (2014) Placental perfusion in normal pregnancy and early and late preeclampsia: a magnetic resonance imaging study. Placenta 3:202–206. https://doi.org/10.1016/j.placenta.2014.01.008
Valensise H, Vasapollo B, Gagliardi G, Novelli GP (2008) Early and late preeclampsia two different maternal hemodynamic states in the latent phase of the disease. Hypertension 5:873–880. https://doi.org/10.1161/HYPERTENSIONAHA.108.117358
Todd N, McNally R, Alqudah A, Jerotic D, Suvakov S, Obradovic D, Hoch D, Hombrebueno JR, Campos GL, Watson CJ, Gojnic-Dugalic M, Simic TP, Krasnodembskaya A, Desoye G, Eastwood KA, Hunter AJ, Holmes VA, McCance DR, Young IS, Grieve DJ, Kenny LC, Garovic VD, Robson T, McClements L (2021) Role of a novel angiogenesis FKBPL-CD44 pathway in preeclampsia risk stratification and mesenchymal stem cell treatment. J Clin Endocrinol Metab 1:26–41. https://doi.org/10.1210/clinem/dgaa403
Orgul G, Hakli DA, Ozten G, Fadiloglu E, Tanacan A, Beksac MS (2019) First trimester complete blood cell indices in early and late onset preeclampsia. Turk J Obstet Gynaecol 2:112–117. https://doi.org/10.4274/tjod.galenos.2019.93708
Nizyaeva NV, Kulikova GV, Nagovitsyna MN, Shchegolev AI (2019) Peculiarities of the expression of TLR4 and inhibitor of TLR-cascade tollip in the placenta in earlyand late-onset preeclampsia. Bull Exp Biol Med 4:507–511. https://doi.org/10.1007/s10517-019-04383-6
Banadakoppa M, Vidaeff AC, Yallampalli U, Ramin SM, Belfort MA, Yallampalli C (2015) Complement split products in amniotic fluid in pregnancies subsequently developing early-onset preeclampsia. Dis Markers. https://doi.org/10.1155/2015/263109
Weissgerber TL, Garcia-Valencia O, Milic NM, Codsi E, Cubro H, Nath MC, White WM, Nath KA, Garovic VD (2019) Early onset preeclampsia is associated with glycocalyx degradation and reduced microvascular perfusion. J Am Heart Assoc. https://doi.org/10.1161/JAHA.118.010647
James MT, Bhatt M, Pannu N, Tonelli M (2020) Long-term outcomes of acute kidney injury and strategies for improved care. Nat Rev Nephrol 4:193–205. https://doi.org/10.1038/s41581-019-0247-z
Saleh MA, Pollock DM (2011) Endothelin in renal inflammation and hypertension. Karger, Switzerland
van Balen VAL, Spaan JJ, Cornelis T, Spaanderman MEA (2017) Prevalence of chronic kidney disease after preeclampsia. J Nephrol 3:403–409. https://doi.org/10.1007/s40620-016-0342-1
Acknowledgements
This research was supported by the Science and Technology Project of Tianjin Health Commission. (No. ZC20057)
Funding
This research was supported by the Science and Technology Project of Tianjin Health Commission (No. ZC20057).
Author information
Authors and Affiliations
Contributions
JR: Project development, Data Collection, Manuscript writing, CZ: Manuscript writing, ZF: Data Collection, Data analysis, YW: Data Collection, HS: Manuscript editing, SH: Project development, All authors contributed to the study conception and design. In addition, all authors have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare they have no financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ren, J., Zhao, C., Fan, Z. et al. The interval between the onset of increased blood pressure and proteinuria in preeclampsia and the contributing factors. Arch Gynecol Obstet (2023). https://doi.org/10.1007/s00404-023-07284-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-023-07284-2