Abstract
Purpose
This study aimed to explore the association between vaginal microbiota and infertility.
Methods
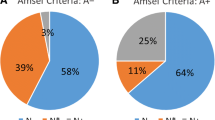
We searched a range of electronic databases for appropriate articles, including PubMed, Web of Science, Embase, Chinese National Knowledge Infrastructure (CNKI), and Wanfang, from inception to 8th September 2019. Identified articles were then screened using strict inclusion and exclusion criteria. By referring to Tamarelle’s method, we divided vaginal microbiota into two categories: low-Lactobacillus vaginal microbiota (LL-VMB) and high-Lactobacillus vaginal microbiota (HL-VMB). Patients were defined as HL-VMB if they had a Nugent score of 0–3, a negative Amesel/Spiegel’s test, or if the vaginal community status was dominated by either L. crispatus, L. iners, L. gasseri and L. jensenii via 16S rRNA sequencing. Otherwise, cases were regarded as LL-VMB. Statistical analyses were performed with STATA 13.0 statistical software. Effect estimates are presented as odds ratios (ORs) with 95% confidence intervals (CIs).
Results
Fifteen articles were included in our final analysis. The HL-VMB was negatively related to infertility; a fixed model showed that the pooled OR was 0.83 (95% CI 0.77–0.90). There was no significant publication bias, as determined by Begg’s test (P = 0.488) and Egger’s test (P = 0.652). Using a random effect model, the pooled OR for intermediate bacterial vaginitis (BV) and infertility was 1.39 (95% CI 1.10–1.76) and the pooled OR for positive BV was 1.72 (95% CI 1.10–2.69). Subgroup and sensitivity analyses further demonstrated that the associations identified were stable. However, the acquired evidence was not sufficient to make inferences with regards to the mechanisms underlying these relationships.
Conclusion
This systematic review and meta-analysis identified a negative correlation between HL-VMB and female infertility. However, due to a variety of limitations, the evidence acquired does not allow us to identify the specific mechanisms underlying this association. Further high-quality studies are needed to verify the causal relationship and explore the molecular mechanisms involved.




Similar content being viewed by others
Abbreviations
- BV:
-
Bacterial vaginitis
- CI:
-
Confidence interval
- CST:
-
Community status type
- HL-VMB:
-
High-Lactobacillus vaginal microbiota
- LL-VMB:
-
Low-Lactobacillus vaginal microbiota
- NGS:
-
Next-generation sequencing
- OR:
-
Odds ratio
- PCOS:
-
Polycystic ovary syndrome
- PID:
-
Pelvic inflammatory disease
- STI:
-
Sexually transmitted infections
References
Inhorn MC, Patrizio P (2015) Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update 21(4):411–426. https://doi.org/10.1093/humupd/dmv016
Vander Borght M, Wyns C (2018) Fertility and infertility: definition and epidemiology. Clin Biochem 62:2–10. https://doi.org/10.1016/j.clinbiochem.2018.03.012
Crawford NM, Steiner AZ (2015) Age-related infertility. Obstet Gynecol Clin N Am 42(1):15–25. https://doi.org/10.1016/j.ogc.2014.09.005
Mol BW, Tjon-Kon-Fat R, Kamphuis E, van Wely M (2018) Unexplained infertility: Is it over-diagnosed and over-treated? Best Pract Res Clin obstet Gynaecol 53:20–29. https://doi.org/10.1016/j.bpobgyn.2018.09.006
Ahmadi MH, Mirsalehian A, Bahador A (2016) Association of Chlamydia trachomatis with infertility and clinical manifestations: a systematic review and meta-analysis of case-control studies. Infection Dis 48(7):517–523. https://doi.org/10.3109/23744235.2016.1160421
Tsevat DG, Wiesenfeld HC, Parks C, Peipert JF (2017) Sexually transmitted diseases and infertility. Am J Obstet Gynecol 216(1):1–9. https://doi.org/10.1016/j.ajog.2016.08.008
Huang B, Fettweis JM, Brooks JP, Jefferson KK, Buck GA (2014) The changing landscape of the vaginal microbiome. Clin Lab Med 34(4):747–761. https://doi.org/10.1016/j.cll.2014.08.006
Spiegel CA, Amsel R, Holmes KK (1983) Diagnosis of bacterial vaginosis by direct gram stain of vaginal fluid. J Clin Microbiol 18(1):170–177
Nugent RP, Krohn MA, Hillier SL (1991) Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol 29(2):297–301
Amsel R, Totten PA, Spiegel CA, Chen KCS, Eschenbach DA, Holmes KK (1983) Nonspecific vaginitis: diagnostic criteria and microbial and epidemiologic associations☆. Am J Med 74(1):14–22
van Oostrum N, De Sutter P, Meys J, Verstraelen H (2013) Risks associated with bacterial vaginosis in infertility patients: a systematic review and meta-analysis. Hum Reprod (Oxford, England) 28(7):1809–1815. https://doi.org/10.1093/humrep/det096
Petrova MI, Reid G, Vaneechoutte M, Lebeer S (2017) Lactobacillus iners: friend or foe? Trends Microbiol 25(3):182–191. https://doi.org/10.1016/j.tim.2016.11.007
Lewis FM, Bernstein KT, Aral SO (2017) Vaginal microbiome and its relationship to behavior, sexual health, and sexually transmitted diseases. Obstet Gynecol 129(4):643–654. https://doi.org/10.1097/aog.0000000000001932
Campisciano G, Florian F, D'Eustacchio A, Stanković D, Ricci G, De Seta F, Comar M (2017) Subclinical alteration of the cervical–vaginal microbiome in women with idiopathic infertility. J Cell Physiol 232(7):1681–1688. https://doi.org/10.1002/jcp.25806
Tamarelle J, Thiebaut ACM, de Barbeyrac B, Bebear C, Ravel J, Delarocque-Astagneau E (2019) The vaginal microbiota and its association with human papillomavirus, Chlamydia trachomatis, Neisseria gonorrhoeae and Mycoplasma genitalium infections: a systematic review and meta-analysis. Clin Microbiol Infect 25(1):35–47. https://doi.org/10.1016/j.cmi.2018.04.019
Liberati A, Altman DG, Tetzlaff J, Mulrow CD, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 6(7):354–391
Hardy RJ, Thompson SG (1998) Detecting and describing heterogeneity in meta-analysis. Stat Med 17(8):841–856. https://doi.org/10.1002/(sici)1097-0258(19980430)17:8<841:aid-sim781>3.0.co;2-d
Morgan DJ, Wong SJ, Trueman G, Priddy A, Lamont RF, Kapembwa MS, Taylorrobinson D (1997) Can bacterial vaginosis influence fertility? Its increased prevalence in a subfertile population. Int J STD AIDS 8:19–20
Mania-Pramanik J, Kerkar SC, Salvi VS (2009) Bacterial vaginosis: a cause of infertility? Int J STD AIDS 20(11):778–781. https://doi.org/10.1258/ijsa.2009.009193
Adamson PC, Krupp K, Freeman AH, Klausner JD, Reingold AL, Madhivanan P (2011) Prevalence & correlates of primary infertility among young women in Mysore, India. Indian J Med Res 134:440–446
Xu Y, Zhang L, Chen F (2011) Analysis of vaginal microbial communities in 300 infertility women. Chin J Hum Sex 20(4):4–6. https://doi.org/10.3969/j.issn.1672-1993.2011.04.002
Salah RM, Allam AM, Magdy AM, Mohamed A (2013) Bacterial vaginosis and infertility: cause or association? Eur J Obstet Gynecol Reprod Biol 167(1):59–63. https://doi.org/10.1016/j.ejogrb.2012.10.031
Tomusiak A, Heczko PB, Janeczko J, Adamski P, Pilarczyk-Zurek M, Strus M (2013) Bacterial infections of the lower genital tract in fertile and infertile women from the southeastern Poland. Ginekol Pol 84(5):352–358
Durugbo II, Nyengidiki TK, Bassey G, Wariso KT (2015) Bacterial vaginosis among women with tubal factor infertility in Nigeria. Int J Gynecol Obstet 131(2):133–136. https://doi.org/10.1016/j.ijgo.2015.05.031
Qin X, Sun C (2016) Analysis of vaginal microflora and micro ecological condition in infertility female. Chin J Hum Sex 25(8):88–90
Zheng Y, Liu X, Liu Z (2016) Vaginal micro-ecological analysis of 560 cases of infertile women in Zhengzhou. Chin J Health Lab Technol 26(9):1294–1296
Babu G, Singaravelu BG, Srikumar R, Reddy SV, Kokan A (2017) Comparative study on the vaginal flora and incidence of asymptomatic vaginosis among healthy women and in women with infertility problems of reproductive age. J Clin Diagn Res 11(8):DC18–DC22. https://doi.org/10.7860/jcdr/2017/28296.10417
Kyono K, Hashimoto T, Nagai Y, Sakuraba Y (2018) Analysis of endometrial microbiota by 16S ribosomal RNA gene sequencing among infertile patients: a single-center pilot study. Reprod Med Biol 17(3):297–306. https://doi.org/10.1002/rmb2.12105
Wee BA, Thomas M, Sweeney EL, Frentiu FD, Samios M, Ravel J, Gajer P, Myers G, Timms P, Allan JA, Huston WM (2018) A retrospective pilot study to determine whether the reproductive tract microbiota differs between women with a history of infertility and fertile women. Aust N Z J Obstet Gynaecol 58(3):341–348. https://doi.org/10.1111/ajo.12754
Yang L, Chen R (2018) Microflora in female reproductive tract of women with tubal infertility. Chin J Microecol 30(12):1452–1455. https://doi.org/10.13381/j.cnki.cjm.201812020
Liu Y (2019) Study on the vaginal microecosystem in 220 patients with infertility. Chin J Hum Sex 28(8):107–110
Moragianni D, Dryllis G, Andromidas P, Kapeta-Korkouli R, Kouskouni E, Pessach I, Papalexis P, Kodonaki A, Athanasiou N, Pouliakis A, Baka S (2019) Genital tract infection and associated factors affect the reproductive outcome in fertile females and females undergoing in vitro fertilization. Biomed Rep 10(4):231–237. https://doi.org/10.3892/br.2019.1194
Garcia-Velasco JA, Menabrito M, Catalan IB (2017) What fertility specialists should know about the vaginal microbiome: a review. Reprod Biomed Online 35(1):103–112. https://doi.org/10.1016/j.rbmo.2017.04.005
Graspeuntner S, Bohlmann MK, Gillmann K, Speer R, Kuenzel S, Mark H, Hoellen F, Lettau R, Griesinger G, Konig IR, Baines JF, Rupp J (2018) Microbiota-based analysis reveals specific bacterial traits and a novel strategy for the diagnosis of infectious infertility. PLoS ONE 13(1):e0191047. https://doi.org/10.1371/journal.pone.0191047
Linhares IM, Witkin SS (2010) Immunopathogenic consequences of Chlamydia trachomatis 60 kDa heat shock protein expression in the female reproductive tract. Cell Stress Chaperones 15(5):467–473. https://doi.org/10.1007/s12192-010-0171-4
Taylor BD, Darville T, Haggerty CL (2013) Does bacterial vaginosis cause pelvic inflammatory disease? Sex Transm Dis 40(2):117–122. https://doi.org/10.1097/OLQ.0b013e31827c5a5b
Wiesenfeld HC, Hillier SL, Meyn LA, Amortegui AJ, Sweet RL (2012) Subclinical pelvic inflammatory disease and infertility. Obstet Gynecol 120(1):37–43. https://doi.org/10.1097/AOG.0b013e31825a6bc9
Chen C, Song X, Wei W, Zhong H, Dai J, Lan Z, Li F, Yu X, Feng Q, Wang Z, Xie H, Chen X, Zeng C, Wen B, Zeng L, Du H, Tang H, Xu C, Xia Y, Xia H, Yang H, Wang J, Wang J, Madsen L, Brix S, Kristiansen K, Xu X, Li J, Wu R, Jia H (2017) The microbiota continuum along the female reproductive tract and its relation to uterine-related diseases. Nature Commun 8(1):875. https://doi.org/10.1038/s41467-017-00901-0
Alcaide ML, Rodriguez VJ, Brown MR, Pallikkuth S, Arheart K, Martinez O, Roach M, Fichorova RN, Jones DL, Pahwa S, Fischl MA (2017) High levels of inflammatory cytokines in the reproductive tract of women with BV and engaging in intravaginal douching: a cross-sectional study of participants in the women interagency HIV study. AIDS Res Hum Retroviruses 33(4):309–317. https://doi.org/10.1089/aid.2016.0187
Barthelmess EK, Naz RK (2014) Polycystic ovary syndrome: current status and future perspective. Front Biosci 6:104–119
Muhleisen AL, Herbst-Kralovetz MM (2016) Menopause and the vaginal microbiome. Maturitas 91:42–50. https://doi.org/10.1016/j.maturitas.2016.05.015
Lindheim L, Bashir M, Munzker J, Trummer C, Zachhuber V, Leber B, Horvath A, Pieber TR, Gorkiewicz G, Stadlbauer V, Obermayer-Pietsch B (2017) Alterations in gut microbiome composition and barrier function are associated with reproductive and metabolic defects in women with polycystic ovary syndrome (PCOS): a pilot study. PLoS ONE 12(1):e0168390. https://doi.org/10.1371/journal.pone.0168390
Zhao J, Hong X, Zhang H, Dai Q, Huang K, Zhang X, Liu Y, Wu J, Wang Q, Shen H, Xu Z, Zhang Y, Yan D, Qi D, Yang X, Zhang Y, Wang B, Ma X (2019) Pre-pregnancy maternal fasting plasma glucose levels in relation to time to pregnancy among the couples attempting first pregnancy. Hum Reprod (Oxford, England) 34(7):1325–1333. https://doi.org/10.1093/humrep/dez069
Kalra B, Kalra S (2017) Vulvovaginitis and diabetes. JPMA J Pakistan Med Assoc 67(1):143–145
Nguyen RH, Wilcox AJ (2005) Terms in reproductive and perinatal epidemiology: I. Reproductive terms. J Epidemiol Community Health 59(11):916–919. https://doi.org/10.1136/jech.2004.023457
Hong X, Zhao J, Huang K, Dai Q, Zhang H, Xuan Y, Wu J, Fang S, Wang Q, Shen H, Xu Z, Zhang Y, Yan D, Qi D, Yang X, Zhang Y, Ma X, Wang B (2019) Preconception blood pressure and time to pregnancy among couples attempting to conceive their first pregnancy. Am J Obstet Gynecol 221(5):470.e471–470.e410. https://doi.org/10.1016/j.ajog.2019.05.038
Ernster VL (1994) Nested case-control studies. Prev Med 23(5):587–590. https://doi.org/10.1006/pmed.1994.1093
Rizzo R, Lo Monte G, Bortolotti D, Graziano A, Gentili V, Di Luca D, Marci R (2015) Impact of soluble HLA-G levels and endometrial NK cells in uterine flushing samples from primary and secondary unexplained infertile women. Int J Mol Sci 16(3):5510–5516. https://doi.org/10.3390/ijms16035510
MacIntyre DA, Chandiramani M, Lee YS, Kindinger L, Smith A, Angelopoulos N, Lehne B, Arulkumaran S, Brown R, Teoh TG, Holmes E, Nicoholson JK, Marchesi JR, Bennett PR (2015) The vaginal microbiome during pregnancy and the postpartum period in a European population. Sci Rep 5:8988. https://doi.org/10.1038/srep08988
Verstraelen H, Verhelst R, Claeys G, De Backer E, Temmerman M, Vaneechoutte M (2009) Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol 9:116. https://doi.org/10.1186/1471-2180-9-116
Gajer P, Brotman RM, Bai G, Sakamoto J, Schutte UM, Zhong X, Koenig SS, Fu L, Ma ZS, Zhou X, Abdo Z, Forney LJ, Ravel J (2012) Temporal dynamics of the human vaginal microbiota. Sci Transl Med 4(132):132ra152. https://doi.org/10.1126/scitranslmed.3003605
Funding
This work was supported by National Natural Science Foundation of China (Grant no. 81872634) and Scientific Research Foundation of Graduate School of Southeast University (Grant no. YBPY1983).
Author information
Authors and Affiliations
Contributions
Literature search and screening: XH, JM, JY and BW; data extraction: XH, JY, JG and BW; data analysis: XH, HZ, MZ and XZ; results visualization: XH, MY and YX; manuscript draft and modification: XH, S.F, JM and BW; funding acquirement: BW. All authors reviewed the final version of the manuscript and approve it for publication.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Data sharing statement
More original data can be obtained from Prof. Wang: wangbeilxb@163.com.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hong, X., Ma, J., Yin, J. et al. The association between vaginal microbiota and female infertility: a systematic review and meta-analysis. Arch Gynecol Obstet 302, 569–578 (2020). https://doi.org/10.1007/s00404-020-05675-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05675-3